- Department of Neurosurgery, Hopital Maisonneuve-Rosemont, Québec, Canada.
- Department ofNeurosurgery, Centre Hospitalier de l’Université de Montréal, Montréal, Québec, Canada.
- Department of Orthopedics, Centre Hospitalier de l’Université de Montréal, Montréal, Québec, Canada.
Correspondence Address:
Sung-Joo Yuh
Department ofNeurosurgery, Centre Hospitalier de l’Université de Montréal, Montréal, Québec, Canada.
DOI:10.25259/SNI_479_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sung-Joo Yuh1,2, Zhi Wang3, Ghassan Boubez3, Daniel Shedid2. Hemiparesis resulting from an unusual C1 fracture: A case report and literature review. 22-Dec-2020;11:449
How to cite this URL: Sung-Joo Yuh1,2, Zhi Wang3, Ghassan Boubez3, Daniel Shedid2. Hemiparesis resulting from an unusual C1 fracture: A case report and literature review. 22-Dec-2020;11:449. Available from: https://surgicalneurologyint.com/surgicalint-articles/10473/
Abstract
Background: Jefferson fractures are burst fractures involving both the anterior and posterior arches of C1. They typically result from axial compression or hyperextension injuries. Most are stable, and neurological deficits are rare. They are often successfully treated with external immobilization, but require surgery (e.g., fusion/ stabilization).
Case Description: An 89-year-old male presented with a left-sided hemiplegia following a trivial fall. The cervical computed tomography scan revealed a left-sided displaced comminuted C1 fracture involving the arch and lateral mass. The MR revealed posterior cord compression and focal myelomalacia. Six months following an emergent C1–C3 decompression with occiput to C4 instrumented fusion, the patient was neurologically intact and pain-free.
Conclusion: An 89-year-old male presented with a left-sided hemiplegia due to a Type 3/4 C1 Jefferson fracture. Following posterior C1–C3 surgical decompression with C0–C4 instrumented fusion, the patient sustained a complete bilateral motor recovery.
Keywords: C1, Central cord syndrome, Cervical fracture, Jefferson fracture
INTRODUCTION
Jefferson fractures are burst fractures involving both the anterior and posterior arches of C1; they account for 2–13% of all cervical fractures.[
The majority of C1 fractures are stable (e.g., with unruptured transverse ligaments) in neurologically intact patients and can be treated with external immobilization alone.[
Here, we present an 89-year-old male, who following trivial trauma, sustained a left-sided C1 Jefferson fracture, resulting in hemiplegia. This was successfully managed with a C1–C3 surgical decompression and C0–C4 instrumented fusion.
CASE REPORT
Following a trivial fall, an 89-year-old right handed male with hypertension, chronic renal failure, and orthostatic hypotension, acutely presented with a flaccid left-sided hemiplegia. He complained of severe neck pain, a limited range of cervical motion, and left lower extremity Lhermitte’s signs (e.g., “electric-like/lightening sensations”). On examination, he was hemiplegic in the left upper (0/5) and lower extremity (1/5) (e.g. the right sided weakness was mild (4/5) in these distributions) and had intact sensory and sphincter function. After 1 hour in the emergency room, his left upper extremity paralysis improved to a 1–2/5 strength level.
Radiologic imaging
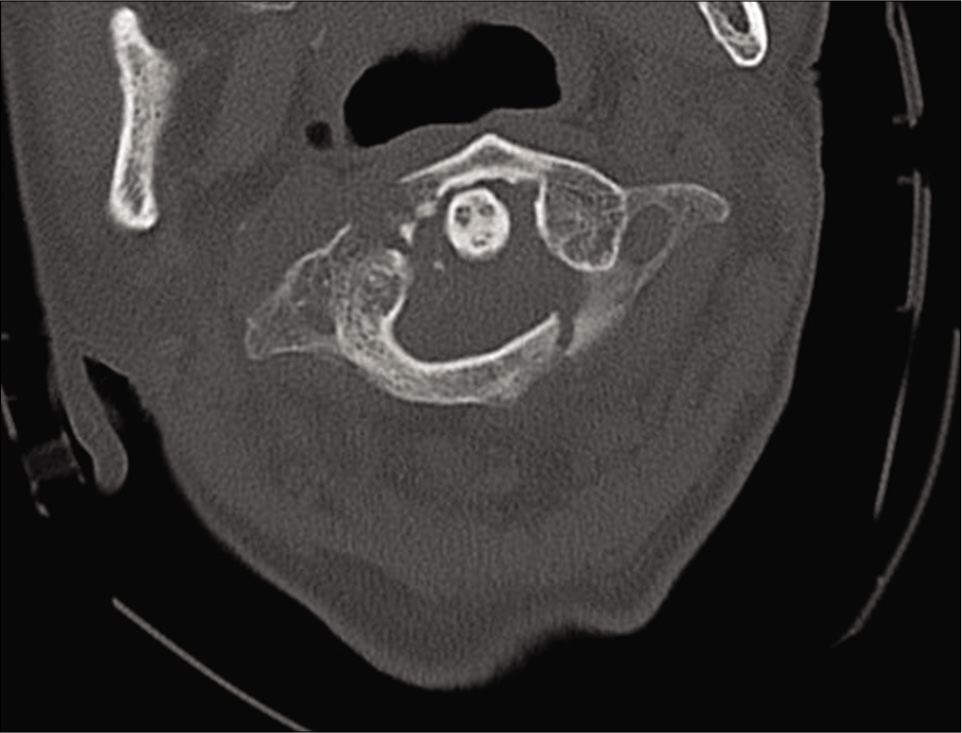
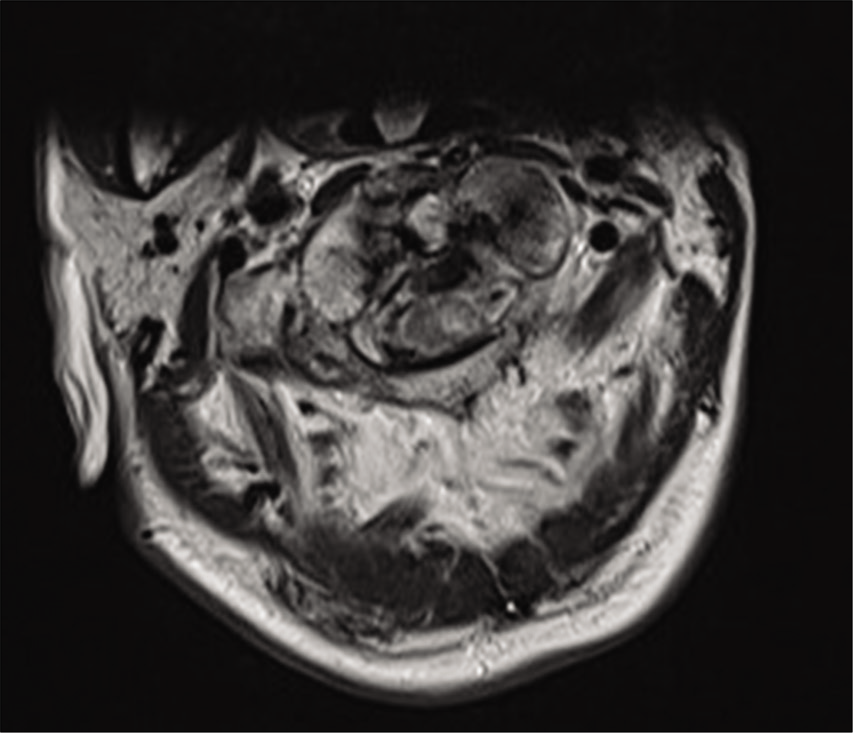
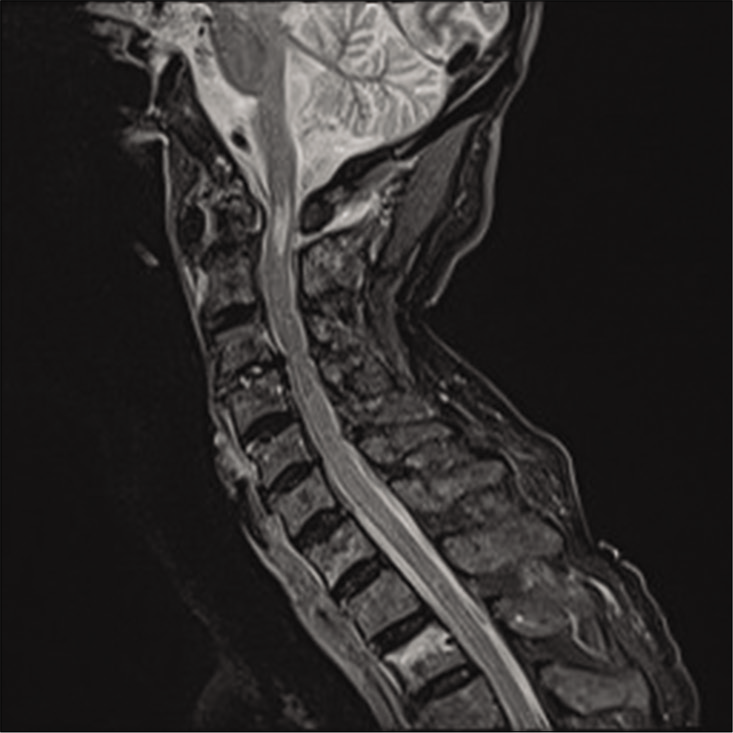
The cervical CT revealed a displaced comminuted C1 arch fracture on the left that involved the left lateral mass of C1 there was an accompanying diathesis of 10 mm [
Surgery
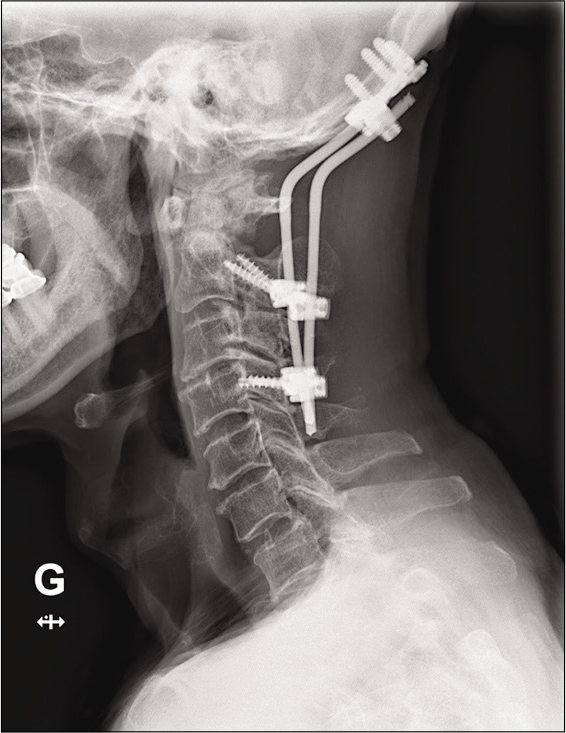
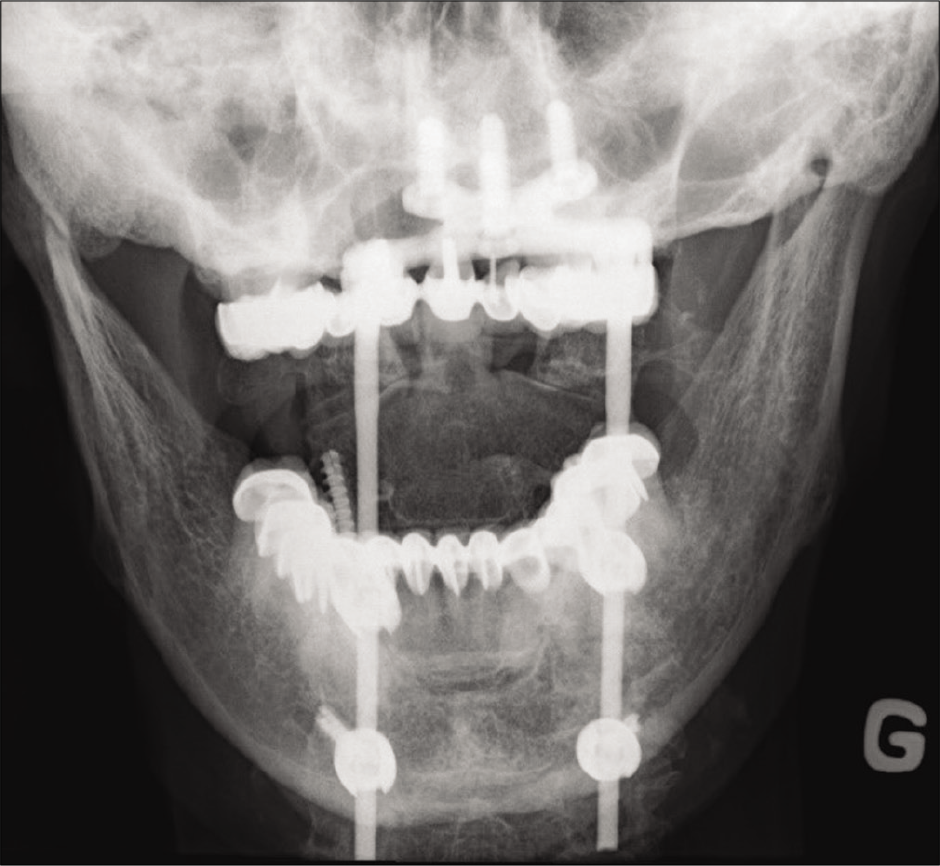
The patient underwent an emergent C1–C3 laminectomy with occiput (CO)–C4 instrumented fusion. Under fluoroscopy, bilateral C1 lateral mass screws, bilateral C2 pars interarticular screws, and C4 lateral mass screws were applied; no C3 lateral mass screws could be placed due to technical interference from the C2 screw heads. Occipital plates/rods were placed bilaterally from C0-C4 [
Postoperative course
Immediately postoperatively, the patient regained strength in both his upper and lower extremities (4/5). He was discharged to a rehabilitation facility 14 days later without any residual deficits. Six months postoperatively, his neck pain resolved, and X-rays showed no subsequent instrument-related complications.
DISCUSSION
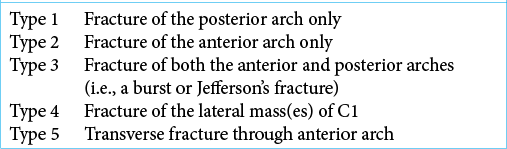
C1 atlas factures can be divided into five different types based on the fracture location patterns[
Here, the initial CT scan showed a fracture of the left lateral mass involving the anterior arch, and a single fracture of the right-sided posterior arch. There was also an associated left occipital condyle fracture. This constituted a Type 3/4 C1 fracture [
Neck pain is the most common presentation for C1 Jefferson fractures, as these fractures typically do not present with neurological deficits; the large diameter of the spinal canal is further widened by the centrifugal displacement of the fragments.[
The integrity of the transverse ligament determines the stability of Jefferson fractures.[
CONCLUSION
After a fall, an 89-year-old male presented with a Type 3/4 C1 Jefferson fracture that resulted in an acute left-sided flaccid hemiplegia. Following a C1–C3 laminectomy and CO–C4 fusion, the patient fully recovered.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bransford R, Falicov A, Nguyen Q, Chapman J. Unilateral C-1 lateral mass sagittal split fracture: An unstable Jefferson fracture variant. J Neurosurg Spine. 2009. 10: 466-73
2. Haus BM, Harris MB. Case report: Nonoperative treatment of an unstable Jefferson fracture using a cervical collar. Clin Orthop Relat Res. 2008. 466: 1257-61
3. Hu Y, Yuan ZS, Kepler CK, Dong WX, Sun XY, Zhang J. Comparison of occipitocervical and atlantoaxial fusion in treatment of unstable Jefferson fractures. Indian J Orthop. 2017. 51: 28-35
4. Kumar A, Onggo J, Fon LH, Oh J. Direct fixation of C1 Jefferson fracture using C1 lateral mass screws: A case report. Int J Spine Surg. 2019. 13: 345-9
5. Lleu M, Charles YP, Blondel B, Barresi L, Nicot B, Challier V. C1 fracture: Analysis of consolidation and complications rates in a prospective multicenter series. Orthop Traumatol Surg Res. 2018. 104: 1049-54
6. Marcon RM, Cristante AF, Teixeira WJ, Narasaki DK, Oliveira RP, de Barros Filho TE. Fractures of the cervical spine. Clinics (Sao Paulo). 2013. 68: 1455-61
7. Ryken TC, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ. Management of isolated fractures of the atlas in adults. Neurosurgery. 2013. 72: 127-31