- Department of Neurosurgery, Japan Organization of Occupational Health and Safety, Toyama Rosai Hospital, Toyama, Japan.
DOI:10.25259/SNI_306_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yu Shimizu, Kazuhiko Tokuda, Park Cheho. Hyperperfusion and intracranial hemorrhage after burr hole surgery of chronic subdural hematoma. 30-Mar-2021;12:124
How to cite this URL: Yu Shimizu, Kazuhiko Tokuda, Park Cheho. Hyperperfusion and intracranial hemorrhage after burr hole surgery of chronic subdural hematoma. 30-Mar-2021;12:124. Available from: https://surgicalneurologyint.com/surgicalint-articles/10687/
Abstract
Background: Chronic subdural hematomas (CSDHs) mainly occur in elderly people and usually develop after minor head injuries. CSDH can be cured by a relatively simple burr hole surgery. Rarely reported, hemorrhagic postsurgical complications include subarachnoid, intracerebral, intraventricular, and remote cerebellar hemorrhages. The causes of such uncommon complications are difficult to explain and remain poorly understood.
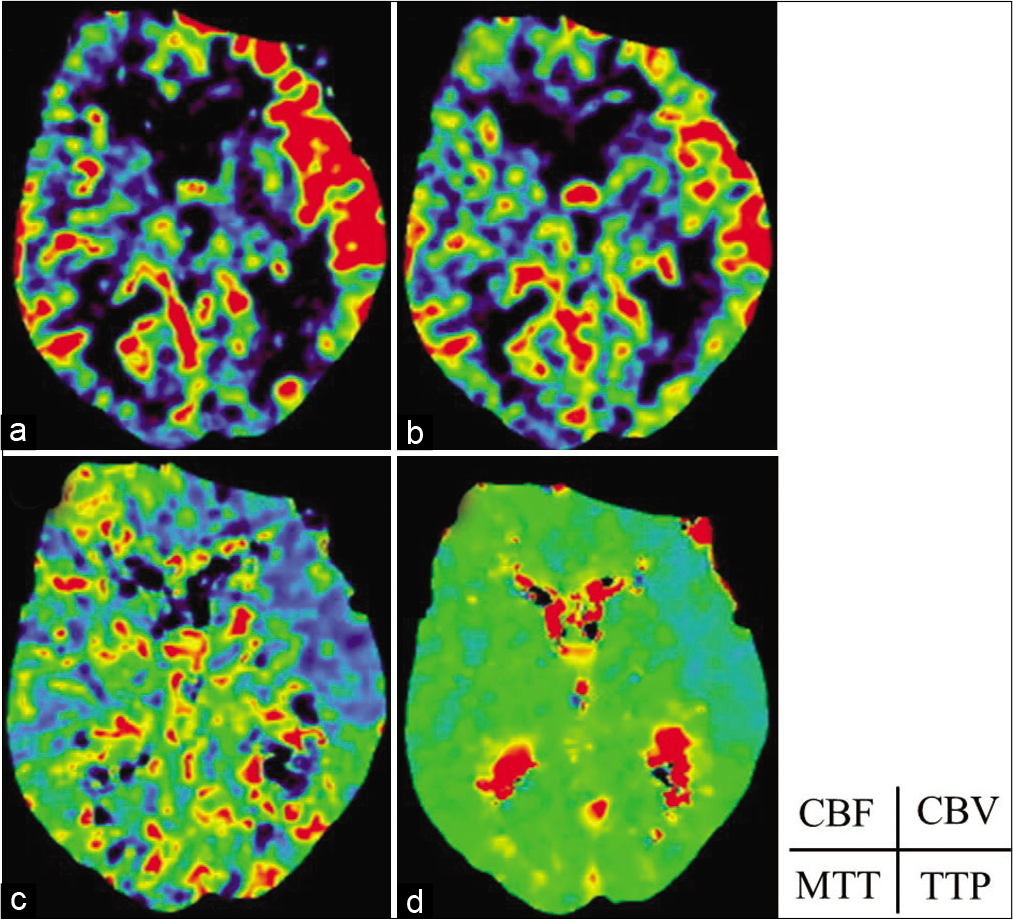
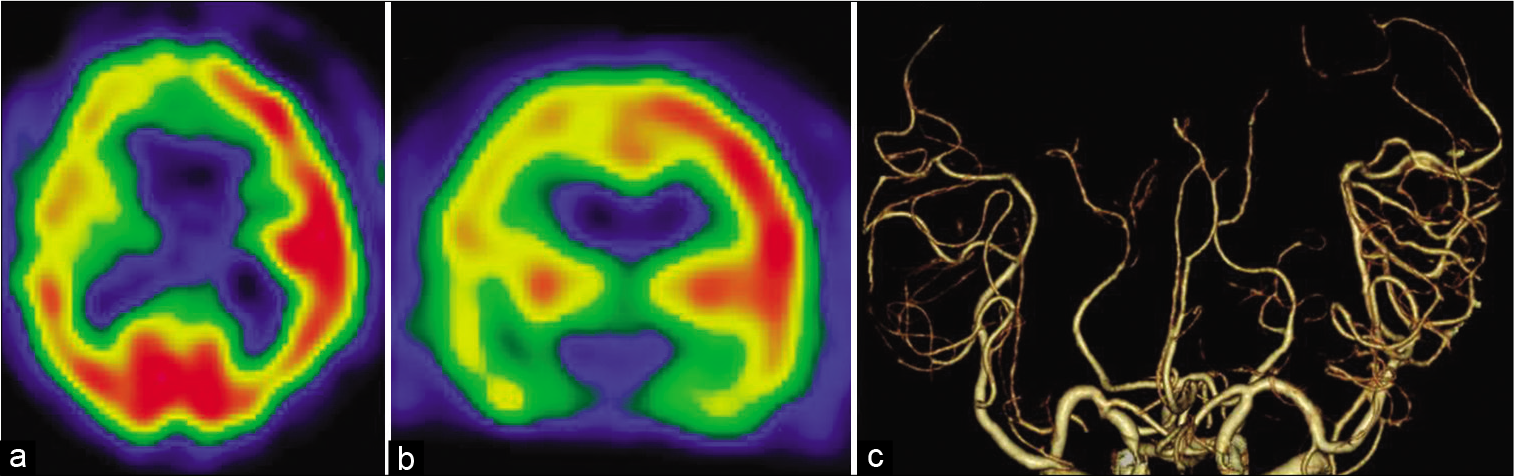
Case Description: We report the case study of an 89-year-old man with CSDH who presented with the right hemiparesis. He underwent burr hole surgery with a closed-drainage system. A computed tomography (CT) scan conducted the following day demonstrated an acute intraventricular hemorrhage and hyperperfusion of the ipsilateral hemisphere.
Conclusion: This is a rare case of an acute hematoma in the ventricle following drainage of a CSDH. The likely mechanism of this intraventricular hemorrhage could be that the drainage of the hematoma produced a movement of the ventricle and hemisphere accompanied by hyperperfusion.
Keywords: Burr hole surgery, Chronic subdural hematoma, Computed tomography perfusion, Hyperperfusion, Intraventricular hemorrhage, Single-photon emission computed tomography, Vascular dilation
BACKGROUND
Chronic subdural hematoma (CSDH) is a neurological disease that frequently affects the elderly, with a mortality rate of 0.5–4%. Known risk factors include mild head injury, advanced age, alcohol abuse, coagulopathies, and therapeutic anticoagulation.
CASE PRESENTATION
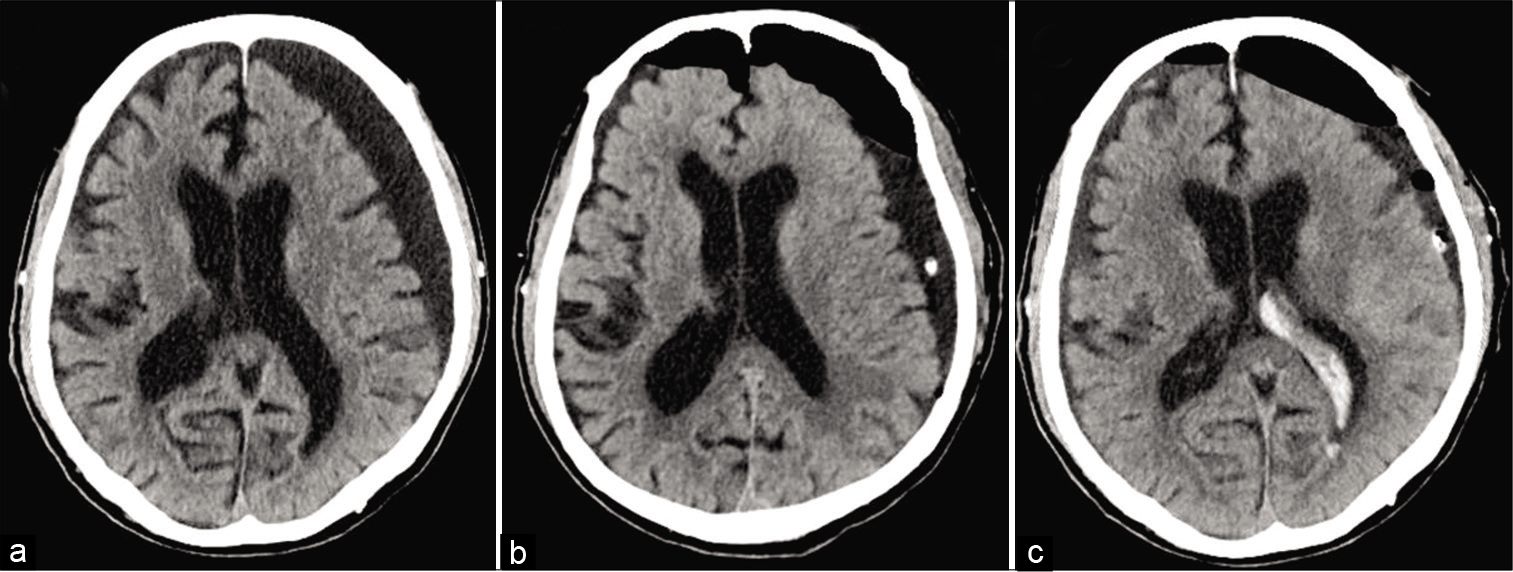
An 89-year-old man was admitted to our division with the right hemiparesis and decreased cognitive ability. Two weeks before admission, he experienced mild head trauma without neurologic deficit. Computed tomography showed a subdural hematoma compressing the left cerebral hemisphere [
Preoperative coagulation parameters were normal. The patient underwent an operation, in which catheters were inserted through the burr holes made in both sides of the parietal area under local anesthesia. The subdural space was washed with warm 0.9% saline until its return was clear. The patient’s vital signs remained stable during the evacuation, and the blood pressure did not increase during the surgery. At the end of the procedure, a subdural frontal closed drainage system was placed. The drainage rate was controlled by gravity and the system was on removed on the second postoperative day. Consciousness and right hemiparesis improved after surgery.
The postoperative CT scan showed bilateral frontal pneumocephalus. No acute bleeding or increase in the left hemispheric hematoma was detected [
DISCUSSION
Intracranial hemorrhage after burr hole surgery has an incidence of approximately 0.08–0.6%.
On the other hand, it has been previously reported that remote hemorrhage could be the result of intraoperative and postoperative loss of CSF.
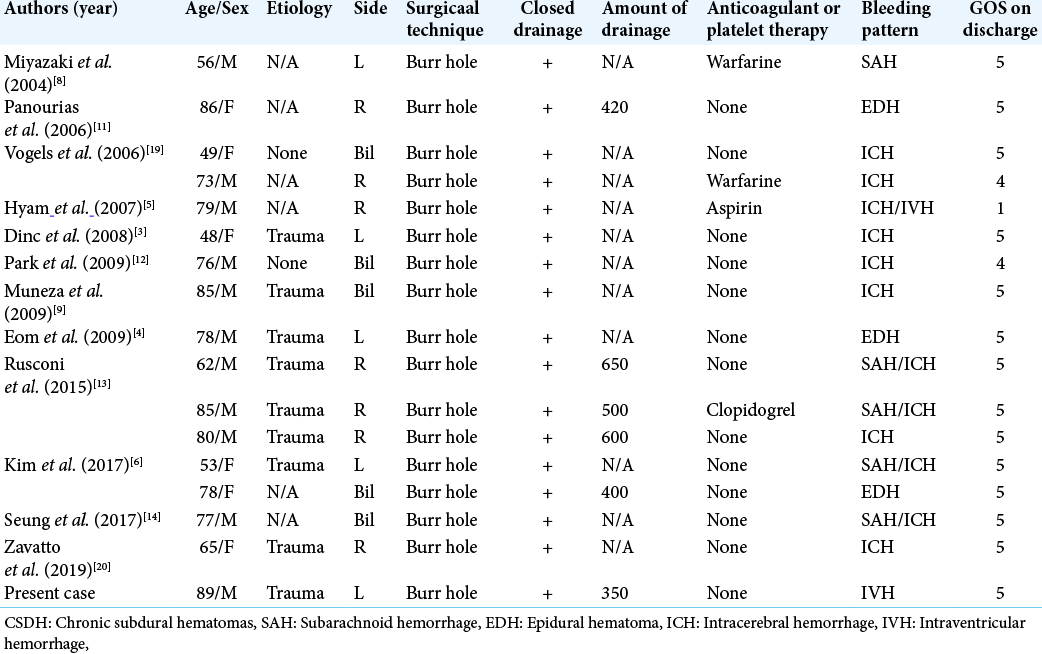
Sixteen other case studies were retrieved from the literature, amounting to 17 reports, including ours. The clinical and radiological summaries of all the patients are shown in [
CONCLUSION
Despite being a rare complication, it is essential to be aware of the development of hyperperfusion and intracranial hematoma after surgery. Sudden decompression should be avoid in the treatment of CSDH and the treatment carefully tailored to the patient’s individual condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Editage (www.editage.com) for the English language editing.
References
1. Brockmann MA, Groden C. Remote cerebellar hemorrhage: A review. Cerebellum. 2006. 5: 64-8
2. Cohen-Gadol AA. Remote contralateral intraparenchymal hemorrhage after overdrainage of a chronic subdural hematoma. Int J Surg Case Rep. 2013. 4: 834-6
3. Dinc C, Iplikcioglu AC, Bikmaz K, Navruz Y. Intracerebral haemorrhage occurring at remote site following evacuation of chronic subdural haematoma. Acta Neurochir (Wien). 2008. 150: 497-9
4. Eom KS, Kim TY, Park JT. Contralateral acute interdural haematoma occurring after burr hole drainage of chronic subdural haematoma. Br J Neurosurg. 2009. 23: 213-5
5. Hyam JA, Turner J, Peterson D. Cerebellar haemorrhage after repeated burr hole evacuation for chronic subdural haematoma. J Clin Neurosci. 2007. 14: 83-6
6. Kim DH, Kim HS, Choi HJ, Han IH, Cho WH, Nam KH. Remote hemorrhage after burr hole drainage of chronic subdural hematoma. Korean J Neurotrauma. 2017. 13: 144-8
7. Kotwica Z, Brzeziński J. Chronic subdural haematoma treated by burr holes and closed system drainage: Personal experience in 131 patients. Br J Neurosurg. 1991. 5: 461-5
8. Miyazaki T, Matsumoto Y, Ohta F, Daisu M, Moritake K. A case of unknown origin subarachnoid hemorrhage immediately following drainage for chronic subdural hematoma. Kurume Med J. 2004. 51: 163-7
9. Muneza S, Rasoloherimampiononiaina MR, Nduwamariya MJ. Postoperative intracerebral and intraventricular hemorrhages following removal of a chronic subdural hematoma. J Clin Neurosci. 2009. 16: 1346-8
10. Ogasawara K, Ogawa A, Okuguchi T, Kobayashi M, Suzuki M, Yoshimoto T. Postoperative hyperperfusion syndrome in elderly patients with chronic subdural hematoma. Surg Neurol. 2000. 54: 155-9
11. Panourias IG, Skandalakis PN. Contralateral acute epidural haematoma following evacuation of a chronic subdural haematoma with burr-hole craniostomy and continuous closed system drainage: A rare complication. Clin Neurol Neurosurg. 2006. 108: 396-9
12. Park KJ, Kang SH, Lee HK, Chung YG. Brain stem hemorrhage following burr hole drainage for chronic subdural hematoma-case report. Neurol Med Chir (Tokyo). 2009. 49: 594-7
13. Rusconi A, Sangiorgi S, Bifone L, Balbi S. Infrequent hemorrhagic complications following surgical drainage of chronic subdural hematomas. J Korean Neurosurg Soc. 2015. 57: 379-85
14. Seung WB, Jeong JH. Postoperative subarachnoid hemorrhage and multi-punctate intracerebral hemorrhages following evacuation of bilateral chronic subdural hematomas. Korean J Neurotrauma. 2017. 13: 149-52
15. Shrestha R, You C. Spontaneous chronic subdural hematoma associated with arachnoid cyst in children and young adults. Asian J Neurosurg. 2014. 9: 168-72
16. Sturiale CL, Rossetto M, Ermani M. Remote cerebellar hemorrhage after supratentorial procedures (Part 1): A systematic review. Neurosurg Rev. 2016. 39: 565-73
17. Toledo E, Eynan N, Shalit M. Intracranial hypotension-an iatrogenic complication of vacuum drainage systems. Acta Neurochir (Wien). 1980. 52: 55-9
18. van Roost D, Thees C, Brenke C, Oppel F, Winkler PA, Schramm J. Pseudohypoxic brain swelling: A newly defined complication after uneventful brain surgery, probably related to suction drainage. Neurosurgery. 2003. 53: 1315-26
19. Vogels RL, Verstegen MJ, van Furth WR. Cerebellar haemorrhage after non-traumatic evacuation of supratentorial chronic subdural haematoma: Report of two cases. Acta Neurochir (Wien). 2006. 148: 993-6
20. Zavatto L, Marrone F, Allevi M. Bilateral oculomotor palsy after surgical evacuation of chronic subdural hematoma. World Neurosurg. 2019. 127: 241-4