- Departments of Neurosurgery, Baylor College of Medicine, Houston, Texas, United States,
- Pathology, Baylor College of Medicine, Houston, Texas, United States,
- Neurology, Baylor College of Medicine, Houston, Texas, United States.
Correspondence Address:
Rita Snyder, Department of Neurosurgery, Baylor College of Medicine, Houston, Texas, United States.
DOI:10.25259/SNI_886_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rita Snyder1, Sungho Lee1, Kent Heck2, Jacob J. Mandel3, Akash J. Patel1, Ali Jalali1. Hemorrhagic cavum vergae colloid cyst: A presentation of anterograde amnesia without hydrocephalus. 15-Apr-2022;13:148
How to cite this URL: Rita Snyder1, Sungho Lee1, Kent Heck2, Jacob J. Mandel3, Akash J. Patel1, Ali Jalali1. Hemorrhagic cavum vergae colloid cyst: A presentation of anterograde amnesia without hydrocephalus. 15-Apr-2022;13:148. Available from: https://surgicalneurologyint.com/surgicalint-articles/11535/
Abstract
Background: Colloid cysts characteristically arise from the roof of the third ventricle near the foramen of Monro, causing symptoms from obstructive hydrocephalus. However, atypical locations have been reported with various clinical presentations, growth patterns, and displacement of surrounding anatomic structures.
Case Description: Here, we describe the interesting case of a patient with a large hemorrhagic cavum vergae colloid cyst presenting with anterograde amnesia soon after starting antiplatelet therapy. The patient did not have hydrocephalus on presentation and his amnesia persisted after complete removal of the hemorrhagic mass through transcallosal interforniceal approach.
Conclusion: To the best of our knowledge, this is the only reported instance of a colloid cyst presenting with amnesia in the absence of hydrocephalus. Pathophysiology as well as diagnostic and management strategies of hemorrhagic colloid cysts are discussed.
Keywords: Cavum vergae, Colloid cyst, Microsurgery
INTRODUCTION
Colloid cysts are unusual entities, with an annual incidence of 3.2 cases/1 million.[
CASE REPORT
A 65-year-old male presented to the emergency center with 2 weeks of anterograde amnesia and related confusion, one episode of urinary incontinence, and gradual functional decline including worsening of his baseline ataxic gait. His medical history included obesity, hypertension, nonalcoholic fatty liver disease, diabetes mellitus type II, congestive heart failure, and coronary artery disease with a recent coronary stent placement and start of dual antiplatelet therapy 3 weeks before presentation. Other than impaired word recall, he had no focal deficits on neurological examination. However, initial CT imaging of the head revealed a heterogeneously hyperdense, lobulated mass in the area of the posterior septum pellucidum measuring 2.8 cm in diameter without any evidence of hydrocephalus [
Figure 1:
Noncontrast axial CT image demonstrates heterogeneously hyperdense mass within the septum pellucidum (a). Axial T2-weighted MRI image demonstrates location of the hemorrhagic lesion posterior to the columns of the fornix within the cavum vergae (b). Coronal (c) and sagittal contrasted T1-weighted MRI images demonstrate patent foramen of Monro (d) lateral displacement of internal cerebral veins (e) and thalami bilaterally.
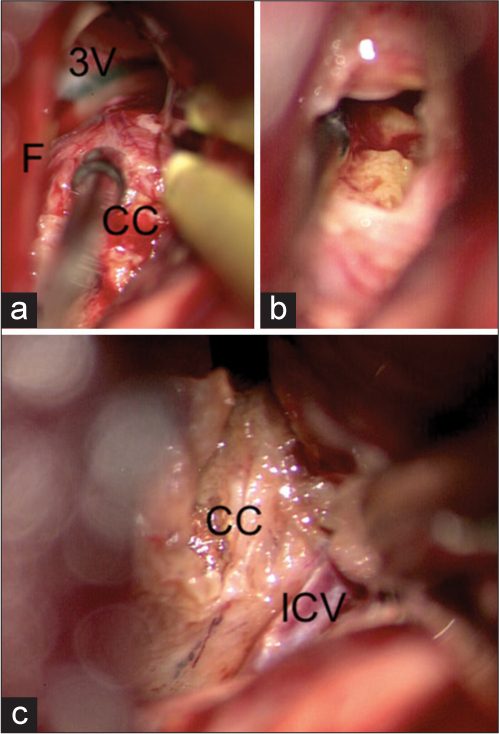
The cystic mass was encountered immediately after the callosotomy. It displaced the fornices laterally but did not extend into the third ventricle [
Figure 2:
Colloid cyst displaced the fornices laterally and did not extend into the 3rd ventricle (a). Xanthochromic, mucinous contents of the colloid cyst (b). Adherence of the cyst wall to the internal cerebral vein (c). 3V: 3rd ventricle, CC: Colloid cyst, F: Fornix, and ICV: Internal cerebral vein.
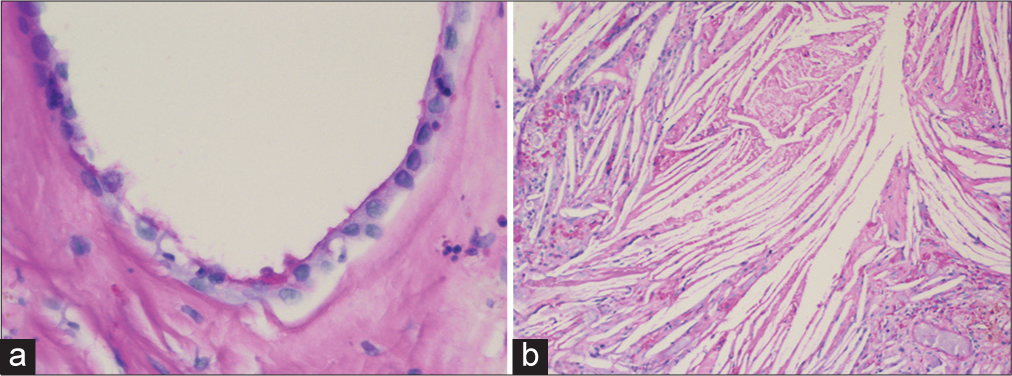
On pathology, the cyst was found to be lined by a simple layer of cuboidal cells which were sparsely ciliated and diffusely positive for epithelial markers epithelial membrane antigen and cytokeratin [
At 6-month clinic follow-up, he was able to carry out routine self-care activities and conversation although his residual anterograde amnesia and baseline comorbidities kept him relatively sedentary and dependent on family for overall care.
DISCUSSION
Hemorrhagic colloid cysts are highly unusual, with <20 cases and five autopsy reports in the literature to date.[
Colloid cysts appear hyperdense on CT imaging, and therefore, hemorrhage cannot be ruled out until an MRI is obtained.[
CONCLUSION
This is the first report of a hemorrhagic cavum vergae colloid cyst presenting with anterograde amnesia without hydrocephalus. We hypothesize that the mass underwent accelerated hemorrhagic expansion after the recent initiation of dual antiplatelet therapy, and the resultant stretch injury on bilateral fornices in the absence of hydrocephalus was responsible for the anterograde amnesia on presentation.
Hemorrhagic colloid cysts are rare entities which can occur in unusual locations. Anterograde amnesia from forniceal stretch injury can occur from a rapidly increasing local mass effect or acute hydrocephalus. Expedited management and microsurgical approach are favored.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al Abdulsalam HK, Ajlan AM. Hemorrhagic colloid cyst. Neurosciences. 2018. 23: 326-33
2. Al-Saiari SA, Abdoh MG, Farag AA, Al-Orabi KM, Rawah EA, Brinji ZS. Atypical haemorrhagic colloid cyst: 2 case reports surgical management and review of literature. Int J Surg Case Rep. 2020. 76: 435-40
3. Azab WA, Salaheddin W, Alsheikh TM, Nasim K, Nasr MM. Colloid cysts posterior and anterior to the foramen of Monro: Anatomical features and implications for endoscopic excision. Surg Neurol Int. 2014. 5: 124
4. Carrasco R, Pascual JM, Medina-López D, BurdaspalMoratilla A. Acute hemorrhage in a colloid cyst of the third ventricle: A rare cause of sudden deterioration. Surg Neurol Int. 2012. 3: 24
5. Hadar EJ, Schmunk GA, Salamat MS. Hemorrhagic colloid cyst in a patient with leukemia. J Neurosurg. 1999. 91: 516
6. Inci S, Al-Rousan N, Söylemezoglu F, Gurçay O. Intrapontomesencephalic colloid cyst: An unusual location. J Neurosurg. 2001. 94: 118-21
7. Menon G, Kongwad LI, Nair RP, Kumar V. Hemorrhagic colloid cyst. Neurol India. 2017. 65: 1164-7
8. Ogbodo E, Kaliaperumal C, Bermingham N, O’Sullivan M. Spontaneous haemorrhage and rupture of third ventricular colloid cyst. BMJ Case Rep. 2012. 2012: bcr2012006863
9. Sivakumaran R, Edwards RJ. Amnesia due to spontaneous haemorrhage into a colloid cyst. Br J Neurosurg. 2015. 29: 110-1
10. Tamura Y, Uesugi T, Tucker A, Ukita T, Tsuji M, Miyake H. Hemorrhagic colloid cyst with intraventricular extension. J Neurosurg. 2013. 118: 498-501