- Department of Neurosurgery, Tokyo General Hospital, Nakano, Tokyo, Japan,
- Department of Neurosurgery, University of Pittsburgh Medical Center (UPMC), Pittsburgh, Pennsylvania, USA,
- Department of Neurosurgery, Hannover Medical School, Hannover, Germany.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Pittsburgh Medical Center (UPMC), Pittsburgh, Pennsylvania, USA.
DOI:10.25259/SNI_611_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Awfa Aktham Abdulateef1, Shuhei Morita1, Samer S. Hoz2, Oday Atallah3, Shinichi Numazawa1, Yasunobu Ito1, Sadayoshi Watanabe1, Kentaro Mori1. Glioependymal cyst in the medulla oblongata – A case report. 15-Dec-2023;14:432
How to cite this URL: Awfa Aktham Abdulateef1, Shuhei Morita1, Samer S. Hoz2, Oday Atallah3, Shinichi Numazawa1, Yasunobu Ito1, Sadayoshi Watanabe1, Kentaro Mori1. Glioependymal cyst in the medulla oblongata – A case report. 15-Dec-2023;14:432. Available from: https://surgicalneurologyint.com/surgicalint-articles/glioependymal-cyst-in-the-medulla-oblongata-a-case-report/
Abstract
Background: Glioependymal cysts (GECs) are rare benign lesions that can be found anywhere along the neuroaxis, with most of the reports denoting supratentorial location. Here, we introduce a rare case of successfully treated glioependymal cysts lying in an uncommon location, namely medulla oblongata.
Case Description: A 69-year-old lady presented with progressive unsteadiness and swallowing disturbances, and brain magnetic resonance imaging showed a dorsally located lesion within the medulla oblongata; based on the presentation and radiological features, surgical intervention was deemed mandatory. The suboccipital midline approach was used to perform marsupialization of the cyst with shunting through a syringosubarachnoid shunt to prevent future recurrence, and the patient outcome was improved.
Conclusion: Medulla Oblongata’s location for glioependymal cysts proposed unique diagnostic and operative challenges that may require highlighting for practicing neurosurgeons.
Keywords: Benign intracranial cyst, Glioependymal cyst, Medulla oblongata, Neuroepithelial cyst
INTRODUCTION
Glioependymal cysts (GECs) are rare benign cystic lesions of congenital ectodermal origin.[
Preoperative diagnosis is challenging, as GECs share many clinical and radiological characteristics with other anomalies, making histopathological studies the only way to differentiate between them. GECs can be found intra-axial or extra-axial, with the former being more common, predominantly in the frontal lobe.[
Here, we report a rare case of surgically managed GEC located in the dorsal of the medulla oblongata.
CASE SCENARIO
A 69-year-old lady had unsteadiness with swallowing difficulty that worsened gradually. Further complicated by severe aspiration pneumonia, which required hospital admission. The patient suffered from tetraparesis, with hoarseness of voice, curtain sign on the right side, and coarse nystagmus bilaterally without extraocular movement abnormality. Later on, she did a brain magnetic resonance imaging (MRI), which showed an intra-axial cystic lesion within the posterior part of the medulla oblongata. It became thin as paper, and the cyst extended superiorly to the lower end of the fourth ventricle and inferiorly to level the C1. It did not communicate with the fourth ventricle; both tonsils displaced laterally. The cystic content followed cerebrospinal fluid (CSF) sequences, not restricted to diffusion-weighted imaging (DWI), with a hypointense signal in T1 and a hyperintense signal in T2. In addition, the capsule was not enhanced [
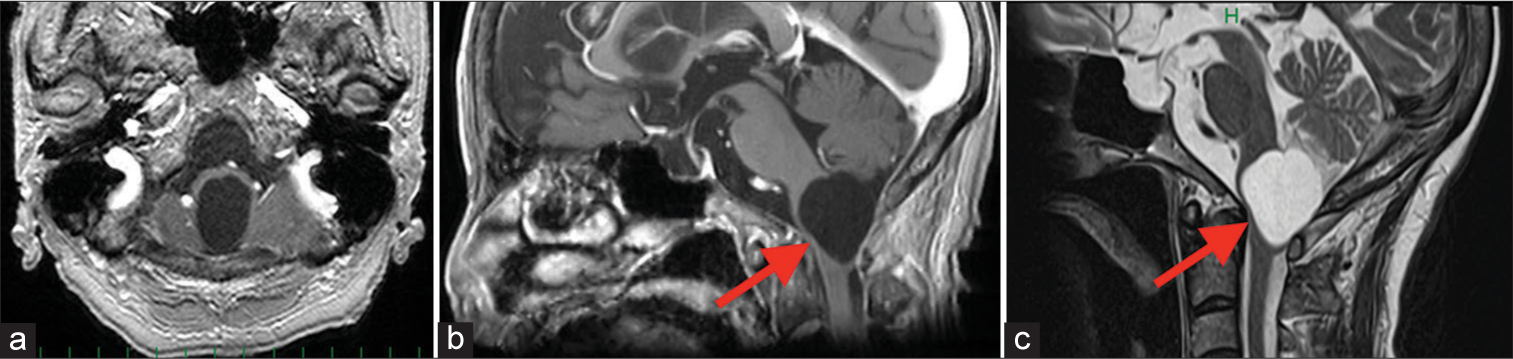
Figure 1:
Preoperative magnetic resonance imaging. (a) The axial T1-weighted image (T1WI) with contrast. (b) sagittal T1WI with contrast. (c) T2-weighted image sagittal. demonstrates that the cystic lesion follows the cerebrospinal fluid signal and located posteriorly with thinning of medulla oblongata. The red arrow represent the glioependymal cyst (GEC) in both 1b and 1c.
Intraoperatively, the cyst wall was whitish, transparent, and laid on the dorsal surface of the medulla oblongata; superiorly, it embedded into the foramen Magendie; meanwhile, the cyst wall was incised, biopsied, and sent for histopathology; and the cyst content was CSF-like clear, colorless fluid gashed out, and the part of the cyst wall which adherent to the medulla was intentionally left. Then, a shunt tube was placed between the cyst cavity and cervical subarachnoid space and fixed on the medulla using surgical fibrin glue [
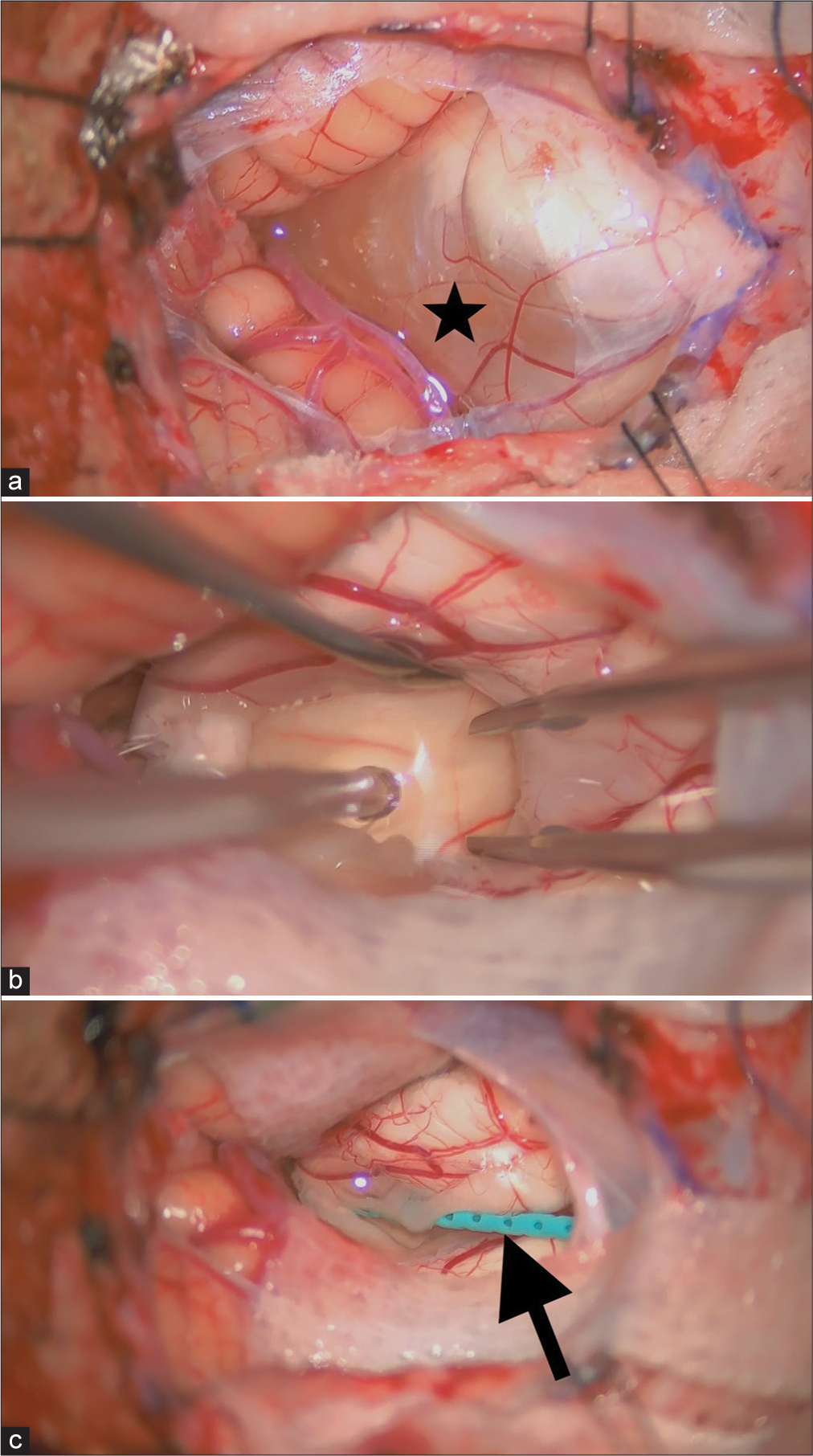
Figure 2:
Intraoperative views through the posterior midline approach show the cyst at the dorsal part of the medulla oblongata. (a) Thin, translucent cyst wall (black star), (b) The colorless fluid content, and (c) cysto-subarachnoid shunt placement (syringosubarachnoid shunt, create Medic Co., Ltd., Kanagawa, Japan) (the black arrow).
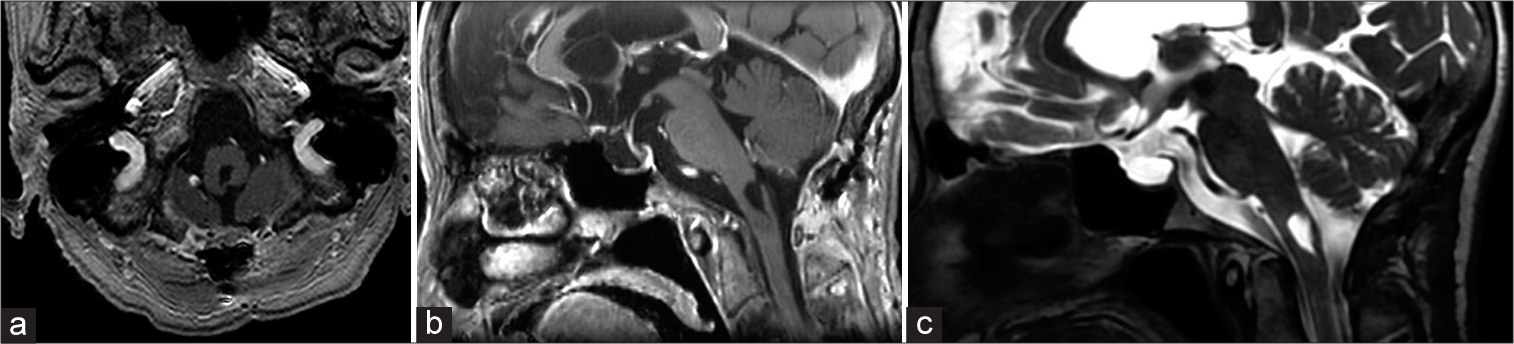
Following one month, the patient’s symptoms improved, and the follow-up MRI 3 months later showed a remarkable resolution of the cyst [
DISCUSSION
The glioependymal cyst (GEC) is a rare nonmalignant cyst that accounts for 0.01% of all central nervous system tumors. It is embryologically driven from ectopic rests of primitive neuroglial tissue, can occur in the midline or laterally, and has been reported both as a unilocular and multilocular anomaly.[
GECs had been described by multiple terms, including neuroglial, neuroepithelial, and choroidal cysts, which were previously used to designate different types of intracranial benign cysts with varied histopathologies. That makes the final interpretation challenging, which was rationalized by Robles et al. Thus, the term “glioependymal cyst” should be used to describe a unique set of cysts with specific pathological and radiological features.[
GECs, presentations were varied owing to their slow-growing nature, with diversity in location commonly causing seizure and compression of adjacent neuronal structure,[
Owing to their neuroepithelial origin, they can be found along the neuroaxis, with the supratentorial location, like the frontal lobe, being the most common. Few articles report the posterior cranial fossa as in the cerebellum, pons, as a site for GECs. In our case, the GEC is located in the medulla oblongata, which was not reported before.[
Radiologically, GECs are unilocular cysts with thin-walled morphology on computed tomography and MRI. In most reported papers, they were hypointense on T1-weighted and fluid-attenuated inversion recovery images and hyperintense on T2-weighted images, were neither restricted in diffusion-weighted sequence nor enhanced with contrast, and did not have edema. Robles et al. reviewed that most of the intracranial benign cysts showed the same radiological findings.[
Treatment was directed for the symptomatic, progressive in nature cases, not for the incidentally discovered ones.[
Intraoperatively, GECs consisted of a thin translucent or grayish membrane with no communication with the subarachnoid or ventricular spaces and contain CSF-like clear fluid in most of the reported cases, with very slow growth due to the activity of the ependymal cells.[
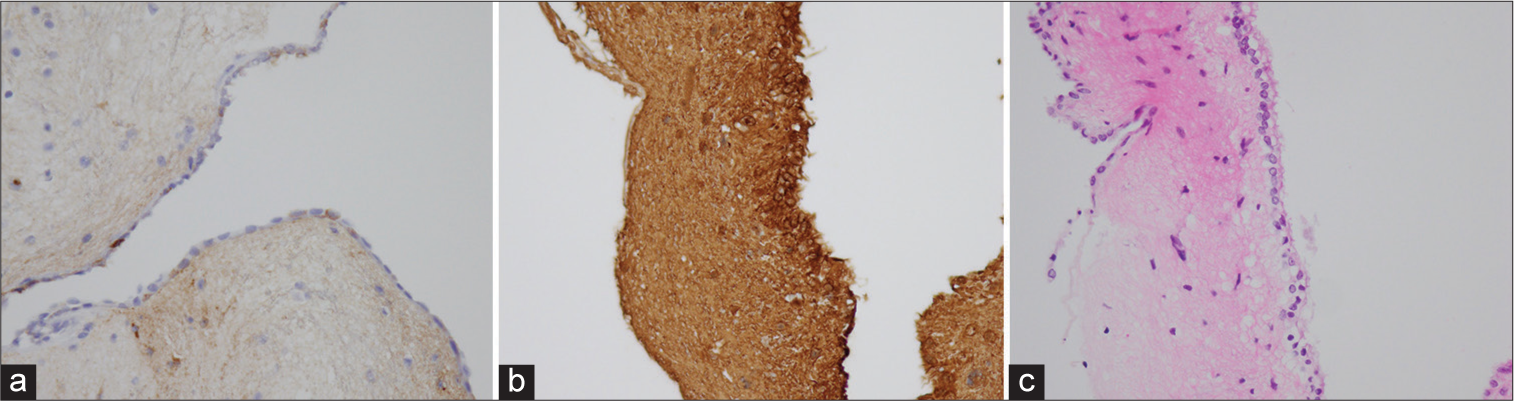
Most reviewers described the wall of GECs as being formed by two or three different layers, and owing to their embryologic origin, they were also positive for GFAP and lacked reactivity for cytokeratin, carcinoembryonic antigen, and EMA.[
In summary, GECs can be easily confused with another intra-axial benign cystic lesion. Owing to the similarity in radiology and presentation with other benign cystic lesions, we suggest that the differential diagnosis of posterior fossa cystic lesions be inclusive to GECs as a rare and unique lesion. We reported a case of a rare GEC location within the dorsal medulla oblongata. The cyst was successfully treated through partial cyst wall removal followed by cystosubarachnoid shunt using a midline suboccipital approach. This approach will enable the avoidance of parenchymal injury of the medulla and prevent recurrence.
CONCLUSION
There are distinct diagnostic and operative challenges associated with the location of glioependymal cyst in the medulla oblongata that may be required to be emphasized by daily practicing neurosurgeons.
Ethical approval
Not applicable.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Andrews BT, Halks-Miller M, Berger MS, Rosenblum ML, Wilson CB. Neuroepithelial cysts of the posterior fossa: Pathogenesis and report of two cases. Neurosurgery. 1984. 15: 91-5
2. Cavalheiro S, Canullo ML, Silva da Costa MD, Dastoli PA, Mendonça Nicácio J, Stavale JN. Glioependymal cyst on the third cranial nerve: Case report. J Neurosurg Pediatr. 2019. 25: 178-82
3. Frazier J, Garonzik I, Tihan T, Olivi A. Recurrent glioependymal cyst of the posterior fossa: An unusual entity containing mixed glial elements. Case report. J Neurooncol. 2004. 68: 13-7
4. Hacıyakupoğlu E, Kayalar AE, Efendioğlu M, Hacıyakupoğlu S. Conflicting behavior of glioependymal cyst: A report of three cases and review of literature. Haydarpasa Numune Med J. 2023. 63: 223-6
5. Kim E. Cerebellar glioependymal cyst. Brain Tumor Res Treat. 2021. 9: 31-4
6. Lach B, Russell N, Atack D, Benoit B. Intraparenchymal epithelial (enterogenous) cyst of the medulla oblongata. Can J Neurol Sci. 1989. 16: 206-10
7. Park CH, Hyun SJ, Kim KJ, Kim HJ. Spinal intramedullary ependymal cysts: A case report and review of the literature. J Korean Neurosurg Soc. 2012. 52: 67-70
8. Qi X, Xie D, Wan Y, Zhu Y, Ma Z, Chen K. Glioependymal cyst of frontal lobe. Neurosurg Q. 2015. 25: 280-2
9. Robles LA, Paez JM, Ayala D, Boleaga-Duran B. Intracranial glioependymal (neuroglial) cysts: A systematic review. Acta Neurochir (Wien). 2018. 160: 1439-49
10. Samadian M, Omidbeigi M, Bakhtevari MH, Asaadi S, Jafari A, Rezaei O. Nerve-sheath-risen neuroglial cyst: Case report and review of the literature. World Neurosurg. 2019. 124: 251-5
11. Schieferdecker S, Hunsche S, El Majdoub F, Maarouf M. Robot-assisted stereotactic shunting as a novel treatment for pontine glioependymal cysts. J Neurol Surg A Cent Eur Neurosurg. 2022. 83: 85-8
12. Tange Y, Aoki A, Mori K, Niijima S, Maeda M. Interhemispheric glioependymal cyst associated with agenesis of the corpus callosum-case report. Neurol Med Chir (Tokyo). 2000. 40: 536-42
13. Umredkar A, Mohindra S, Gupta R, Bal AK. Contrasting behavior of glio-ependymal cysts: A report of two cases and literature review. Neurol India. 2010. 58: 659-61