- Medical Student, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India
- Department of General Surgery, Medical College, Jagadguru Jayadeva Murugarajendra (JJM), Medical College, Davangere, Karnataka, India
- Department of Neurosurgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India
- Department of Neurosurgery, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India
Correspondence Address:
Jitender Chaturvedi, Department of Neurosurgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand,
DOI:10.25259/SNI_79_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abhishek Mehan1, FNU Ruchika2, Jitender Chaturvedi3, Mohit Gupta3, Tejas Venkataram3, Nishant Goyal3, Anil Kumar Sharma4. Giant Tarlov Cyst presenting as pelvic mass: Often doing less is better. 24-Mar-2023;14:95
How to cite this URL: Abhishek Mehan1, FNU Ruchika2, Jitender Chaturvedi3, Mohit Gupta3, Tejas Venkataram3, Nishant Goyal3, Anil Kumar Sharma4. Giant Tarlov Cyst presenting as pelvic mass: Often doing less is better. 24-Mar-2023;14:95. Available from: https://surgicalneurologyint.com/surgicalint-articles/12218/
Abstract
Background: Tarlov cysts are sacral perineural cysts arising between the peri and endoneurium of the posterior spinal nerve root at the Dorsal Root Ganglion and have a global prevalence rate of 4.27%. These are primarily asymptomatic (only 1% with symptoms) and typically arise in females between the ages of 50–60. Patients’ symptoms include radicular pain, sensory dysesthesias, urinary and/or bowel symptoms, and sexual dysfunction. Non-surgical management with lumbar cerebrospinal fluid drainage and computerized tomography-guided cyst aspiration typically provide only months of improvement before recurring. Surgical treatment includes a laminectomy, cyst, and/or nerve root decompression with fenestration of the cyst and/ or imbrication. Early surgery for large cysts provides the longest symptom-free periods.
Case Description: A 30-year-old male presented with a very large magnetic resonance-documented Tarlov cyst (Nabors Type 2) arising from bilateral S2 nerve root sheaths with marked pelvic extension. Although he was initially treated with a S1, S2 laminectomy, closure of the dural defect, and excision/marsupialization of the cyst, he later required placement of a thecoperitoneal shunt (TP shunt).
Conclusion: A 30-year-old male with large Nabors Type 2 Tarlov cyst arising from both S2 nerve root sheaths required a S1-S2 laminectomy, dural closure/marsupialization, and imbrication of the cyst, eventually followed by placement of a TP shunt.
Keywords: Nabor cyst, Pelvic cyst, Spine, Tarlov cyst, Theco-peritoneal shunt
INTRODUCTION
We present a 30-year-old male whose lower extremity radicular and sphincteric complaints attributed to an magnetic resonance (MR)-documented Type 2 Tarlov cyst arising from both S2 nerve root sheaths. Although he underwent a laminectomy, closure of the bilateral dural fistulas with imbrication/marsupialization of the sacral cysts, he ultimately required placement of a thecoperitoneal (TP) shunt.
CASE DETAILS
A 30-year-old male presented with posterior left thigh pain of 18 months’ duration and 1 year of urinary frequency/urgency, constipation, and scrotal/perineal pain. The lumbosacral MR imaging (MRI) revealed a Tarlov cyst (Nabors Type 2) arising from bilateral S2 nerve root sheaths with marked pelvic extension.
Computerized tomography (CT) and MR findings
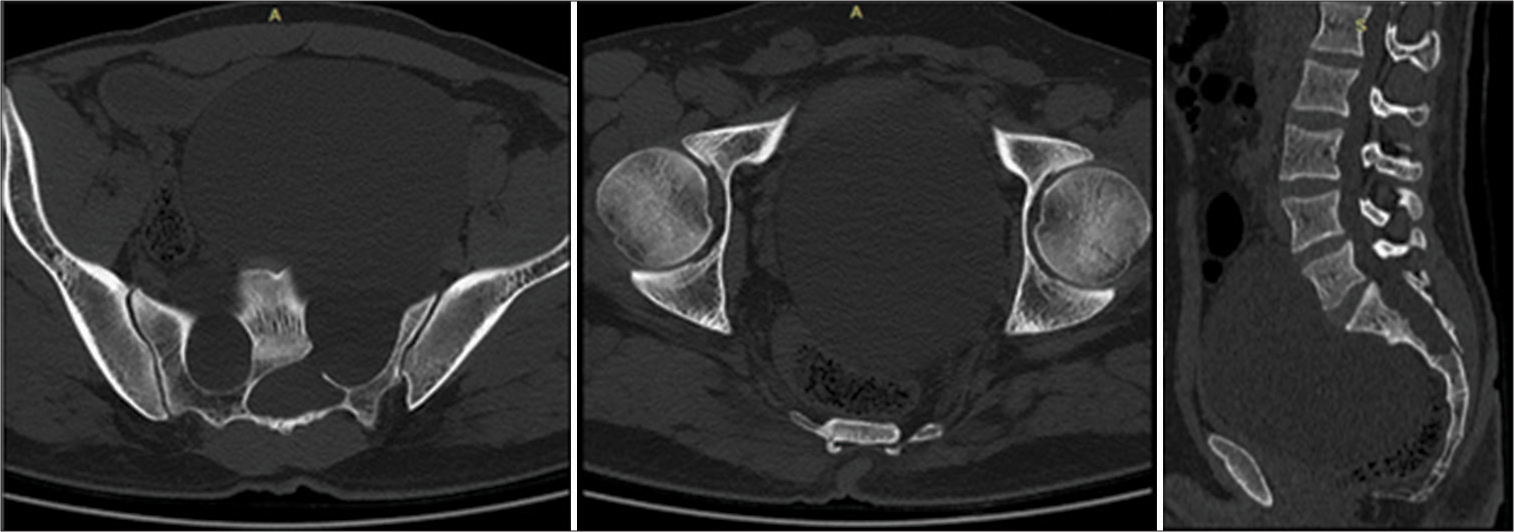
A Nabors-2 Tarlov cyst was diagnosed based on both lumbosacral CT and MR studies. The CT showed a hypodense lesion filling the pelvic cavity origination from bilateral S1 sacral roots, accompanied by chronic bony erosion of the sacrum at multiple levels (i.e., specially from S2 to 4) [
Figure 1:
Axial and sagittal computerized tomography scan of Lumbo-Sacral (LS) spine. Hypodense Expansile cystic lesion is seen filling the pelvic cavity reaching almost up to the anterior abdomen wall. It displaces the bladder and rectum posteroinferior with bony erosions of the sacrum from S2-4. Note the simultaneous spinal canal expansion at the S2-4 level.
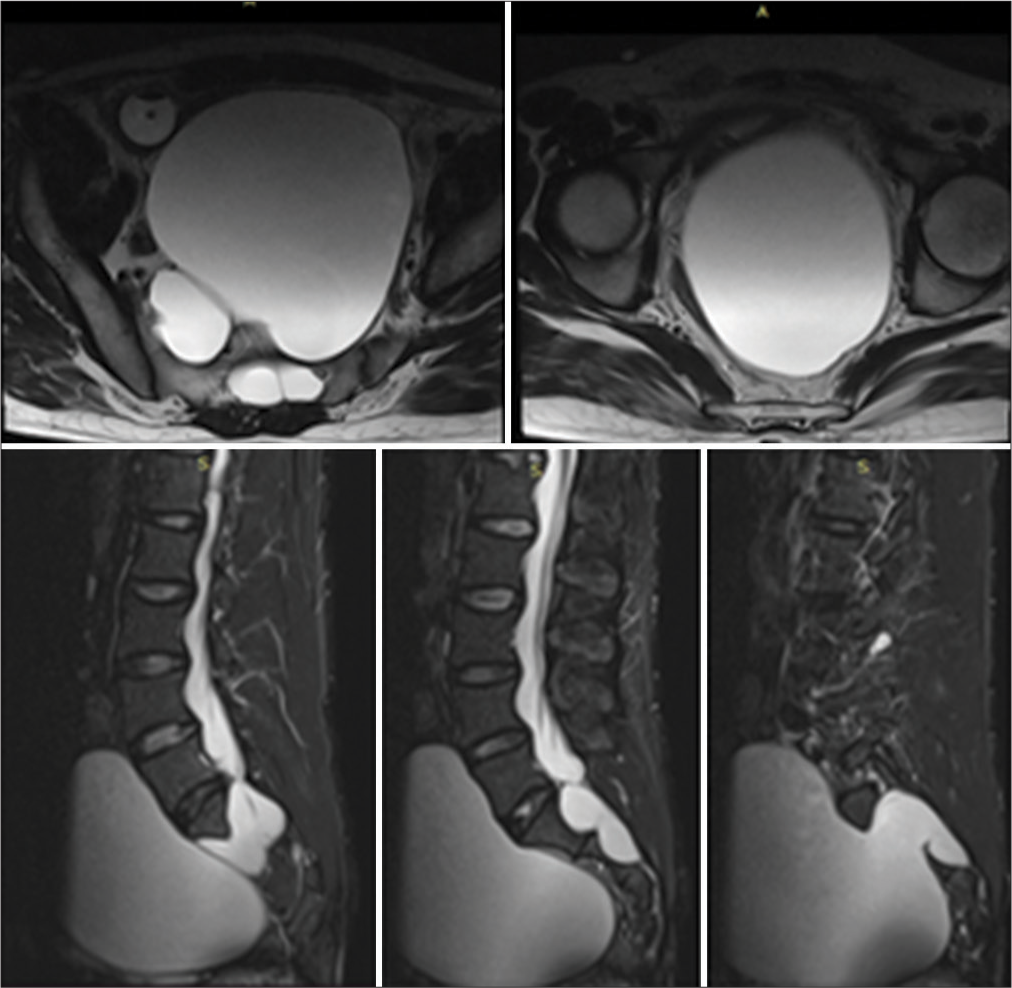
Figure 2:
Preoperative axial and sagittal T2-W magnetic resonance imaging scan Lumbo-Sacral (LS) spine. The T2-hypointense lesion originates from bilateral neural foramen at the level of S2. Appreciate the septa between two sides of the cavities within the pelvis. Bony elements are seen missing at levels S2-4.
Surgery
Following a S1, S2 laminectomy, dural fistula closure, and excision/marsupialization of the cyst, he remained asymptomatic for a few months. However, 6 months later symptoms recurred at which point he underwent, lumbar drainage that relieved his urinary complaints; a TP shunt was then placed. At surgery, two separate large tense cysts were encountered extradurally surrounding the bilateral S2; these cysts extended ventrally into the pelvis. Another small cyst compressed the left S1 root as it exited the canal. The three cysts were incised and drained (i.e., around 1.5 L of Cerebro-Spinal Fluid (CSF). Biopsies were taken from the cyst walls, and the cysts were marsupialized. In addition, gel foam was placed over the neck of the bilateral cysts bilaterally in conjunction with the application of fibrin glue (i.e., over the dura and cyst necks).
Postoperative MR imaging
The postoperative spine/pelvic MR revealed air-fluid levels in both cysts which were reduced in size vs. the preoperative scans.
Postoperative symptoms
Postoperatively, the patient had severe headaches that resolved within the 1st postoperative day by keeping the head of bed flat. By postoperative day 2, there was complete resolution of the deep pelvic pain and no further urinary symptoms. The remainder of the postoperative course was uneventful, and the patient was discharged on postoperative day 5.
Recurrent symptoms requiring placement of a TP shunt
Within 6 postoperative months, the patient presented with recurrent symptoms (i.e., pelvic pain and urinary dysfunction).The lumbosacral MR spine now revealed a posterior dural sac-CSF collection, measuring 4 × 4.4 × 10 cm (AP × TR × CC) with recurrent bilateral presacral tarlov cysts communicating with the thecal sac (i.e., thorough the neural foramina of S1-S2, right Cyst 4.6 × 3.3 × 4.2 cm, left cyst 12.3 × 12 × 15.4 cm [AP × TR × CC]) [
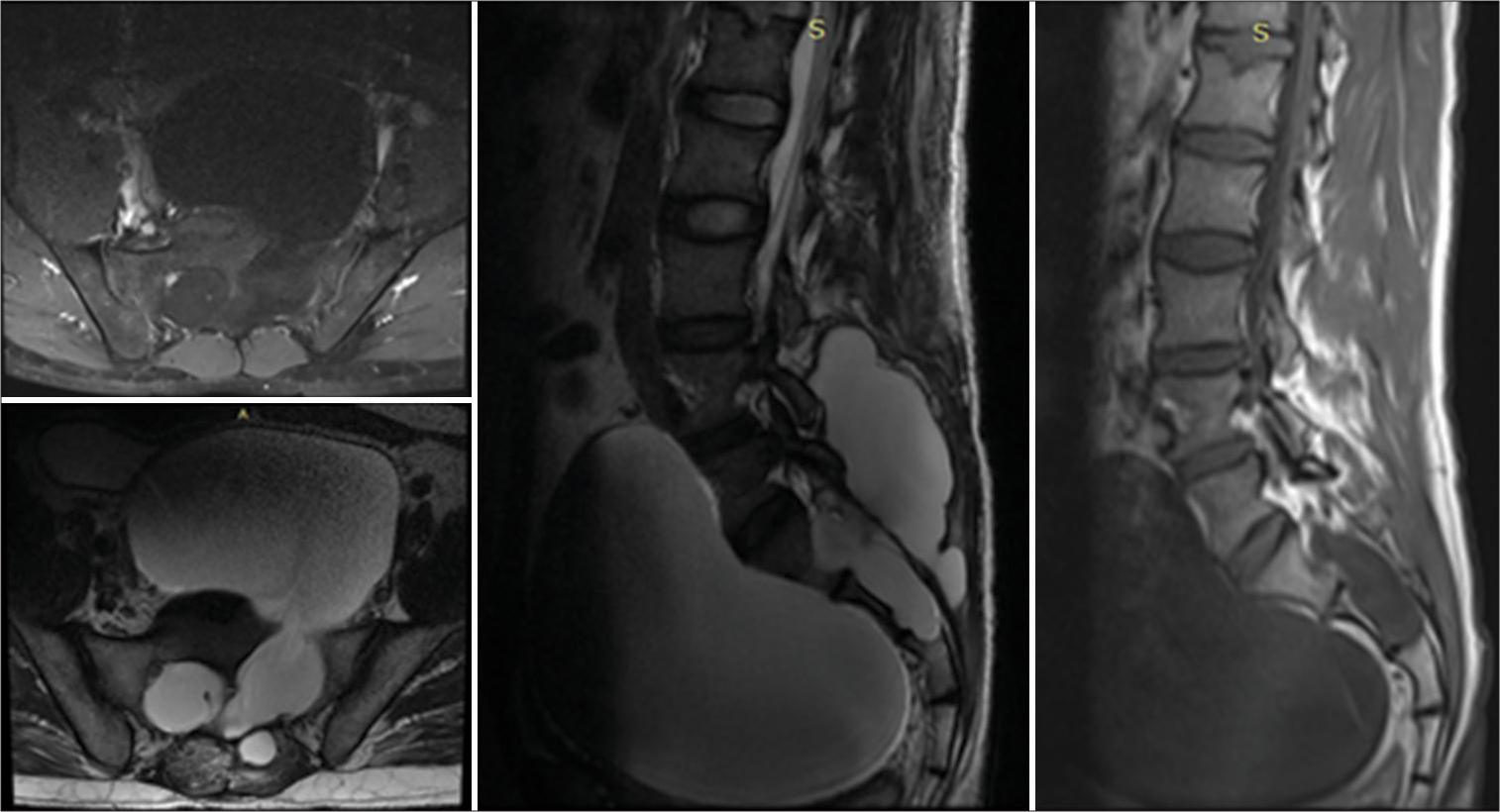
Figure 3:
Axial and sagittal magnetic resonance imaging scan of Lumbo-Sacral (LS) spine 6 months after index surgery. T1-hypointense and T2-hyperintense lesion is seen reappearing in the pelvic cavity. Posteriorly, the collection of cerebrospinal fluid can be noted at the level of surgery/laminectomy.
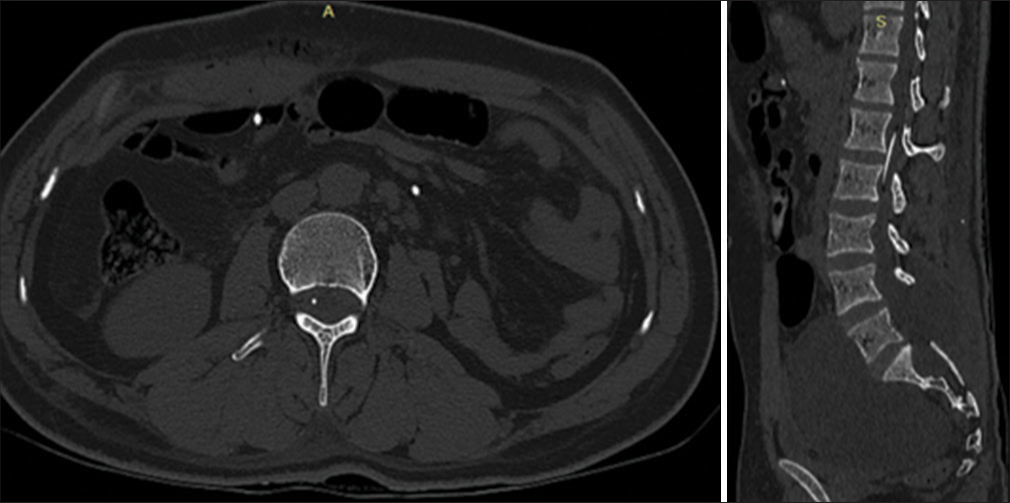
Figure 4:
Axial and sagittal computerized tomography scan revealing Theco-peritoneal (TP) shunt tip in the cavity of the spinal canal at the level of L1 vertebral body and reduction in the size of the cyst within the pelvic cavity. The white dots of the TP shunt can be seen within the peritoneal cavity.
DISCUSSION
Tarlov cysts are CSF-filled cavities contained by an epithelium first described in cadaveric surgery by Tarlov.[
Literature review
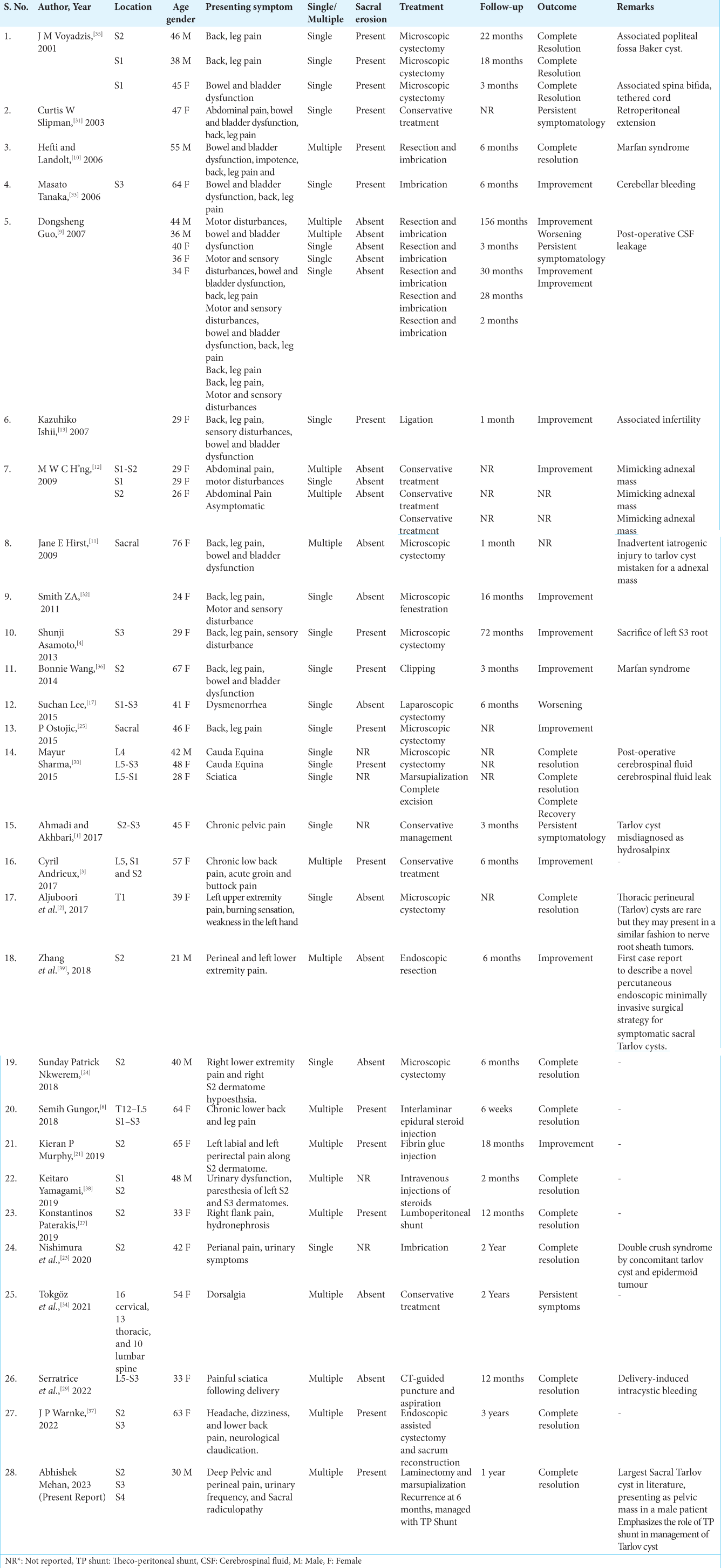
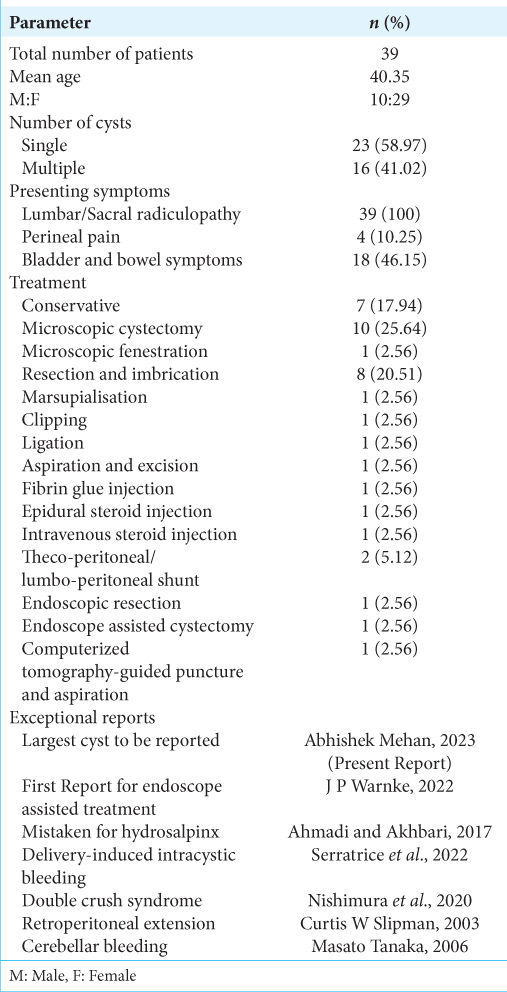
A review of the literature on Tarlov cysts showed that of the total 39 cases, the majority were females [
CONCLUSION
Tarlov cysts may become extremely large in the presacral region to the point where they contribute to significant pelvic pain and genitourinary symptoms mimicking a pelvic cavity tumor. Treatment typically consists of laminectomy, occlusion of the dural/subarchnoid fistula, and imbrication/ marsupialization of the cyst with select cases warranting the placement of TP shunts.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmadi F, Akhbari F. Adnexal masses or perineural (tarlov) cysts? Differentiation by imaging techniques: A case report. Int J Reprod BioMed. 2017. 15: 589-92
2. Aljuboori Z, Yaseen A, Simpson J, Boakye M. Surgical excision of a symptomatic thoracic nerve root perineural cyst resulting in complete resolution of symptoms: A case report. Cureus. 2017. 9: e1343
3. Andrieux C, Poglia P, Laudato P. Tarlov cyst: A diagnostic of exclusion. Int J Surg Case Rep. 2017. 39: 25-8
4. Asamoto S, Fukui Y, Nishiyama M, Ishikawa M, Fujita N, Nakamura S. Diagnosis and surgical strategy for sacral meningeal cysts with check-valve mechanism. Acta Neurochir (Wien). 2013. 155: 309-13
5. Cattaneo L, Pavesi G, Mancia D. Sural nerve abnormalities in sacral perineural (Tarlov) cysts. J Neurol. 2001. 248: 623-4
6. Chaturvedi J, Singh P, Malagi S, Goyal N, Sharma AK. Spinal extradural arachnoid cyst: Rare cases from Indian Institutes. Surg Neurol Int. 2020. 11: 306
7. Elatrozy HI, Saber SA, Abdelhameed E. Minimally invasive insertion of the coperitoneal shunts using ventriculoscope. Interdiscip Neurosurg. 2021. 25: 101274
8. Gungor S, Ozcan A. Management of lumbar radiculopathy due to disc herniation with interlaminar epidural steroid injection in the presence of multilevel Tarlov cysts in the neural foramina: A case report. Medicine. 2018. 97: e12389
9. Guo D, Shu K, Chen R, Ke C, Zhu Y, Lei T. Microsurgical treatment of symptomatic sacral perineurial cysts. Neurosurgery. 2007. 60: 1059-66
10. Hefti M, Landolt H. Presacral mass consisting of a meningocele and a Tarlov cyst: Successful surgical treatment based on pathogenic hypothesis. Acta Neurochir (Wien). 2006. 148: 479-83
11. Hirst JE, Torode H, Sears W, Cousins MJ. Beware the Tarlov cyst. J Minim Invasive Gynecol. 2009. 16: 78-80
12. H’ng MW, Wanigasiri UI, Ong CL. Perineural (Tarlov) cysts mimicking adnexal masses: A report of three cases. Ultrasound Obstet Gynecol. 2009. 34: 230-3
13. Ishii K, Yuzurihara M, Asamoto S, Doi H, Kubota M. A huge presacral Tarlov cyst: Case report. J Neurosurg Spine. 2007. 7: 259-63
14. Klepinowski T, Orbik W, Sagan L. Global incidence of spinal perineural Tarlov’s cysts and their morphological characteristics: A meta-analysis of 13,266 subjects. Surg Radiol Anat. 2021. 43: 855-63
15. Kubo S, Ueno M, Takimoto H, Karasawa J, Kato A, Yoshimine T. Endoscopically aided retroperitoneal placement of a lumboperitoneal shunt. Technical note. J Neurosurg. 2003. 98: 430-3
16. Kuhn FP, Hammoud S, Lefevre-Colau MM, Poiraudeau S, Feydy A. Prevalence of simple and complex sacral perineural Tarlov cysts in a French cohort of adults and children. J Neuroradiol. 2017. 44: 38-43
17. Lee ET, Wong FW. Dysmenorrhoea and adnexal cysts-a rare presentation of Tarlov cysts in the pelvis. J Clin Case Rep. 2015. 5: 476
18. Lockhart C, Selman W, Rodziewicz G, Spetzler RF. Percutaneous insertion of peritoneal shunt catheters with use of the Veress needle. Technical note. J Neurosurg. 1984. 60: 444-6
19. Medani K, Lawandy S, Schrot R, Binongo JN, Kim KD, Panchal RR. Surgical management of symptomatic Tarlov cysts: Cyst fenestration and nerve root imbrication-a single institutional experience. J Spine Surg. 2019. 5: 496
20. Mummaneni PV, Pitts LH, McCormack BM, Corroo JM, Weinstein PR. Microsurgical treatment of symptomatic sacral Tarlov cysts. Neurosurgery. 2000. 47: 74-8
21. Murphy KP, Ryan S. Shrinking of a Tarlov cyst. BMJ Case Rep. 2019. 12: e227256
22. Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988. 68: 366-77
23. Nishimura Y, Hara M, Awaya T, Ando R, Eguchi K, Nagashima Y. Possible double crush syndrome caused by iatrogenic acquired lumbosacral epidermoid tumor and concomitant sacral Tarlov cyst. NMC Case Rep J. 2020. 7: 195-9
24. Nkwerem SP, Ito K, Ichinose S, Horiuchi T, Hongo K. Resection and imbrication of symptomatic sacral Tarlov cysts: A case report and review of the literature. Surg Neurol Int. 2018. 9: 180
25. Ostojic P. Sacral perineural cyst mimicking inflammatory low back pain. Z Rheumatol. 2015. 74: 75-7
26. Patel MR, Louie W, Rachlin J. Percutaneous fibrin glue therapy of meningeal cysts of the sacral spine. AJR Am J Roentgenol. 1997. 168: 367-70
27. Paterakis K, Brotis A, Bakopoulou M, Rountas C, Dardiotis E, Hadjigeorgiou GM. A giant Tarlov cyst presenting with hydronephrosis in a patient with Marfan syndrome: A case report and review of the literature. World Neurosurg. 2019. 126: 581-7
28. Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts). Am J Neuroradiol. 1994. 15: 293-7
29. Serratrice N, Taifour S, Attieh C, Faddoul J, Tarabay B, Yachou Y. CT-guided aspiration of a hemorrhagic Tarlov cyst for the treatment of a Post-partum sciatica: A case report and a review of the literature. Front Surg. 2022. 9: 788786
30. Sharma M, Velho V, Mally R, Khan S. Symptomatic lumbosacral perineural cysts: A report of three cases and review of literature. Asian J Neurosurg. 2015. 10: 222-5
31. Slipman CW, Bhat AL, Bhagia SM, Issac Z, Gilchrist RV, Lenrow DA. Abdominal pain secondary to a sacral perineural cyst. Spine J. 2003. 3: 317-20
32. Smith Z, Khoo L. Sacral laminoplasty and fenestration of sacral Tarlov cysts: Clinical outcomes and complications. Spine J. 2011. 11: S119-20
33. Tanaka M, Nakahara S, Ito Y, Nakanishi K, Sugimoto Y, Ikuma H. Surgical results of sacral perineural (Tarlov) cysts. Acta Med Okayama. 2006. 60: 65-70
34. Tokgöz MA, Kılıçaslan ÖF Parlak AE. Multiple perineural cysts in the cervical, thoracic, and lumbar vertebrae of a mature individual. Jt Dis Relat Surg. 2021. 32: 262-6
35. Voyadzis JM, Bhargava P, Henderson FC. Tarlov cysts: A study of 10 cases with review of the literature. J Neurosurg Spine. 2001. 95: 25-32
36. Wang B, Moon SJ, Olivero WC, Wang H. Pelvic pain from a giant presacral tarlov cyst successfully obliterated using aneurysm clips in a patient with Marfan syndrome: Case report. J Neurosurg Spine. 2014. 21: 833-6
37. Warnke JP, Chanamoglu V, Mawrin C. Histopathology of a symptomatic Tarlov cyst-Case report and review of the literature. Interdiscip Neurosurg. 2022. 28: 101426
38. Yamagami K, Shono T, Iihara K. Multiple sacral perineurial cysts presented symptoms triggered by nonaneurysmal perimesencephalic subarachnoid hemorrhage. NMC Case Rep J. 2019. 6: 57-60
39. Zhang B, Dou Q, Feng P, Kong Q. Percutaneous endoscopic treatment for a symptomatic sacral Tarlov cyst. World Neurosurg. 2018. 116: 390-3