- Department of Pharmacology,Translational Neurology Research Group, Medical School of Athens, Athens, Greece.
- Department of Neurosurgery, Korgialenio, Benakio, HRC General Hospital of Athens, Athens, Greece.
- Department of Neurology, “Evaggelismos” General Hospital of Athens, Athens, Greece.
- Laboratory of Experimental Surgery and Surgical Research, University of Athens, Athens, Greece.
- Department of Neurosurgery, “Evaggelismos” General Hospital of Athens, Athens, Greece.
Correspondence Address:
Nikolaos Plakopitis, Department of Pharmacology, Translational Neurology Research Group,Medical School of Athens, Athens, Greece.
DOI:10.25259/SNI_415_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nikolaos Plakopitis1, Konstantinos Themistoklis2, Konstantinos Melanis3, Eleftherios Spartalis4, Panayiotis Patrikelis5, Themistoklis Papasilekas2. Hemorrhagic complications after removal of an external ventricular drain: A case report and literature review. 25-Aug-2023;14:298
How to cite this URL: Nikolaos Plakopitis1, Konstantinos Themistoklis2, Konstantinos Melanis3, Eleftherios Spartalis4, Panayiotis Patrikelis5, Themistoklis Papasilekas2. Hemorrhagic complications after removal of an external ventricular drain: A case report and literature review. 25-Aug-2023;14:298. Available from: https://surgicalneurologyint.com/surgicalint-articles/12515/
Abstract
Background: External ventricular drainage (EVD) is one of the most common neurosurgical procedures. Complications are rather rare and mostly include hemorrhage and infection. Hematomas may form during placement or even after the removal of an EVD. Regarding the latter, the literature is scarce, with only nine clinically significant cases reported.
Case Description: We present the case of a young woman who suffered an extensive hemorrhage after removal of an EVD, in the setting of a posterior fossa stroke. We discuss the management and possible consequences of such an event and we emphasize the need for alertness to avoid such complications.
Conclusion: Removal of an EVD is a safe procedure, with rare cases of hemorrhagic complications being reported. A case of a large hematoma that formed after the removal of an EVD is presented. Stricter follow-up protocols should be implemented to better estimate the risk of hemorrhage.
Keywords: External ventricular drainage, External ventricular drainage removal, Hemorrhage, Ventriculostomy
INTRODUCTION
Placement of an external ventricular drainage (EVD) is arguably one of the most common and important life-saving procedures in neurosurgery.[
When Dandy introduced the technique of bedside ventriculostomy in his landmark paper, back in 1918, he confidently stated that the procedure was complication-free in experienced hands.[
The scope of this article is to describe the case of a young female stroke patient who suffered a major intracerebral hemorrhage after an EVD removal. We also present a brief review of the relevant literature. To the best of our knowledge, there are only eight other cases in the literature of clinically significant or large hematomas associated with the removal of an EVD.[
CASE REPORT
A 44-year-old woman with an unremarkable medical history presented at the emergency department of our hospital due to acute onset gait imbalance accompanied by vertigo. Symptoms had already been present for several hours before her admission. On neurological examination, she was found to be confused, with a wide-based ataxic gait as well as right-sided dysmetria and dysdiadochokinesia. Dysarthria and right-beating nystagmus were also noted (National Institutes of Health Stroke Scale-5). A brain magnetic resonance imaging scan with IV contrast revealed ischemia of the right cerebellar hemisphere. Further, workup, including an ultrasound of the carotid and vertebral arteries, a heart ultrasound, a brain, and cervical area computed tomography (CT) angiogram as well as a cerebral digital subtraction angiography, revealed no other underlying pathology. Her vital signs on presentation were recorded as respiratory rate 15, blood pressure (BP) 155/95 mmHg, pulse rate 88 bpm, oxygen saturation 99%, and T 37.0°C.
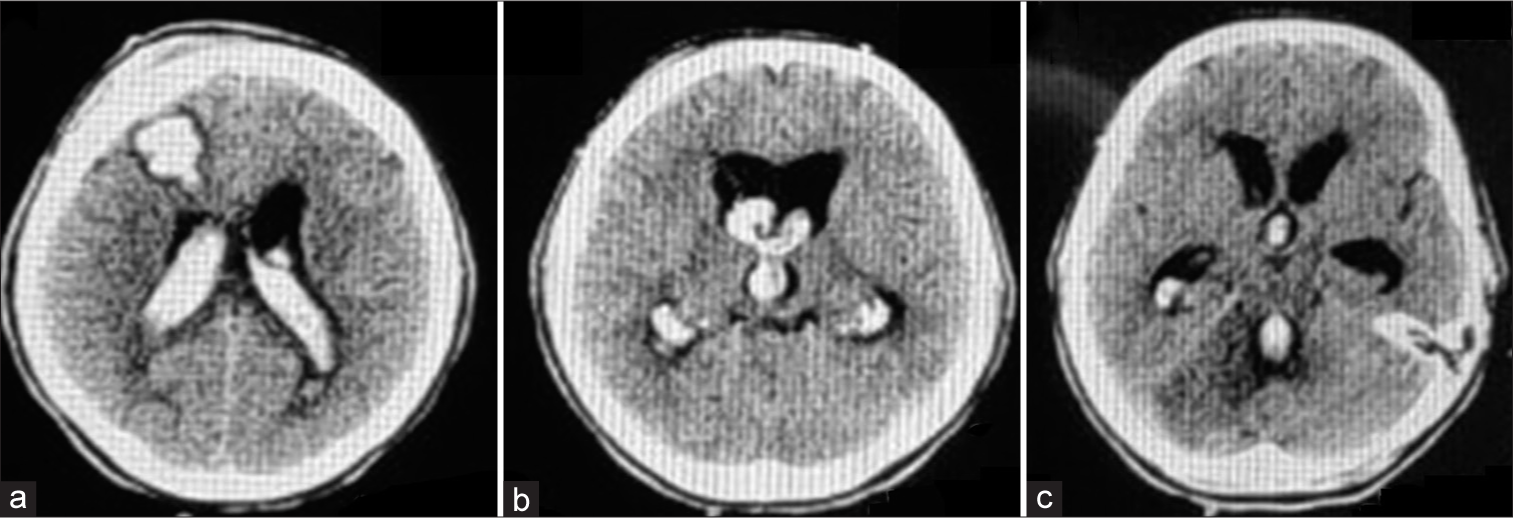
Deemed outside the time frame for thrombolysis and with no thrombectomy service available on site, the patient was started on aspirin and rosuvastatin (secondary stroke prevention) and she was transferred to the neurological ward where she remained for the next 48 h, essentially unchanged. Of note, her BP throughout this initial period remained within normal limits ruling out hypertension as the underlying cause of the bleeding. However, on day 3 of her admission, the patient gradually became unresponsive. An emergency brain CT scan revealed acute obstructive hydrocephalus with dislocation of the fourth ventricle due to edema around the ischemic lesion. No significant brainstem compression was noted. As a result, the patient was intubated and an EVD was put in place at the OR. Aspirin was discontinued due to the intervention and she was moved to the intensive care unit for further hospitalization. Three days later, she was extubated and on day 7, after successful weaning, the EVD was scheduled to be removed. Her vital signs and blood tests were all within normal range. Due to a busy schedule on that particular day, the EVD was left for the on-call resident to take out; after all elective procedures would be complete. Removal was performed as per standard protocol, on the bedside. On completion of the procedure, the patient immediately complained of a headache and within the following hour, she fell into a stupor. She was again intubated with a new brain CT scan showing obstructive hydrocephalus due to hemorrhage extending along the EVD track and down to the lateral and third ventricles [
DISCUSSION
Even though EVD removal is generally considered to be a technically simple and safe procedure, there have been reports in the literature of hemorrhage complications and even deaths following such a maneuver. An EVD-associated hemorrhage is characterized as clinically significant in all cases that a patient suffers a temporospatially related neurological deterioration. Obviously, this depends on the extent of the hemorrhage and also on its exact location. The latter is fairly constant in EVD cases and in close proximity to Kocher’s point, the presence or absence though of intraventricular extension significantly alters prognosis.[
Clinically, significant hemorrhages following an EVD removal, although rare, do often require intervention. In general, ventriculostomy revision with insertion of a new EVD at either the ipsilateral or contralateral side is the treatment of choice while clot evacuation is indicated when its intraparenchymal component is of a sufficient size.[
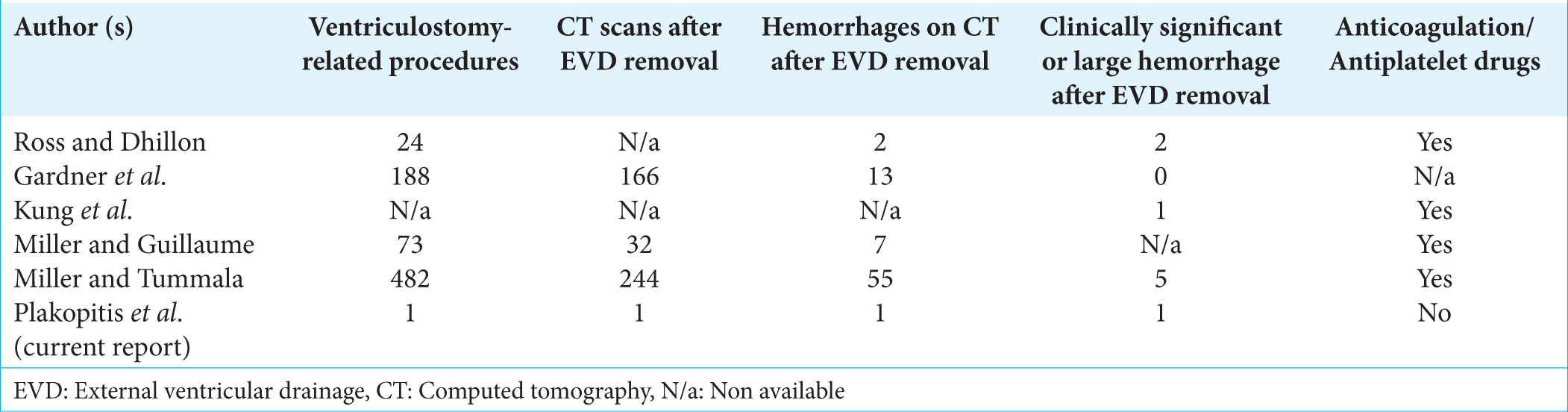
To the best of our knowledge, there are only five other articles in the literature referring to post EVD removal hemorrhages [
Extrapolating data from the aforementioned studies, EVD removal carries an overall bleeding risk ranging from 7.8% to 22.5%, while the risk for clinically significant and/or large hemorrhages ranges from 0% to 2%. The mortality rate due to hemorrhages after EVD removal ranges between 0% and 0.2%. Notably, no uniform hemorrhage evaluation protocol has been applied with most patients only scanned on the indication of new symptoms (i.e., patients with small-scale hematomas may have been missed). It is thus safe to assume that the incidence of this kind of hemorrhages has been miscalculated and only routine post EVD removal imaging will help us extrapolate proper data.
Before closing, it should be underlined that an often overlooked consequence of EVD-related hemorrhages is their potential to act as an epileptogenic site.[
CONCLUSION
As already mentioned, the removal of an EVD is considered to be both safe and simple. In rare cases however, there can be complications with hemorrhage being the most serious one. To the best of our knowledge, this is the ninth report of clinically significant such hemorrhage, with another eight cases reported in five articles. Since the above-described incident in our department, we have altered our protocol to carry out EVD removals in an operation room (OR) setting. Furthermore, although no one felt that what happened had anything to do with our trainee’s actions, we have rearranged the training curriculum to put special emphasis on EVD management for our junior residents. To better estimate the risk of hemorrhage during an EVD removal and its impact on the final outcome, we believe that stricter follow-up protocols need to be implemented in clinical practice.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Dandy WE. Ventriculography following the injection of air into the cerebral ventricles. Ann Surg. 1918. 68: 5-11
2. Gardner PA, Engh J, Atteberry D, Moossy JJ. Hemorrhage rates after external ventricular drain placement. J Neurosurg. 2009. 110: 1021-5
3. Kung DK, Policeni BA, Capuano AW, Rossen JD, Jabbour PM, Torner JC. Risk of ventriculostomy-related hemorrhage in patients with acutely ruptured aneurysms treated using stent-assisted coiling. J Neurosurg. 2011. 114: 1021-7
4. Miller C, Guillaume D. Incidence of hemorrhage in the pediatric population with placement and removal of external ventricular drains. J Neurosurg Pediatr. 2015. 16: 662-7
5. Miller C, Tummala RP. Risk factors for hemorrhage associated with external ventricular drain placement and removal. J Neurosurg. 2017. 126: 289-97
6. Ross IB, Dhillon GS. Ventriculostomy-related cerebral hemorrhages after endovascular aneurysm treatment. AJNR Am J Neuroradiol. 2003. 24: 1528-31