- Department of Neurosurgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India
- Department of Pathology, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India
- Department of Pathology and Laboratory Medicine, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
Correspondence Address:
Nishant Goyal, Department of Neurosurgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
DOI:10.25259/SNI_201_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kunal Singla1, Nishant Goyal1, Pulkit Mittal1, Zahed Ali Qamer2, Jitender Chaturvedi1, Arvind Kumar3. Hump on head: Rare case of bi-frontal fibrous dysplasia. 05-Jan-2024;15:1
How to cite this URL: Kunal Singla1, Nishant Goyal1, Pulkit Mittal1, Zahed Ali Qamer2, Jitender Chaturvedi1, Arvind Kumar3. Hump on head: Rare case of bi-frontal fibrous dysplasia. 05-Jan-2024;15:1. Available from: https://surgicalneurologyint.com/surgicalint-articles/12699/
Abstract
Background: FD is relatively rare in the craniofacial region, accounting for only 20% of all cases. Currently, two general subtypes of FD are recognized: monostotic and polyostotic. The monostotic form is more frequent, accounting for 75% to 80% of fibrous dysplasia cases.
Case Description: An 18-year-old male presented with the complaint of bony-hard swelling over the forehead for 8 years. Radiology showed an expansile osseous lesion involving frontal bones. The patient underwent bi-frontal craniectomy with gross total resection of tumour mass with titanium mesh cranioplasty. His postoperative period was uneventful and was discharged on the seventh postoperative day.
Conclusion: The cases of monostotic skull fibrous dysplasia should be treated by resection of the affected bone and cranioplasty. However, a more conservative re-contouring may be carried out in cases with multifocal involvement or when the excision is considered risky due to proximity to the major venous sinuses.
Keywords: Fibrous dysplasia, Frontal, Hump on the head, Parietal
INTRODUCTION
Fibrous dysplasia (FD) is a benign, congenital, and noncommunicable disease affecting both genders equally. A benign proliferation of fibrous tissue in the bone marrow characterizes it. FD is relatively rare in the craniofacial region, and incidence has been estimated at 1 in 5,000–10,000.[
The authors wish to report a rare case of monostotic FD, as it involves the bifrontal bone, overlying the superior sagittal sinus. We used the “cut, remove, and replace” method of dealing with FD and would like to discuss the management options of this rare entity.
CASE DESCRIPTION
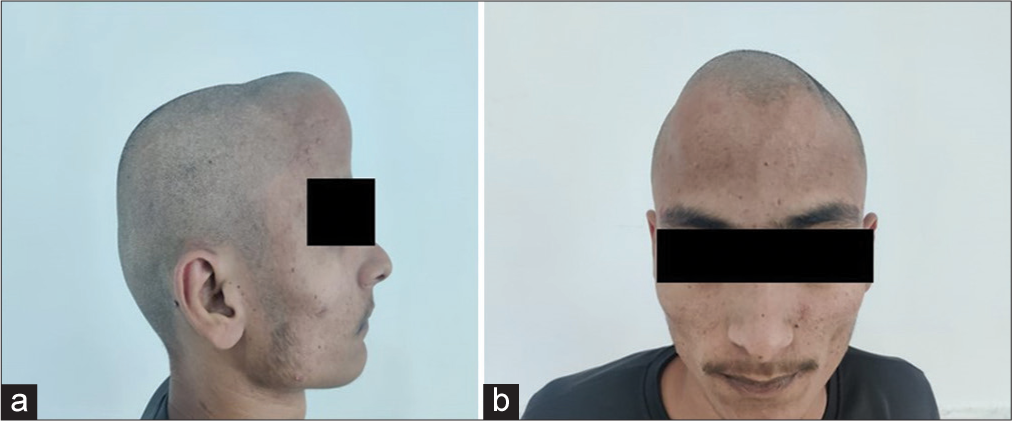
An 18-year-old male presented with the complaint of a bony, hard swelling over the forehead for eight years. As per the patient’s description, the swelling was “initially the size of a pea,” but it gradually increased to “the size of a tennis ball.” There was no history of rupture or discharge from it. This was associated with mild headaches without any aggravating or relieving factors. There was no history of seizure, vomiting, trauma, or blurring of vision. On examination, a bony, hard, nonpulsatile, immobile, non-tender swelling, 8 × 10 × 15 cm in size, was present over the midline, bifrontal region [
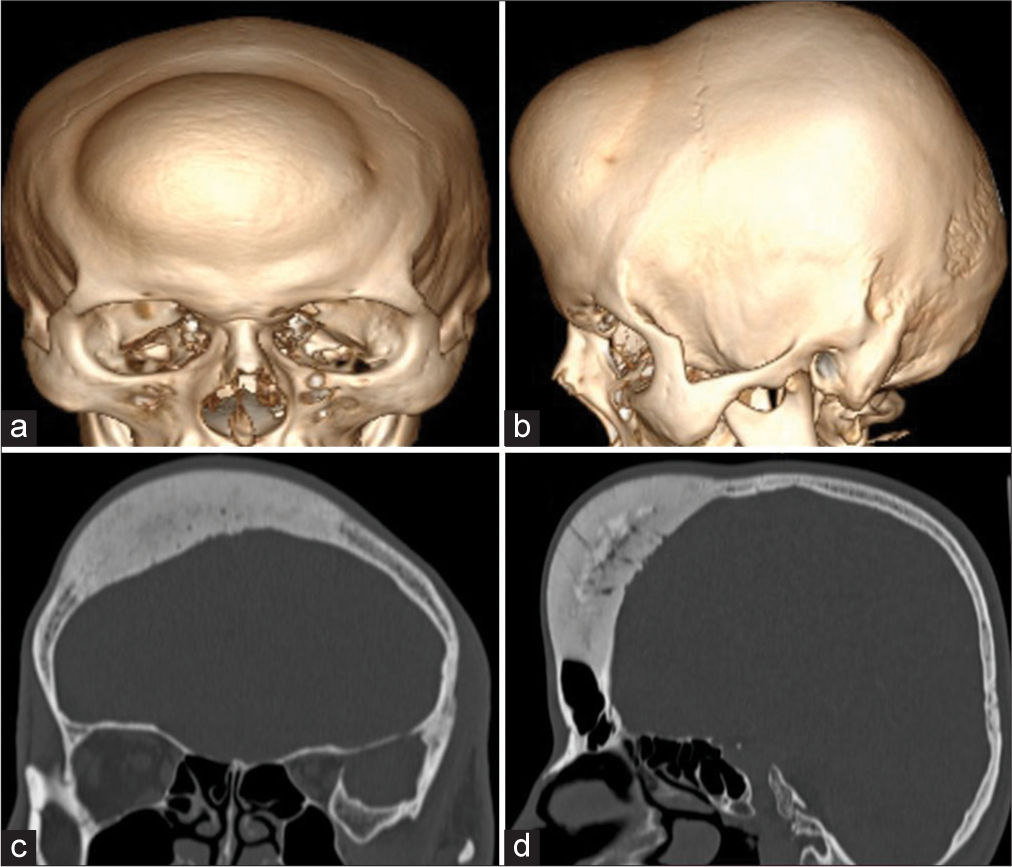
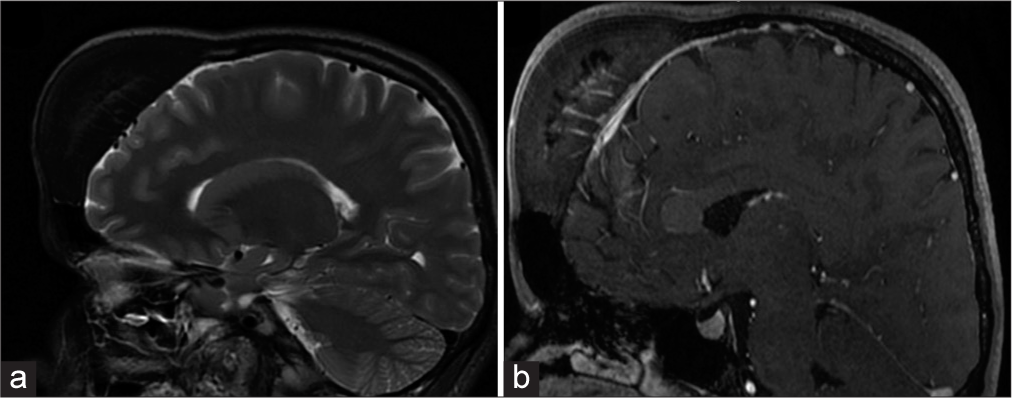
Computed tomography (CT) of the head showed an expansile osseous lesion involving the bifrontal bones with linear trabecular striations [
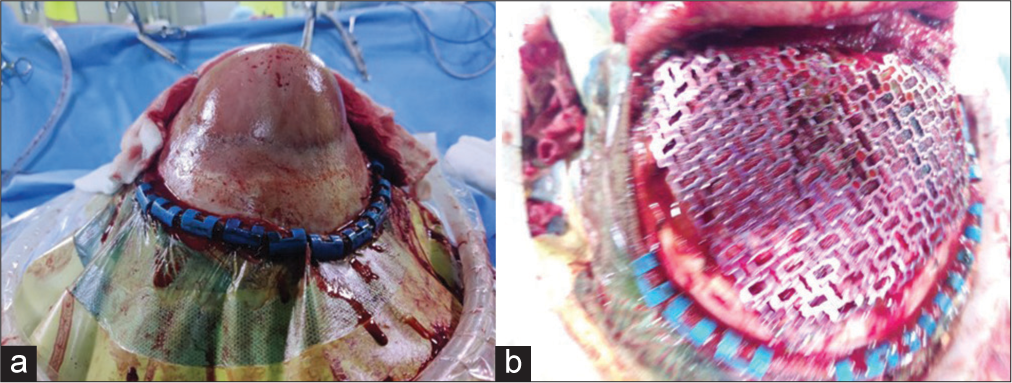
The tumor was resected by bifrontal craniotomy [
The postoperative period was uneventful, and the patient was discharged on the 7th postoperative day. Histopathology revealed a fibro-osseous lesion with irregular curvilinear woven bone without conspicuous osteoblastic rimming, intervening fibrous tissue composed of bland fibroblastic spindle cells [
DISCUSSION
FD is characterized by fibro-osseous lesions with blending of fibrous and osseous tissue, with resultant secondary bony metaplasia, without osteoblast maturation producing immature, newly formed, and weakly calcified bone.[
CT best characterizes FD. Its appearance pattern on CT may vary because of variable combinations of osseous as well as fibrous elements. It may be ground glass or mixed (56%), homogeneous radiopaque (sclerotic) (23%), and radiolucent with a lytic pattern of trabeculae (cystic) (21%).[
The aim of the treatment is correction of the facial deformity, prevention of pathological fracture, control of pain, and prevention of recurrence.[
CONCLUSION
To conclude, cases of monostotic skull FD should be treated by resection of the affected bone and cranioplasty. As we have shown, even a case involving the bifrontal bones and lying over the superior sagittal sinus can be resected completely, followed by reconstruction. However, a more conservative recontouring may be carried out in cases with multifocal involvement or when the excision is considered risky due to proximity to the major venous sinuses.
Ethical approval
Not applicable.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chandavarkar V, Patil PM, Bhargava D, Mishra MN. A rare case report of craniofacial fibrous dysplasia. J Oral Maxillofac Pathol. 2018. 22: 406-9
2. Gupta D, Garg P, Mittal A. Computed tomography in craniofacial fibrous dysplasia: A case series with review of literature and classification update. Open Dent J. 2017. 11: 384-403
3. Javaid MK, Boyce A, Appelman-Dijkstra N, Ong J, Defabianis P, Offiah A. Best practice management guidelines for fibrous dysplasia/McCune-Albright syndrome: A consensus statement from the FD/MAS international consortium. Orphanet J Rare Dis. 2019. 14: 139
4. Maher CO, Friedman JA, Meyer FB, Lynch JJ, Unni K, Raffel C. Surgical treatment of fibrous dysplasia of the skull in children. Pediatr Neurosurg. 2002. 37: 87-92
5. Menon S, Venkatswamy S, Ramu V, Banu K, Ehtaih S, Kashyap VM. Craniofacial fibrous dysplasia: Surgery and literature review. Ann Maxillofac Surg. 2013. 3: 66-71
6. Ozek C, Gundogan H, Bilkay U, Tokat C, Gurler T, Songur E. Craniomaxillofacial fibrous dysplasia. J Craniofac Surg. 2002. 13: 382-9
7. Xu J, Li X, Lv CS, Chen Y, Wang M, Liu JF. Treatment protocols for growth hormonesecreting pituitary adenomas combined with craniofacial fibrous dysplasia: A case report of atypical McCuneAlbright syndrome. Exp Ther Med. 2014. 8: 877-80