- Department of Neurosurgery, Hospital Santa Maria, Centro Hospitalar Lisboa Norte, Portugal
- Radiology Unit, Centro Hospitalar Lisboa Central, Lisboa, Portugal.
Correspondence Address:
Samuel Sequeira Lemos, Department of Neurosurgery, Hospital Santa Maria, Lisboa, Portugal.
DOI:10.25259/SNI_685_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Samuel Sequeira Lemos1, Diogo Belo1, Filipe Veloso Gomes2. Giant sacral aneurysmal bone cyst treated with endovascular embolization. 20-Oct-2023;14:373
How to cite this URL: Samuel Sequeira Lemos1, Diogo Belo1, Filipe Veloso Gomes2. Giant sacral aneurysmal bone cyst treated with endovascular embolization. 20-Oct-2023;14:373. Available from: https://surgicalneurologyint.com/surgicalint-articles/12603/
Abstract
Background: Spine aneurysmal bone cysts (SABC) are osteolytic tumor-like lesions with cystic, blood-filled cavities that represent 15% of all primary spinal bone tumors. The sacrum is a rare site for SABC, and sacral lesions typically carry higher morbidity rates. Here, a 19-year-old female with a large primary multisegmental sacral SABC was successfully managed with 2-staged endovascular embolization.
Case Description: A 19-year-old female presented with progressive worsening of axial lumbosacral pain, and a left L5/S1 radiculopathy. The lumbosacral computed tomography and magnetic resonance studies showed a large (10 cm [AP] × 11 cm [Tr] × 12 cm [CC]) heterogeneous, osteolytic lesion containing multiple fluid-fluid levels. The biopsy confirmed the diagnosis of a primary SABC. She was treated with a 2-staged endovascular embolization that resolved her pain. This was followed by radiographic confirmation of occlusion of the SABC.
Conclusion: A 19-year-old female presented with an atypical SABC that was successfully managed with 2-staged endovascular embolization.
Keywords: Embolization, Endovascular treatment, Sacral aneurysmal bone cyst, Spine
INTRODUCTION
Most spine aneurysmal bone cysts (SABC) occur in patients under 20 years of age. They typically present with focal pain and neurological deficits reflecting their locations. SABC represent 15% of all primary bone spine tumors, and only rarely involve the sacrum (i.e., 3%).[
CASE DESCRIPTION
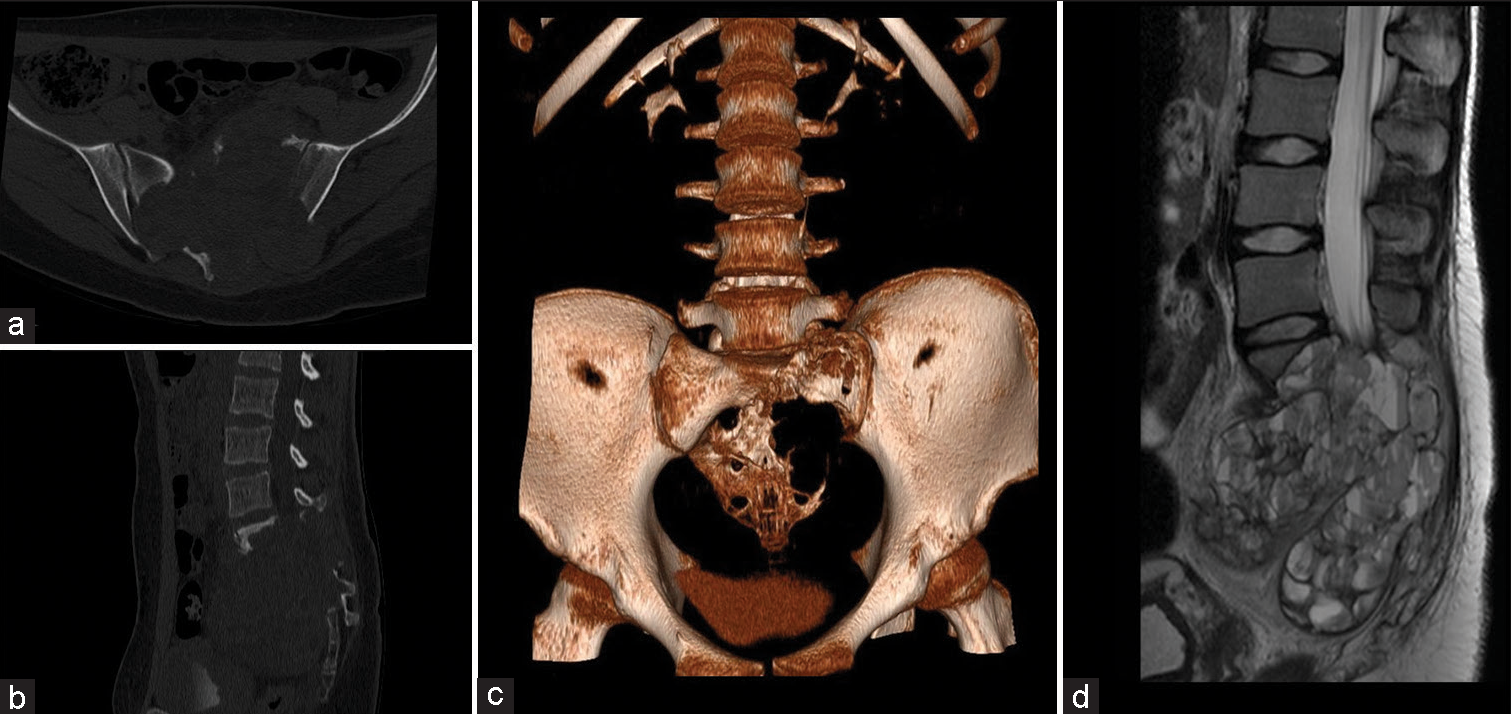
A 19-year-old female presented 6 months of worsening, nocturnal, lumbosacral and left-sided L5/S1 pain, and weakness. The CT scan showed an extensive (i.e., 10 cm [AP] × 11 cm [Tr] × 12 cm [CC]) heterogeneous lytic lesion containing multiple cysts with fluid levels in the sacrum with attendant cortical destruction and invasion of the sacral canal. The lesion extended anteriorly to the sacrum into the pelvic cavity (i.e., with ill-defined borders), laterally into the iliac bones, superiorly into the L5 vertebral body, and inferiorly into S4 [
Figure 1:
(a) Computed tomography (CT) axial view, (b) sagittal view, and (c) 3D reconstruction showing an extensive sacral lytic lesion extending to the iliac bones. (d) T2 magnetic resonance imaging(MRI) sagittal view showing multiple cystic cavities with fluid levels extending into the sacral canal and peritoneal cavity.
Biopsy and pathology
Percutaneous biopsies performed at multiple lesion locations yielded the diagnosis of a primary SABC (i.e., typical histological pattern for ABC and with no precursor lesion identified).
Two-Stage endovascular embolization
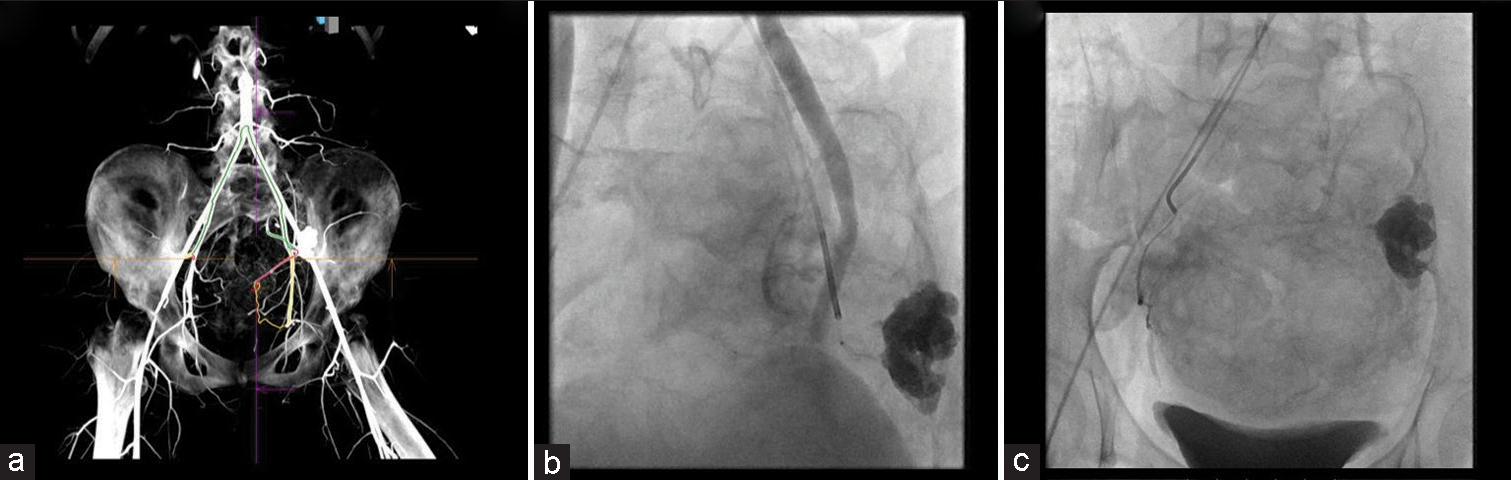
Digital subtraction angiography of the infrarenal aorta identified feeders from the posterior rami of both internal iliac arteries, (i.e., mainly from the left) [
Figure 2:
(a) Intra-Arterial computerized tomography (CT) with 3D reconstruction identifying culprit arterial branches. (b) Digital subtraction angiography (DSA) showing catheter and microcatheter tip with stasis in one of the arterial branches. Gross calcification of the aneurysmal bone cysts (ABC) is seen on the left. (c) DSA showing a branch from the right internal iliac artery which was super selectively catheterized and embolized with polyvinyl alcohol particles ( PVA) particles.
Postoperative course
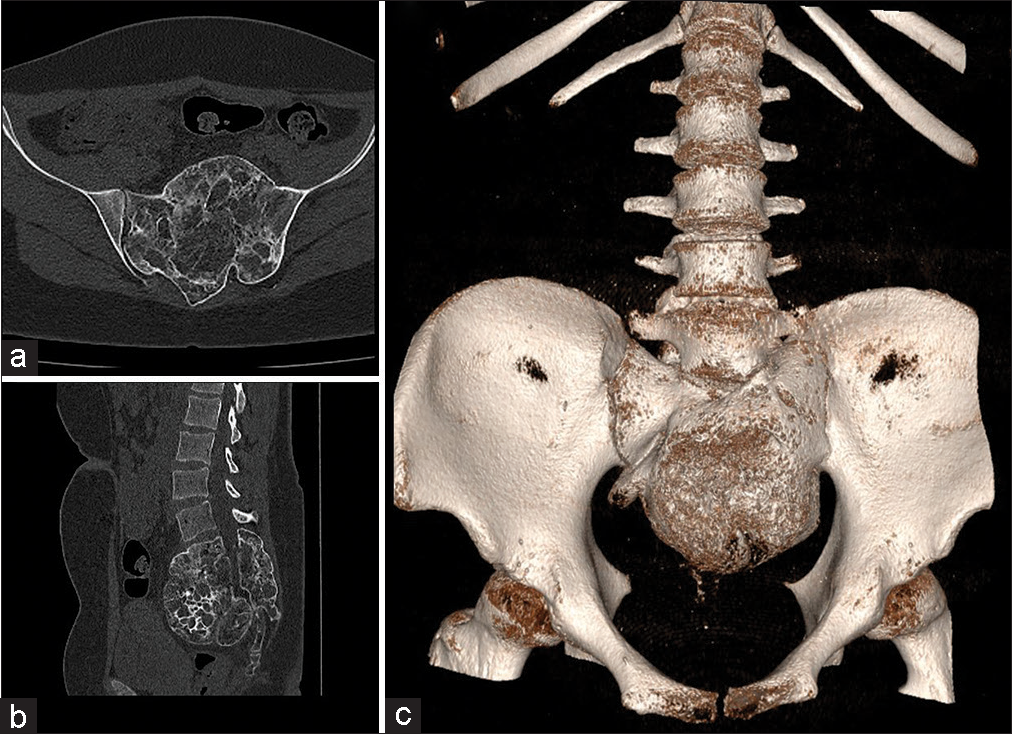
Postoperatively, although the left-sided L5/S1 motor deficit remained, the patient’s pain significantly improved. Multiple follow-up CT exams obtained up to 2 years later showed progressive healing, (i.e., bone formation within the ABC and peripheral sclerotic bony changes) [
DISCUSSION
Here, a 19-year-old female demonstrated L5/S1 pain, and motor deficits attributed to a sacral SABC (i.e., L5–S4 with a total volume of 680 cm3). This SABC extended into the iliac bones, sacral canal, and peritoneal cavity (i.e., Enneking type 3 lesion with an aggressive invasion of adjacent tissues).[
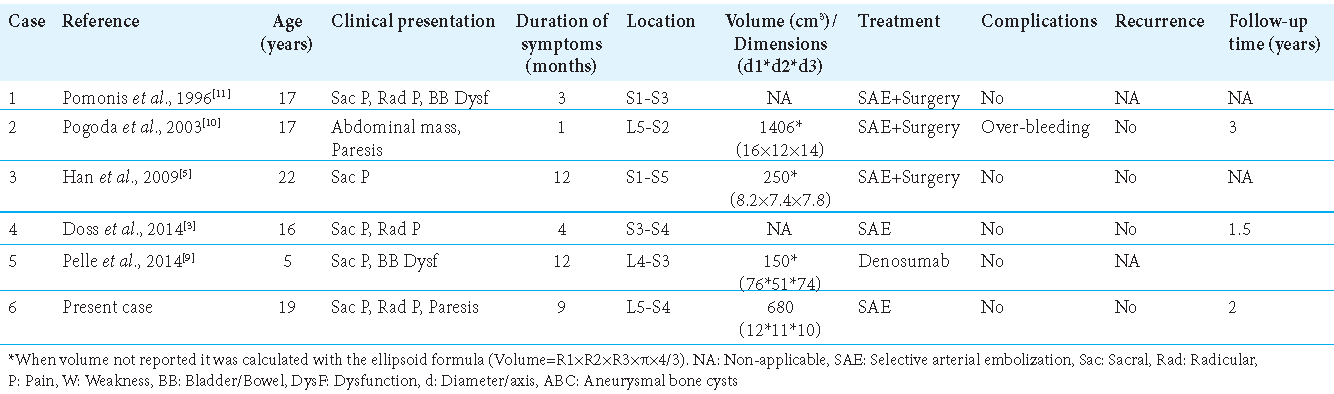
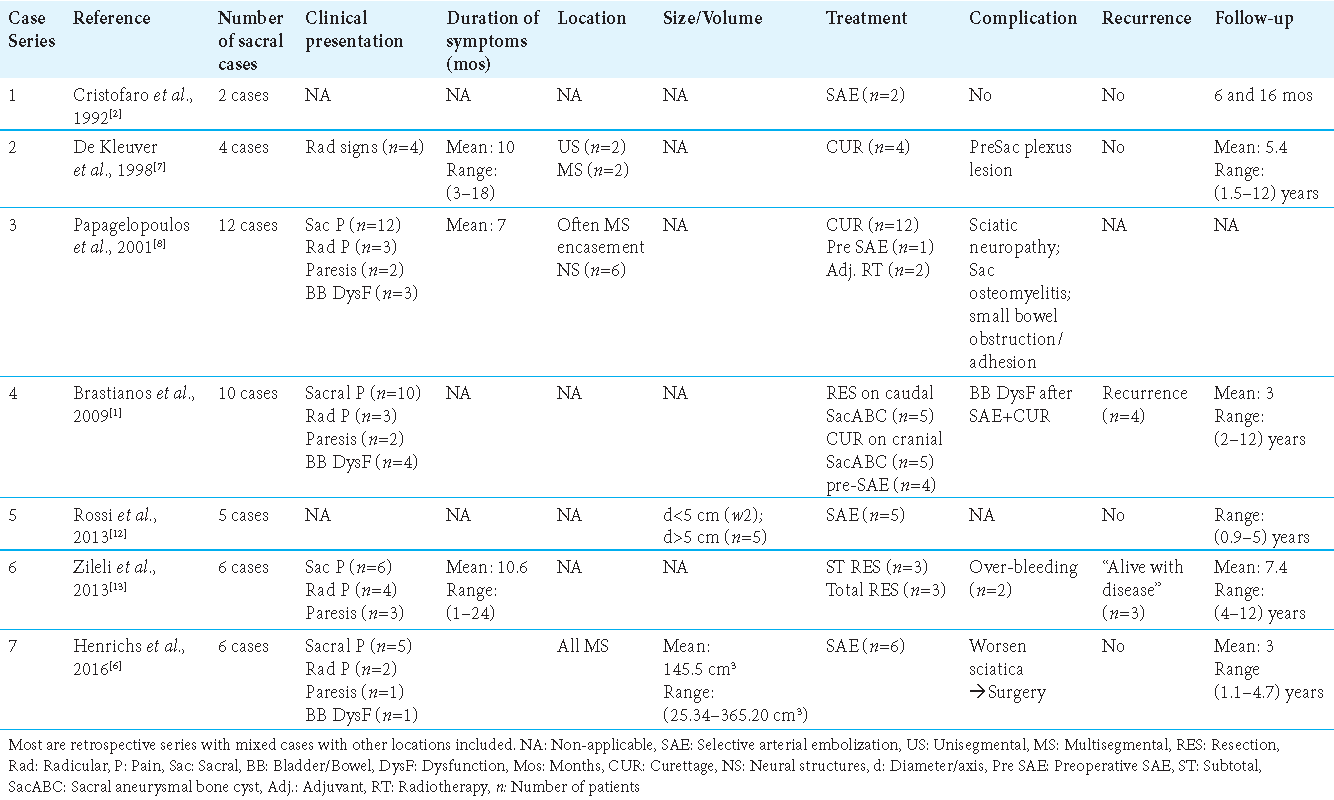
Increase in endovascular arterial embolization of sacral ABC to limit morbidity of surgery
The large extent of SABC, associated with increased perioperative morbidity (i.e., risks of gross total en bloc excision or curettage resulting in life-threatening intraoperative bleeding, and/or significant neurologic deficits) has prompted greater interest in alternative treatment with endovascular arterial embolization. We identified 14 sacral ABC cases from the literature that were successfully treated with SAE (i.e., spinal arterial embolization) performed in 1–3 stages; the most significant improvement usually occurred within the first few days following the first embolization stage.[
CONCLUSION
We successfully treated a 19-year-old female’s large multisegmental sacral ABC with 2-staged endovascular embolization.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Brastianos P, Gokaslan Z, McCarthy EF. Aneurysmal bone cysts of the sacrum: A report of ten cases and review of the literature. Iowa Orthop J. 2009. 29: 74-8
2. De Cristofaro R, Biagini R, Boriani S, Ricci S, Ruggieri P, Rossi G. Selective arterial embolization in the treatment of aneurysmal bone cyst and angioma of bone. Skeletal Radiol. 1992. 21: 523-7
3. Doss VT, Weaver J, Didier S, Arthur AS. Serial endovascular embolization as stand-alone treatment of a sacral aneurysmal bone cyst. J Neurosurg Spine. 2014. 20: 234-8
4. Enneking WF. A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res. 1986. 204: 9-24
5. Han HJ, Lee SG, Park CW, Yoo CJ, Kim WK. Huge aneurysmal bone cyst of the sacrum. Korean J Spine. 2009. 1: 35-9
6. Henrichs MP, Beck L, Gosheger G, Streitbuerger A, Koehler M, Heindel W. Selective arterial embolisation of aneurysmal bone cysts of the sacrum: A promising alternative to surgery. Fortschr Röntgenstr. 2016. 188: 53-9
7. Kleuver M, van der Heul RO, Veraart BE. Aneurysmal bone cyst of the spine. J Pediatr Orthop B. 1998. 7: 286-92
8. Papagelopoulos PJ, Choudhury SN, Frassica FJ, Bond JR, Unni KK, Sim FH. Treatment of aneurysmal bone cysts of the pelvis and sacrum. J Bone Joint Surg Am. 2001. 83: 1674-81
9. Pelle DW, Ringler JW, Peacock JD, Kampfschulte K, Scholten DJ, Davis MM. Targeting receptor-activator of nuclear kappaB ligand in aneurysmal bone cysts: Verification of target and therapeutic response. Transl Res. 2014. 164: 139-48
10. Pogoda P, Linhart W, Priemel M, Rueger JM, Amling M. Aneurysmal bone cysts of the sacrum. Clinical report and review of the literature. Arch Orthop Trauma Surg. 2003. 123: 247-51
11. Pomonis S, Machera M, Sakellaridis N, Grammenou M, Anagnostopoulos D, Kelekis D. Giant aneurysmal bone cyst of the sacrum. Neuroradiol J. 1996. 9: 619-22
12. Rossi G, Rimondi E, Bartalena T, Gerardi A, Alberghini M, Staals EL. Selective arterial embolization of 36 aneurysmal bone cysts of the skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol. 2009. 39: 161-7
13. Zileli M, Isik HS, Ogut FE, Is M, Cagli S, Calli C. Aneurysmal bone cysts of the spine. Eur Spine J. 2013. 22: 593-601