- Department of Neurosurgery, Chiba Hokusoh Hospital, Nippon Medical School, Inzai, Chiba, Japan.
Correspondence Address:
Kyongsong Kim, Department of Neurosurgery, Chiba Hokusoh Hospital, Nippon Medical School, Inzai, Chiba, Japan.
DOI:10.25259/SNI_408_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kenta Koketsu, Kyongsong Kim, Minoru Ideguchi, Rinko Kokubo, Takayuki Mizunari, Akio Morita. High-flow bypass surgery using a radial artery graft for an extracranial internal carotid artery aneurysm: Case reports and literature review. 06-Jul-2021;12:333
How to cite this URL: Kenta Koketsu, Kyongsong Kim, Minoru Ideguchi, Rinko Kokubo, Takayuki Mizunari, Akio Morita. High-flow bypass surgery using a radial artery graft for an extracranial internal carotid artery aneurysm: Case reports and literature review. 06-Jul-2021;12:333. Available from: https://surgicalneurologyint.com/surgicalint-articles/10945/
Abstract
Background: Extracranial carotid artery aneurysms are rare. Surgery may be difficult when vessels are tortuous and on a high cervical level. We report two patients whose tortuous extracranial internal carotid artery (ICA) aneurysm located on a high cervical level was successfully treated by ICA ligation and a high-flow bypass using a radial artery (RA) graft between the external carotid- and the middle cerebral artery.
Case Description: (Case 1) A 47-year-old man suffered a recurrent cerebral infarct despite medical treatment. His right extracranial ICA aneurysm measured 33 mm; it was tortuous and located at a high cervical level. We ligated the ICA after placing a high-flow bypass using an RA graft. The aneurysm was not repaired. (Case 2) A 59-year-old woman noticed pulsatile swelling on her left neck. It was due to an extracranial ICA aneurysm that was large (36 mm), tortuous, and located at a high cervical level. We performed ICA ligation after placing a high-flow bypass using an RA graft without direct aneurysmal repair. Six months after the operation she noted a pulsatile bulge on the left oropharynx. We confirmed recurrence of an aneurysm from retrograde blood flow and performed internal trapping by occluding the distal portion of the ICA aneurysm using an intravascular procedure.
Conclusion: ICA ligation after placing a high-flow bypass with an RA-graft is a technically demanding, but safe procedure to address extracranial ICA aneurysms that are tortuous and located at a high cervical level.
Keywords: Aneurysm, Bypass surgery, Extracranial internal carotid artery, Radial artery graft
INTRODUCTION
Extracranial carotid artery aneurysms constitute fewer than 1% of all aneurysms.[
CASE REPORT
Case 1
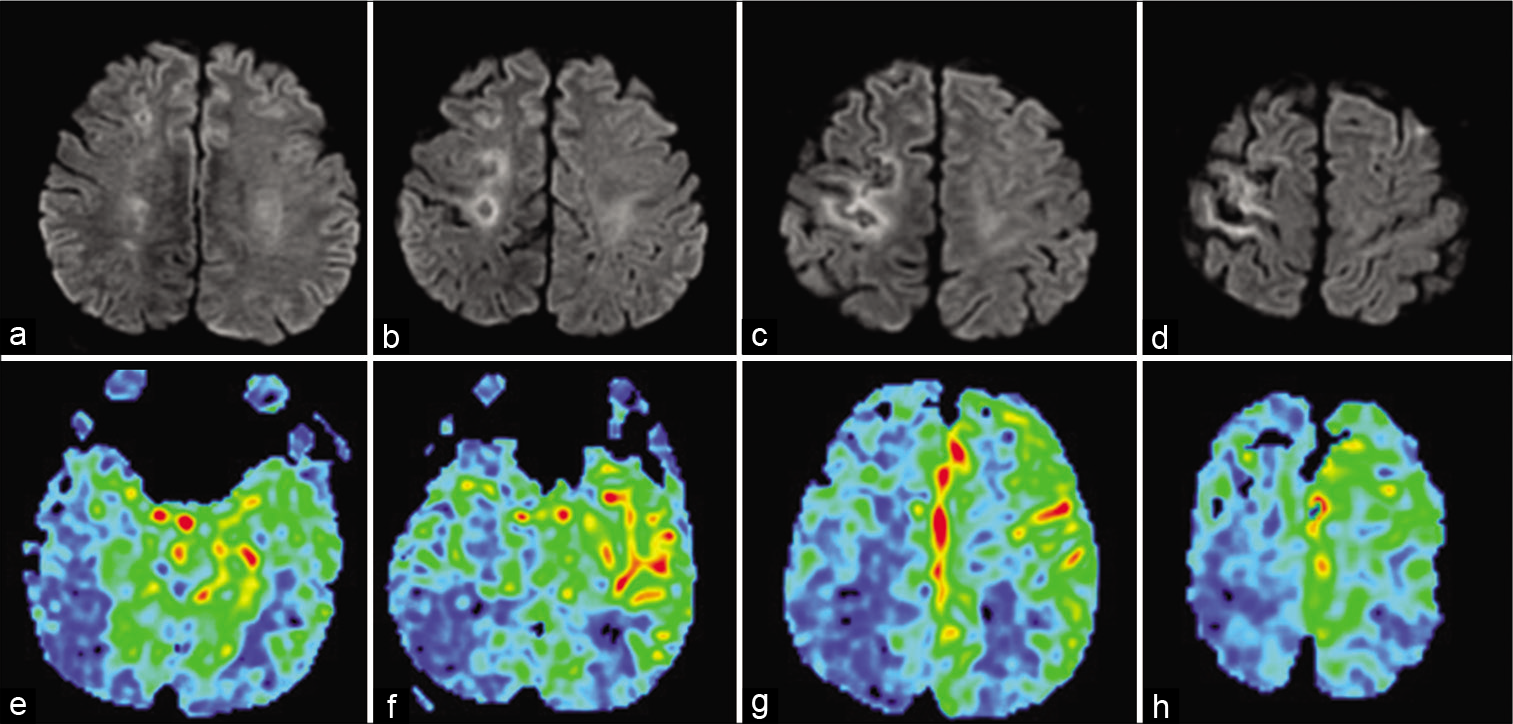
This 47-year-old man had suffered left hemiparesis due to a cerebral infarct at the right MCA 9 years earlier. The diagnosis was thrombo-embolism from a right extracranial ICA aneurysm and antiplatelet treatment was started. He developed left hemiparesis and was admitted to a local hospital. Brain magnetic resonance imaging (MRI) revealed a cerebral infarct in the right MCA territory and heparinization was added. However, his paresis worsened due to progression of the infarct. On the 22nd day after admission, he was transferred to us. On admission, left hemiparesis (3~4/5; MMT) was observed. Brain MRI revealed a subacute cerebral infarct in the MCA territory; perfusion MRI showed hypoperfusion of the right hemisphere [
Figure 2:
(Case 1) Cervical axial computed tomography scans (a and b) show a 33-mm extracranial carotid artery aneurysm (white arrow). The upper end of the aneurysm (a) is at the mandibular level. The left carotid artery angiogram (c, lateral view) shows an internal carotid artery (ICA) aneurysm with an irregular wall at the C2 level. (d) Postoperative angiogram confirming ICA occlusion and disappearance of the aneurysm and patency of the radial artery graft (arrowhead).
Postoperatively, there was no neurological deterioration; brain MRI showed no new cerebral infarction. Cerebral angiography confirmed right ICA occlusion and disappearance of the aneurysm [
Case 2
This 59-year-old woman had noticed pulsative swelling on the left neck 4 months earlier. She underwent cervical 3D-computed tomography-angiography; the presence of an extracranial ICA aneurysm was suspected and she was transferred to our hospital. She presented with no obvious neurological deficits. Brain MRI showed no lesion, however, perfusion MRI revealed hypo-perfusion in the left hemisphere [
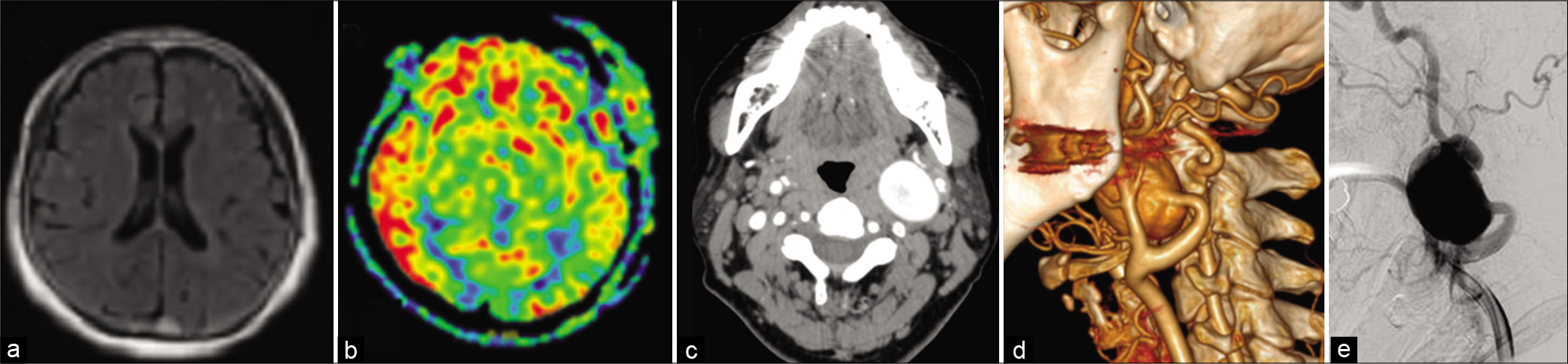
Figure 3:
(Case 2) T2-FLAIR magnetic resonance imaging (MRI) axial image (a) shows no abnormal lesion. MRI perfusion images (b) reveal hypo-perfusion in the left cerebral hemisphere. Cervical computed tomography angiograms (c and d) and a left carotid artery angiogram (e) reveal a 36-mm left extracranial internal carotid artery aneurysm the level of C1 to C3. Part of the aneurysm is behind the mandible.
After surgery, she suffered left incomplete facial nerve palsy (House-Brackmann Grade II) due to local injury. Brain MRI showed no ischemic lesion, and confirmed patency of the high-flow bypass without blood flow from the proximal portion of the ICA. She was discharged 18 days after the operation. However, 6 months after the operation, she noted a pulsatile bulge on the left oropharynx although her facial nerve paralysis had disappeared. A cerebral angiogram from the RA graft showed that the aneurysm was fed retrogradely in the delayed phase. We trapped the aneurysm by occluding the distal portion of the ICA intravascularly [
DISCUSSION
Open repair is the gold-standard treatment for ECA aneurysms. The potential risks posed by surgery are unwanted embolization, difficulties with distal control, and injury to surrounding vital structures. The reported postoperative mortality rate was 2.2–6.0%, morbidity due to neurological complications was 5.5–10% and included fatal stroke.[
As RA grafts are usually placed at a layer shallower than the parallel-running ECA in the cervical region, it is difficult to address extracranial ICA aneurysms with RA grafts. Preoperative images confirmed that in our patients, the aneurysms were not located at sites where an RA graft would normally be placed. This point must be confirmed on preoperative images before our treatment strategy can be implemented. In both of our patients, our approach was successful without serious postoperative sequelae.
Some extracranial carotid artery aneurysms can be addressed endovascularly.[
CONCLUSION
Our patients with tortuous extracranial carotid artery aneurysms that were located on a high cervical level were successfully treated by ICA ligation and the placement of a high-flow bypass using a RA-graft.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Drescher F, Weber W, Berlis A, Rohde S, Carolus A, Fischer S. Treatment of intra-and extracranial aneurysms using the flow-redirection endoluminal device: Multicenter experience and follow-up results. AJNR Am J Neuroradiol. 2017. 38: 105-12
2. El-Sabrout R, Cooley DA. Extracranial carotid artery aneurysms: Texas heart institute experience. J Vasc Surg. 2003. 31: 702-12
3. Faggioli GL, Freyrie A, Stella A, Pedrini L, Gargiulo M, Tarantini S. Extracranial internal carotid artery aneurysms: Results of a surgical series with long-term follow-up. J Vasc Surg. 1996. 23: 587-94
4. Fankhauser GT, Stone WM, Fowl RJ, O’Donnell ME, Bower TC, Meyer FB. Surgical and medical management of extracranial carotid artery aneurysms. J Vasc Surg. 2015. 61: 389-93
5. Fischer S, Perez MA, Kurre W, Albes G, Bäzner H, Henkes H. Pipeline embolization device for the treatment of intra-and extracranial fusiform and dissecting aneurysms: Initial experience and long-term follow-up. Neurosurgery. 2014. 75: 364-74
6. Hamasaki R, Yanagisawa T, Takahashi Y, Shimizu H. Surgical treatment of cervical carotid artery aneurysm. No Shinkei Geka. 2017. 45: 677-83
7. Jin J, Liu Y, Shen X, Bai J, Qu L. Endovascular and hybrid interventions for extracranial juxta-skullbase carotid artery aneurysms: Experience and long-term results. J Stroke Cerebrovasc Dis. 2021. 30: 105611
8. Kraemer CJK, Zhou W. Carotid aneurysm review. Int J Angiol. 2019. 28: 17-9
9. Li Z, Chang G, Yao C, Guo L, Liu Y, Wang M. Endovascular stenting of extracranial carotid artery aneurysm: A systematic review. Eur J Vasc Endovasc Surg. 2011. 42: 419-26
10. Mizunari T, Murai Y, Kim K, Kobayashi S, Kamiyama H, Teramoto A. Posttraumatic carotid-cavernous fistulae treated by internal carotid artery trapping and high-flow bypass using a radial artery graft-two case reports. Neurol Med Chir (Tokyo). 2011. 51: 113-6
11. Radak D, Davidovic L, Vukobratov V, Illijevski N, Kostic D, Maksimovic S. Carotid artery aneurysms: Serbian multicentric study. Ann Vasc Surg. 2007. 21: 23-9
12. Rosset E, Albertini JN, Magnan PE, Ede B, Thomassin JM, Branchereau A. Surgical treatment of extracranial internal carotid artery aneurysms. J Vasc Surg. 2000. 31: 713-23
13. Xue S, Tang X, Zhao G, Tang H, Shen Y, Yang YE. Contemporary outcomes of open and endovascular intervention for extracranial carotid artery aneurysms: A single center experience. Eur J Vasc Endovasc Surg. 2020. 60: 347-54