- Department of Neurosurgery, Soeradji Tirtonegoro Central Public Hospital, Klaten, Indonesia.
- Department of Urology, Soeradji Tirtonegoro Central Public Hospital, Klaten, Indonesia.
- Department of Pathology Anatomy, Soeradji Tirtonegoro Central Public Hospital, Klaten, Indonesia.
Correspondence Address:
Wisnu Baskoro, Department of Neurosurgery, Soeradji Tirtonegoro Central Public Hospital, Klaten, Indonesia.
DOI:10.25259/SNI_267_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Wisnu Baskoro1, Muhammad Fakhri Raiyan Pratama1, Hanan Anwar Rusidi1, Adhika Restanto Purnomo2, Bidari Kameswari3. Gross total resection of benign retroperitonealy/intra/paraspinal giant schwannoma. 31-May-2024;15:184
How to cite this URL: Wisnu Baskoro1, Muhammad Fakhri Raiyan Pratama1, Hanan Anwar Rusidi1, Adhika Restanto Purnomo2, Bidari Kameswari3. Gross total resection of benign retroperitonealy/intra/paraspinal giant schwannoma. 31-May-2024;15:184. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12915
Abstract
Background: Schwannoma is a typically benign nerve sheath tumor. Here, a 30-year-old female underwent resection of a benign retroperitoneal/intra/paraspinal schwannoma.
Case Description: A 30-year-old female originally had urological surgery to remove an ill-defined retroperitoneal tumor. When she newly presented with right-side low back pain, and the magnetic resonance documented a recurrent/residual L1–L3 intra/paraspinal lesion, she required an additional tumor excision for the removal of the benign schwannoma.
Conclusion: Spinal surgeons, dealing with benign schwannomas located in the retroperitoneal/intra/paraspinal compartments, need to work collaboratively with other surgeons (i.e., in this case, urologists) to achieve gross total tumor excision, and the best long-term results.
Keywords: Paraspinal, Schwannoma, Tumor
INTRODUCTION
Benign spinal schwannomas account for 25% of all spine tumors (i.e., 0.3–0.5/100,000). They are typically located extradurally, or in the intradural/extramedullary compartment (i.e., 0.3–0.5/100,000).[
CASE PRESENTATION
A 30-year-old female presented with 3 months of low back pain. Previously, urology had partially resected an undefined tumor in the peritoneal cavity. When she still complained of low back pain postoperatively, a lumbar MR was performed. It revealed a right-sided intra/paraspinal retroperitoneal hypointense mass on the T1-weighted and inhomogeneous hyperintense lesion on the T2-weighted study that was homogeneously enhanced with contrast [
Pathology
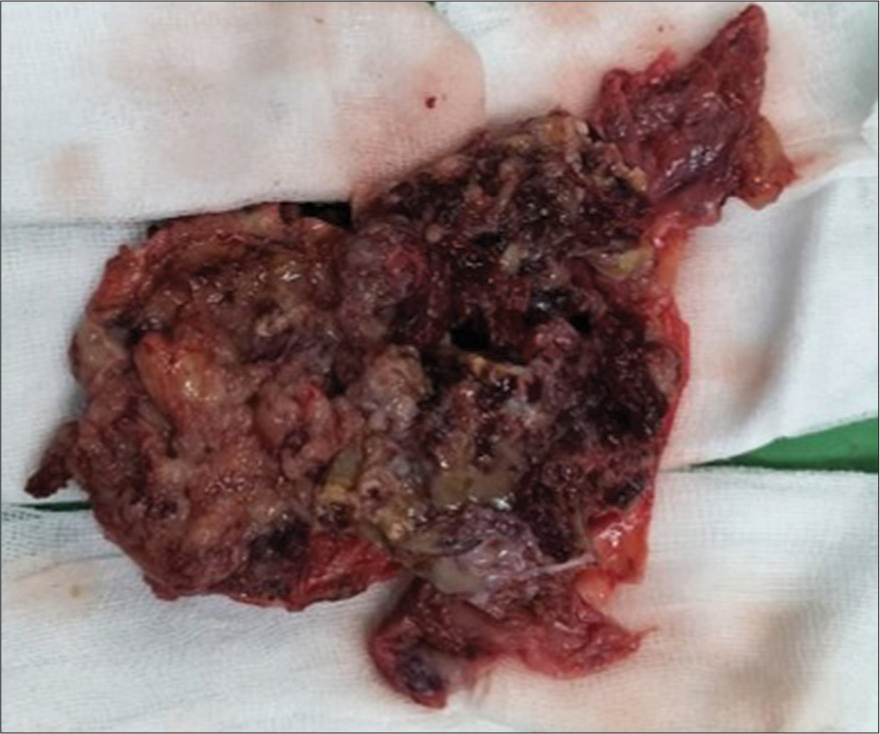
The histopathology was consistent with a benign schwannoma. Slides revealed partial palisading/cells arranged in longitudinal/transverse bundles containing monomorphic features, medium cytoplasm, and round and/or oval spindle nuclei. To confirm the findings, S100 immunohistochemistry demonstrated high-intensity positive staining of the nucleus/cytoplasm involving most tumor cells. Additional spinal muscular atrophy staining of tumor cells was negative. Microscopic features of the tumor can be seen in
Postoperative course
The patient had less pain on the 1st day following the postoperative day, and all symptoms/signs resolved within 1 week. At 3 postoperative months, she remains disease-free.
DISCUSSION
Gross total excision of spinal schwannomas is the treatment of choice.[
CONCLUSION
A 30-year-old female originally underwent resection of an intraperitoneal schwannoma by urology. When symptoms of low back pain persisted, and the lumbar MR identified a right-sided L1–L3 intra/paraspinal extension of the lateral/foraminal mass, the patient successfully underwent secondary gross total tumor resection.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abul-Kasim K, Thurnher MM, McKeever P, Sundgren PC. Intradural spinal tumors: Current classification and MRI features. Neuroradiology. 2008. 50: 301-14
2. Chen H, Xu Q, Zhan P, Liu Y, Dai M, Zhang B. Giant paravertebral schwannoma near the lumbar nerve roots with bone destruction: A case report. Medicine (Baltimore). 2019. 98: e17341
3. Gottfried ON, Binning MJ, Schmidt MH. A biweekly publication for clinical neurosurgical surgical approaches to spinal schwannomas. Contemp Neurosurg. 2005. 27: 1-8
4. Laliotis N, Chrysanthou C, Baskinis N, Konstandinidis P, Giannakopoulou L, Zarampouka K. Schwannoma of the lumbar spine, presenting with pain of the knee, like an osteoid osteoma, in a 10-year-old girl. Clin Case Rep. 2021. 9: 224-8
5. Liu Z, Xu Z, Shen J, Zhang T, Lin H, Zhou L. Scoring model to predict postoperative neurological deterioration in spinal schwannoma. Front Oncol. 2023. 13: 1086299
6. Savu C, Grigorie V, Melinte A, Diaconu C, Iliescu L, Dimitriu M. Giant Intrathoracic Schwannoma: A case report. In Vivo (Brooklyn). 2020. 34: 3527-32
7. Sun I, Pamir MN. Non-syndromic spinal schwannomas: A novel classification. Front Neurol. 2017. 8: 318
8. Vanegas Cerna G, Barrientos Castillo RE, Nurmukhametov R, Baldoncini M, López Lara CE, Rosario A. Giant invasive intradural extramedullary lumbar schwannoma: A case report and literature review. Cureus. 2023. 15: e40708
9. Zhou Y, Liu CZ, Zhang SY, Wang HY, Varma SN, Cao LQ. Giant schwannoma of thoracic vertebra: A case report. World J Clin Cases. 2021. 9: 11448-56