- Department of Neuroscience, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
Correspondence Address:
Nancy E. Epstein
Department of Neuroscience, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
DOI:10.4103/2152-7806.191070
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Epstein NE. High neurological complication rates for extreme lateral lumbar interbody fusion and related techniques: A review of safety concerns. Surg Neurol Int 22-Sep-2016;7:
How to cite this URL: Epstein NE. High neurological complication rates for extreme lateral lumbar interbody fusion and related techniques: A review of safety concerns. Surg Neurol Int 22-Sep-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/high-neurological-complication-rates-extreme-lateral-lumbar-interbody-fusion-related-techniques-review-safety-concerns/
Abstract
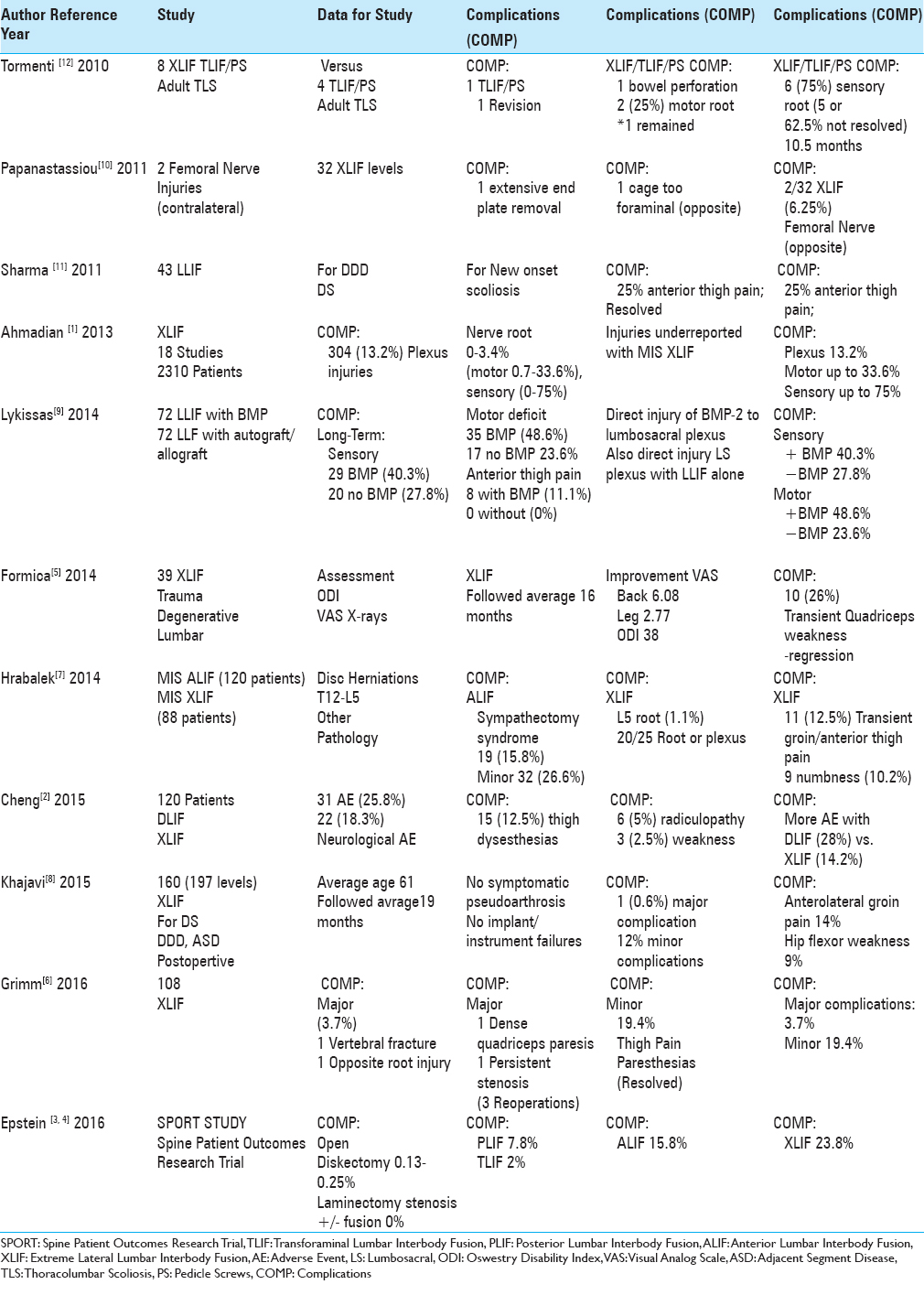
Background:There are frequent reports of lumbosacral plexus and other neurological injuries occurring with extreme lateral interbody fusions (XLIF) and other related lateral lumbar techniques.
Methods:This review focuses on the new neurological deficits (e.g. lumbosacral plexus, root injuries) that occur following minimally invasive surgery (MIS) XLIF and other related lateral lumbar techniques.
Results:A review of multiple articles revealed the following ranges of new postoperative neurological complications for XLIF procedures: plexus injuries 13.28%; sensory deficits 0–75% (permanent in 62.5%); motor deficits 0.7–33.6%; anterior thigh pain 12.5–25%. Of interest, in a study by Lykissas et al., the frequency of long-term neural injury following lateral lumber interbody fusion (LLIF) with BMP-2 (72 patients) was much higher than for LLIF performed with autograft/allograft (72 patients). The addition of bone morphogenetic protein led to persistent sensory deficits in 29 vs. 20 without BMP; persistent motor deficits in 35 with vs. 17 without BMP; and persistent anterior thigh/groin pain in 8 with vs. 0 without BMP. They should also have noted the unacceptably high incidence of neural injury occurring with LLIF alone without BMP.
Conclusion:This review highlights the high risk of neural injury (up to 75% for sensory, 33.6% for motor, and an overall plexus injury rate of 13.28%) utilizing the XLIF and other similar lateral lumbar approaches. With such extensive neurological injuries, is the XLIF really safe, and should it still be performed?
Keywords: Comparison with other lateral interbody methods, extreme lateral interbody fusion, minimally invasive surgery, neurological complications, open surgery
INTRODUCTION
This review focuses on the frequency of neural injuries resulting from extreme lumbar interbody fusion (XLIF) or similar lateral procedures (e.g., direct lumbar interbody fusion (DLIF) and lateral lumbar interbody fusion (LLIF)). The multiple studies analyzed cited the following ranges of new postoperative neurological complications attributed to XLIF: new sensory deficits 0–75% (permanent 62.5%), new motor deficits 0.7–33.6%, new anterior thigh pain 12.5–25%, and a plexus injury rate of 13.28%. Because it is well-known that the transpsoas approach places the lumbosacral plexus at risk, some authors even concluded these frequent deficits should not be considered “complications,” as they were simply “anticipated” consequences of the procedure. Here, we emphasize the unacceptably high rate of neurological injuries attributed to XLIF and related lateral lumbar procedures, and question whether, with this safety record, it should still be performed?
HIGH FREQUENCY OF NEW NEUROLOGICAL INJURIES WITH XLIF AND RELATED LATERAL LUMBAR PROCEDURES
Multiple authors have reported a high frequency of neurological injuries, including anterior thigh pain, contralateral femoral nerve palsies, new sensory/motor root deficits, and lumbar plexopathies attributed to XLIF and other lateral lumbar procedures. In 2011, Sharma et al. evaluated the 1-year outcomes of 43 LLIF addressing degenerative disc disease (DDD), degenerative spondylolisthesis (DS), or scoliosis; 25% of the patients experienced new postoperative anterior thigh pain [
EXTREME LATERAL INTERBODY FUSION COMPLICATIONS INCREASED WITH THE ADDITION OF BONE MORPHOGENETIC PROTEIN-2
The study by Lykissas et al. in 2014 critically pointed out the potential direct damage of rhMP-2 to the lumbosacral plexus when utilized for LLIF [
COMBINING EXTREME LATERAL INTERBODY FUSION WITH OTHER PROCEDURES FOR ADULT SCOLIOSIS
XLIF procedures combined with additional procedures to address adult scoliosis increased the complication rates [
CONCLUSION
This review focused on the high frequency of neural injuries resulting from XLIF and related lateral lumber interbody procedures. New neurological injuries included sensory deficits in 0–75% of cases (permanent 62.5%), motor deficits in 0.7–33.6% of patients, anterior thigh pain in 12.5–25%, and a 13.28% plexus injury rate. When is the neurological injury rate for XLIF and its related procedures considered unacceptable? And when do we question why, with this safety record, it should still be performed?
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahmadian A, Deukmedjian AR, Abel N, Dakwar E, Uribe JS. Analysis of lumbar plexopathies and nerve injury after lateral retroperitoneal transpsoas approach: Diagnostic standardization. J Neurosurg Spine. 2013. 18: 289-97
2. Cheng I, Briseño MR, Arrigo RT, Bains N, Ravi S, Tran A. Outcomes of Two Different Techniques Using the Lateral Approach for Lumbar Interbody Arthrodesis. Global Spine J. 2015. 5: 308-14
3. Epstein NE. More nerve root injuries occur with minimally invasive lumbar surgery, especially extreme lateral interbody fusion: A review. Surg Neurol Int. 2016. 7: S83-95
4. Epstein NE. More nerve root injuries occur with minimally invasive lumbar surgery: Let's tell someone. Surg Neurol Int. 2016. 7: S96-S101
5. Formica M, Berjano P, Cavagnaro L, Zanirato A, Piazzolla A, Formica C. Extreme lateral approach to the spine in degenerative and post traumatic lumbar diseases: Selection process, results and complications. Eur Spine J. 2014. 23: S684-92
6. Grimm BD, Leas DP, Poletti SC, Johnson DR. Postoperative Complications Within the First Year After Extreme Lateral Interbody Fusion: Experience of the First 108 Patients. Clin Spine Surg. 2016. 29: E151-6
7. Hrabalek L, Adamus M, Gryga A, Wanek T, Tucek P. A comparison of complication rate between anterior and lateral approaches to the lumbar spine. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014. 158: 127-32
8. Khajavi K, Shen A, Lagina M, Hutchison A. Comparison of clinical outcomes following minimally invasive lateral interbody fusion stratified by preoperative diagnosis. Eur Spine J. 2015. 24: S322-30
9. Lykissas MG, Aichmair A, Sama AA, Hughes AP, Lebl DR, Cammisa FP. Nerve injury and recovery after lateral lumbar interbody fusion with and without bone morphogenetic protein-2 augmentation: A cohort-controlled study. Spine J. 2014. 14: 217-24
10. Papanastassiou ID, Eleraky M, Vrionis FD. Contralateral femoral nerve compression: An unrecognized complication after extreme lateral interbody fusion (XLIF). J Clin Neurosci. 2011. 18: 149-51
11. Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: Clinical and radiographic outcomes at 1 year: A preliminary report. J Spinal Disord Tech. 2011. 24: 242-50
12. Tormenti MJ, Maserati MB, Bonfield CM, Okonkwo DO, Kanter AS. Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus. 2010. 28: E7-