- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita City, Chiba, Japan.
Correspondence Address:
Yuhei Michiwaki, M.D., Ph.D., Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita City, Chiba, Japan.
DOI:10.25259/SNI_778_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuhei Michiwaki, Fumitaka Yamane, Hiroshi Itokawa, Tatsuya Tanaka, Kazuaki Shimoji, Akira Matsuno. Hands-on neuroendovascular practice for nonselective undergraduate medical students increases interest and aspirations in pursuing neurosurgery as a specialization. 01-Dec-2023;14:414
How to cite this URL: Yuhei Michiwaki, Fumitaka Yamane, Hiroshi Itokawa, Tatsuya Tanaka, Kazuaki Shimoji, Akira Matsuno. Hands-on neuroendovascular practice for nonselective undergraduate medical students increases interest and aspirations in pursuing neurosurgery as a specialization. 01-Dec-2023;14:414. Available from: https://surgicalneurologyint.com/surgicalint-articles/12651/
Abstract
Background: The number of medical students aspiring to become neurosurgeons has decreased worldwide, mainly due to poor work-life balance among neurosurgeons; therefore, recruiting students for neurosurgery is essential to ensure the availability and appropriate quality of neurosurgical treatment. This study aimed to evaluate the efficacy of hands-on neuroendovascular practice for nonselective undergraduate medical students to determine whether this increases their interest in neurosurgery and contributes to their aspirations of becoming neurosurgeons.
Methods: Hands-on neuroendovascular practice for mechanical thrombectomy was performed by undergraduate 5th-year medical students during their 2-week clinical rotation in the Department of neurosurgery at our university hospital between April 2021 and March 2023. After the neurosurgery practice, a questionnaire about their understanding of neurosurgery and aspirations for this specialization before and after the practice was anonymously completed by all students.
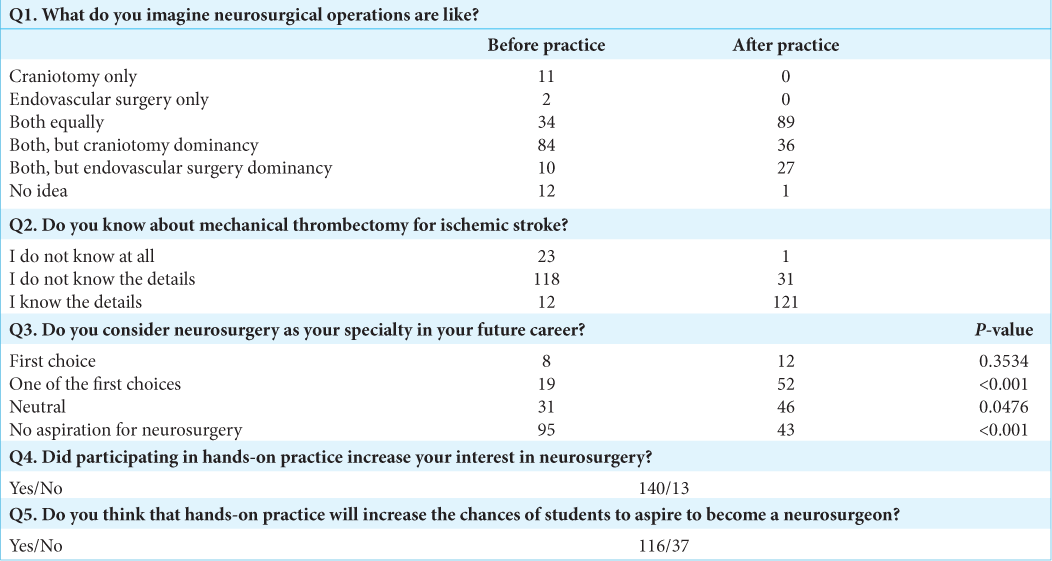
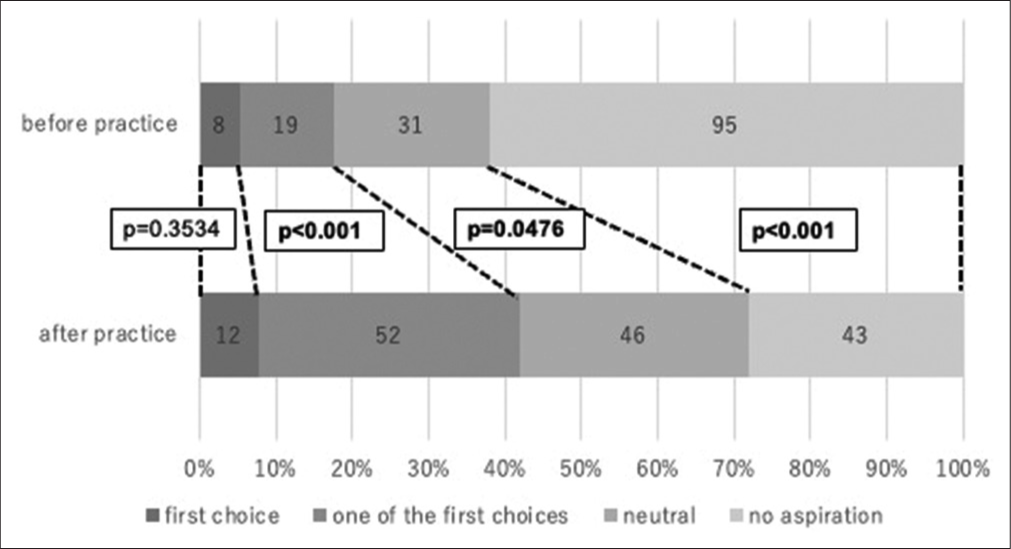
Results: Overall, 153 students completed the questionnaire. Of these, 140 (91.5 %) showed increased interest in neurosurgery after participating in the hands-on practice. Through this practice, the number of students who considered neurosurgery as their first choice or one of their specialty choices increased from 8 (5.2%) to 12 (7.8%) (P = 0.3534) and from 19 (12.4%) to 52 (34.0%) (P P
Conclusion: Hands-on neuroendovascular practice for nonselective undergraduate medical students effectively increased their interest in neurosurgery specialization and their desire to become neurosurgeons. Therefore, this practice can help recruit medical students for neurosurgery specialization.
Keywords: Education, Endovascular, Hands-on practice, Medical students, Neurosurgery
INTRODUCTION
Neurosurgery has a wide range of subspecialties and is used in the treatment of a large number of patients. Neurosurgical operations include direct surgeries and endovascular treatments. Direct surgeries have traditionally been the mainstay; however, endovascular treatments have been increasingly performed in recent decades. Moreover, the importance of neuroendovascular treatments have been highlighted by evidence for thrombectomy as a treatment for acute ischemic stroke. While neuroendovascular treatments are primarily performed by radiologists or neurologists in some countries, in Japan, neurosurgeons mostly perform the treatments, including thrombectomy. Therefore, the role of neurosurgeons and the demand for neurosurgeons have been on the rise in Japan.
Recruiting medical students for neurosurgery is essential for sufficient human resources to continue providing high-quality neurosurgical care. However, poor work-life balance and high rates of burnout among neurosurgeons are common concerns for physicians entering this specialty, and these can be largely attributed to aging in society and the burdens of neuro surgeries such as thrombectomy, which require prompt treatment.[
Medical education mainly consists of classroom lectures and bedside learning (BSL), with differences among countries and regions. In Japan, the medical university program consists of a 6-year program, and clinical practice typically commences during the 4th or 5th year. Our medical university was established in 2017, and the first batch of medical students graduated in 2023. According to the educational curricula of our university, 1–3rd-year medical students mainly attend classroom lectures, basic laboratory practicals, and anatomy practice, whereas 4th- and 5th-year medical students undergo BSL through practical training at university hospitals. In the Department of neurosurgery at our university hospital, hands-on neuroendovascular practice for mechanical thrombectomy is conducted for all students in addition to conference participation, lectures, surgery observations, and report writing. In the present study, we evaluated the effectiveness of this hands-on practice for nonselective undergraduate medical students, including those not interested in neurosurgery, to determine whether it increases their interest in neurosurgery and contributes to their aspirations of becoming neurosurgeons.
MATERIALS AND METHODS
Fifth-year medical students in groups of six or seven underwent a 2-week clinical rotation in the Department of Neurosurgery at our university hospital. The targeted students were the first batch who underwent BSL, including hands-on neuroendovascular practice, between April 2021 and March 2022 and the second batch who underwent the practice between April 2022 and March 2023. This study did not include patient information; therefore, the institutional review board’s approval was not required.
Hands-on neuroendovascular practice
Each group performed hands-on neuroendovascular practice for mechanical thrombectomy during BSL. First, the indications for and methods of thrombectomy were explained, and then a video demonstrating the procedure and typical movement of the catheter was presented. After the demonstration, a simulated thrombus was inserted into an artificial blood vessel model, and thrombectomy using a microcatheter and stent retriever was performed by each student. In addition, thrombectomy using an aspiration catheter only and a combined technique using an aspiration catheter and a stent retriever were also performed by the students, and the overall time for the hands-on practice ranged from 120 min to 150 min, depending on the number of students and the ease of progress.
Questionnaire
After the practice was completed, a questionnaire regarding the students’ understanding and their aspirations for specialization in their careers before and after the practice was anonymously collected from the students. The Chi-squared tests were used to investigate differences in the proportions of answers before and after the practice. The level of statistical significance was set at P < 0.05. JMP (version 17; SAS Institute, Cary, NC, USA) was used for all statistical analyses.
RESULTS
A total of 153 students, including 51 in the first batch and 102 in the second batch, completed the practice and questionnaire. The reasons for the lower number of responses from the first batch were the inclusion of students who did not practice at our hospital, the presence of groups that could not participate in the hands-on practice due to scheduling conflicts, and a low response rate. Details regarding the questionnaire and the students’ responses are presented in
DISCUSSION
In the present study, a hands-on neuroendovascular practice for nonselective medical students, including those not interested in neurosurgery, increased their interest in pursuing neurosurgery, increased the number of students aspiring to become neurosurgeons, and contributed to a mind shift in students with no interest in neurosurgery as a career.
The number of medical students aspiring to become neurosurgeons has decreased worldwide, with one of the major reasons being the poor work-life balance among neurosurgeons;[
In the present study, the number of students who wanted to select neurosurgery as one of their specialties significantly increased. Moreover, the number of students with no aspirations to become neurosurgeons significantly decreased after participation in the hands-on practice. However, the number of students who considered neurosurgery as their first-choice specialty did not significantly change. This might be because, although the hands-on practice increased student interest, they remained indecisive about whether this is a better option than other fields.
Interests and aspirations for a particular clinical department depend not only on the interests felt during the practice but also on factors such as job satisfaction, income, lifestyle, and working area. A few more years of follow-up are required to determine whether students will select neurosurgery as a specialization after exposure to the hands-on practice of performing neurosurgical procedures. However, the hands-on practice likely provided an impetus to aspire to become a neurosurgeon. Therefore, medical faculty should actively incorporate hands-on practice into students’ education to recruit students who find neurosurgery is interesting.
Study limitations
This study had some limitations, with the most important one being the lack of long-term follow-up. Given the questionnaire was administered right after participation, it is unclear whether a sustained interest in neurosurgery was generated and whether the practice increased the number of students applying for neurosurgery residency. In addition, there is a possibility of recall bias, as the students were questioned after the practice session about their interest in neurosurgery before the practice session. Moreover, if a group that did not receive the hands-on practice was established as a control group, it is possible that the efficacy of the practice could have become clearer. However, based on the principle of educational equity, no control group was established in this study. This study was conducted at a single facility in Japan, and the results may not be generalizable to larger populations in the authors’ countries or other countries. Since the environments surrounding medical students and neurosurgeons differ in each country, we believe that it is useful to take measures that correspond to each situation.
CONCLUSION
Hands-on neuroendovascular practice for nonselective medical students increased their interest in neurosurgery and aspirations of becoming neurosurgeons. In the future investigations into whether these students chose neurosurgery would be helpful.
Ethical approval
This study did not include patient information; therefore, the institutional review board’s approval was not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
We would like to thank Mr. Yosuke Akatsu, Stryker, Japan K.K., for his cooperation in the students’ hands-on practice.
References
1. Agarwal N, Norrmén-Smith IO, Tomei KL, Prestigiacomo CJ, Gandhi CD. Improving medical student recruitment into neurological surgery: A single institution’s experience. World Neurosurg. 2013. 80: 745-50
2. Burford C, Hanrahan J, Ansaripour A, Smith B, Sysum K, Rajwani K. Factors influencing medical student interest in a career in neurosurgery. World Neurosurg. 2019. 122: e367-74
3. Chan KI, Khu KJ, Brillante EM, Flores GP, Nakpil AS, Go DA. Perceptions and likelihood of medical students to pursue a career in neurosurgery: Findings from the Philippines. World Neurosurg. 2022. 164: e590-8
4. Ekhator C, Rak R. The need for improved recruitment to neurosurgery training: A systematic review of enrollment strategies. Cureus. 2022. 14: e26212
5. Flannery T, Gormley G. Evaluation of the contribution of theatre attendance to medical undergraduate neuroscience teaching--a pilot study. Br J Neurosurg. 2014. 28: 680-4
6. Huq S, Khalafallah AM, Ishida W, Porras JL, Lee RP, RinconTorroella J. Recruiting medical students to neurosurgery through a focused neuroanatomy lab initiative. World Neurosurg. 2020. 137: e535-46
7. Knight J, Stroud L, Geyton T, Stead A, Cock HR. Medical student perceptions of clinical neurosurgery teaching in an undergraduate medical school curriculum. Br J Neurosurg. 2017. 31: 727-30
8. Lubelski D, Xiao R, Mukherjee D, Ashley WW, Witham T, Brem H. Improving medical student recruitment to neurosurgery. J Neurosurg. 2019. 9: 1-7
9. McAbee JH, Ragel BT, McCartney S, Jones GM, Michael LM, DeCuypere M. Factors associated with career satisfaction and burnout among US neurosurgeons: Results of a nationwide survey. J Neurosurg. 2015. 123: 161-73
10. Nishimura K, Nakamura F, Takegami M, Fukuhara S, Nakagawara J, Ogasawara K. Cross-sectional survey of workload and burnout among Japanese physicians working in stroke care: The nationwide survey of acute stroke care capacity for proper designation of comprehensive stroke center in Japan (J-ASPECT) study. Circ Cardiovasc Qual Outcomes. 2014. 7: 414-22
11. Pugazenthi S, Islam AA, Sivakumar W, Dornbos DL, Johnson JN, Wolfe SQ. Assessing opportunities for formal exposure to clinical neurosurgery within United States allopathic medical education curricula. J Neurosurg. 2023. 139: 248-54
12. Saleh M. Attracting the top medical students to a career in neurosurgery. Br J Neurosurg. 2013. 27: 405
13. Sansosti AA, Jacobs RC, Safonova A, Jani RH, Schumann J, Friedlander RM. Impact of a hands-on pre-clinical neurosurgery elective course on second-year medical student interest and attitudes. J Med Educ Curric Dev. 2020. 7: 2382120520964852
14. Shakir HJ, McPheeters MJ, Shallwani H, Pittari JE, Reynolds RM. The prevalence of burnout among US neurosurgery residents. Neurosurgery. 2018. 83: 582-90
15. Williams MM, Wilson TA, Leslie-Mazwi T, Hirsch JA, Kellogg RT, Spiotta AM. The burden of neurothrombectomy call: A multicenter prospective study. J Neurointerv Surg. 2018. 10: 1143-8
16. Wilson TA, Leslie-Mazwi T, Hirsch JA, Frey C, Kim TE, Spiotta AM. A multicenter study evaluating the frequency and time requirement of mechanical thrombectomy. J Neurointerv Surg. 2018. 10: 235-9
17. Zoli M, Zenesini C, Bassani G, Colangelo A, Fayel E, Labanca Lima G. Shadows and lights: Perspectives of training and education in neurosurgery for undergraduate students. Front Surg. 2022. 9: 882063
18. Zuccato JA, Kulkarni AV. The impact of early medical school surgical exposure on interest in neurosurgery. Can J Neurol Sci. 2016. 43: 410-6