- Department of Neuroradiology, Leeds Teaching Hospitals NHS Trust, Leeds,
- Department of Medicine, Pinderfields General Hospital, Wakefield,
- Department of Neurosurgery, Leeds General Infirmary, Leeds, United Kingdom.
Correspondence Address:
Saad Moughal, Department of Neuroradiology, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom.
DOI:10.25259/SNI_963_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saad Moughal1, Sana Ahmad2, Nayyar Saleem1, Chris Derham3. Hypertensive posterior reversible encephalopathy causing obstructive hydrocephalus. 17-Mar-2023;14:94
How to cite this URL: Saad Moughal1, Sana Ahmad2, Nayyar Saleem1, Chris Derham3. Hypertensive posterior reversible encephalopathy causing obstructive hydrocephalus. 17-Mar-2023;14:94. Available from: https://surgicalneurologyint.com/surgicalint-articles/12193/
Abstract
Background: Posterior reversible encephalopathy syndrome (PRES) can occur due to the detrimental effect of malignant hypertension on cerebral autoregulation. Most reported cases describe involvement of the supratentorial areas. Involvement of the posterior fossa structures in conjunction with supratentorial involvement has also been reported; however, PRES affecting the infratentorial structures without supratentorial involvement is a rare phenomenon. Clinical manifestations can involve severe headache, seizures, and reduced consciousness with treatment focused primarily on blood pressure control.
Case Description: We report a case of PRES with isolated involvement of the infratentorial structures leading to obstructive hydrocephalus. The patient was managed with aggressive control of blood pressure and avoided ventriculostomy or posterior fossa decompression with a good outcome.
Conclusion: Medical management in the absence of neurological deficit can be associated with a good outcome.
Keywords: Cerebral autoregulation, Hypertensive encephalopathy, Obstructive hydrocephalus, Posterior fossa oedema
INTRODUCTION
Posterior reversible encephalopathy syndrome (PRES) or hypertensive encephalopathy is an entity associated with hypertensive crisis and typically presents with acute headache, seizures, or disorders of consciousness.[
We present a case of posterior fossa PRES due to hypertensive crisis that presented with acute obstructive hydrocephalus and discuss pertinent clinical and radiological features.
Literature search
A search of PubMed and Medline databases was reviewed for articles from inception to April 2022 inclusive. Limits were placed on those articles published in the English language. We excluded editorials, commentaries, letters, conference papers, and reviews. Our search only identified case reports; therefore, we did not perform a systematic review.
CASE REPORT
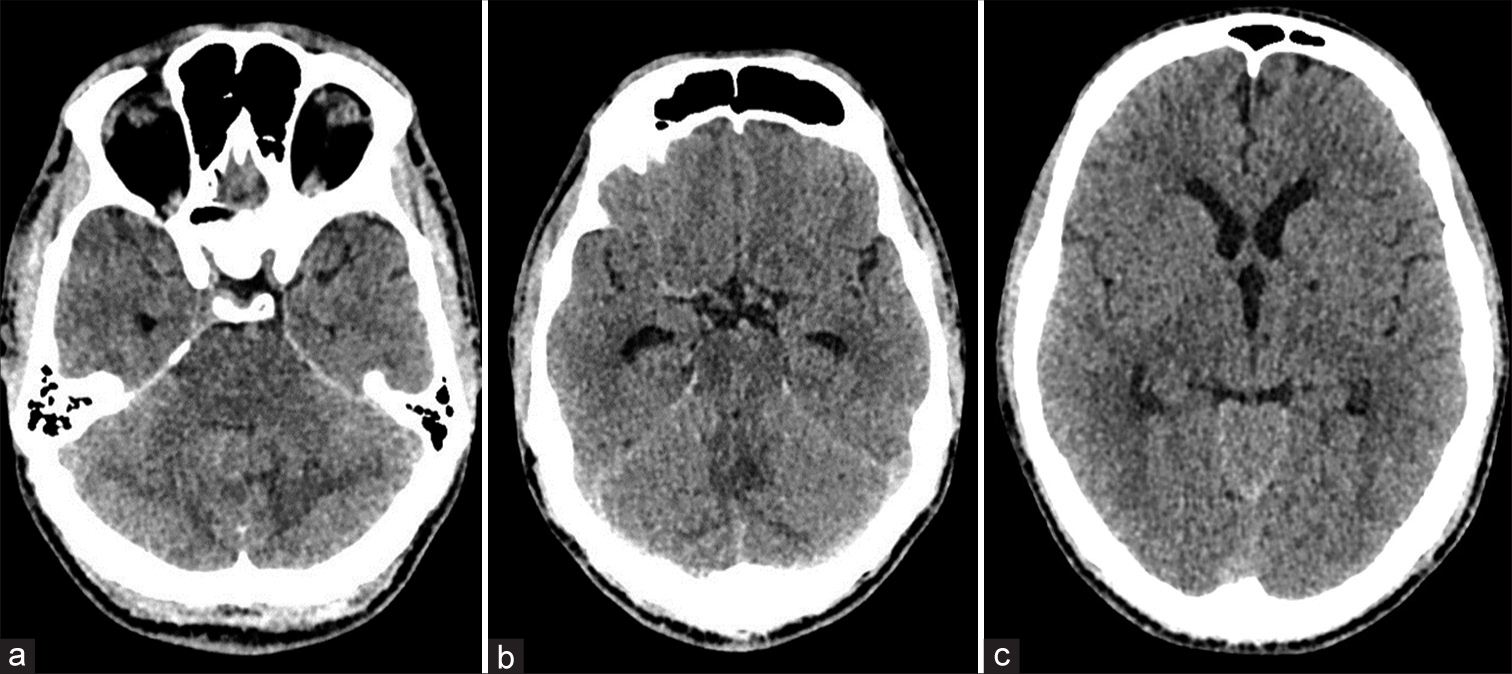
A 39-year-old male, Caucasian, smoker who was usually fit and well presented with a 4-month history of progressive headache and new onset vomiting leading to attendance at the emergency department. Headaches were suggestive of raised intracranial pressure, worse on lying flat and bending forward. The patient reported blurriness of his vision when the headaches were severe, but there were no lower cranial nerve signs. Blood pressure on arrival was 241/151 mmHg. Fundoscopy demonstrated Grade III papilledema in the right eye. The rest of the neurological examination was normal. An urgent computed tomography head scan demonstrated mild hydrocephalus and possible diffuse cerebellar edema, but no mass lesion or hemorrhage [
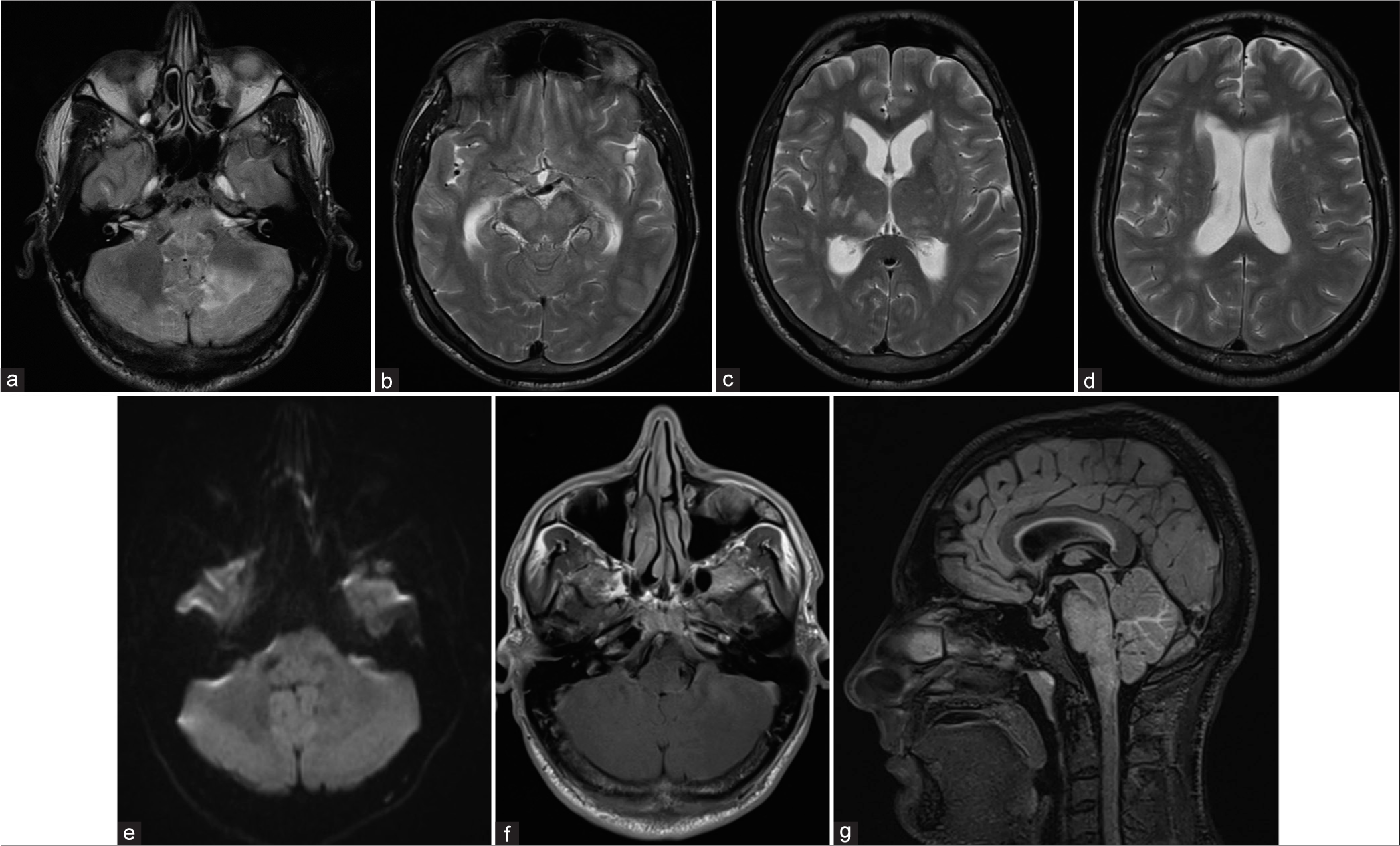
Figure 2:
Initial magnetic resonance imaging showing T2/fluid attenuated inversion recovery hyperintensities in the cerebellum and brainstem (a, b, and g) and dilated lateral ventricles with periventricular hyperintensity (c and d). No infarction on diffusion-weighted imaging (e) or enhancing lesion on contrast-enhanced T1 imaging (f).
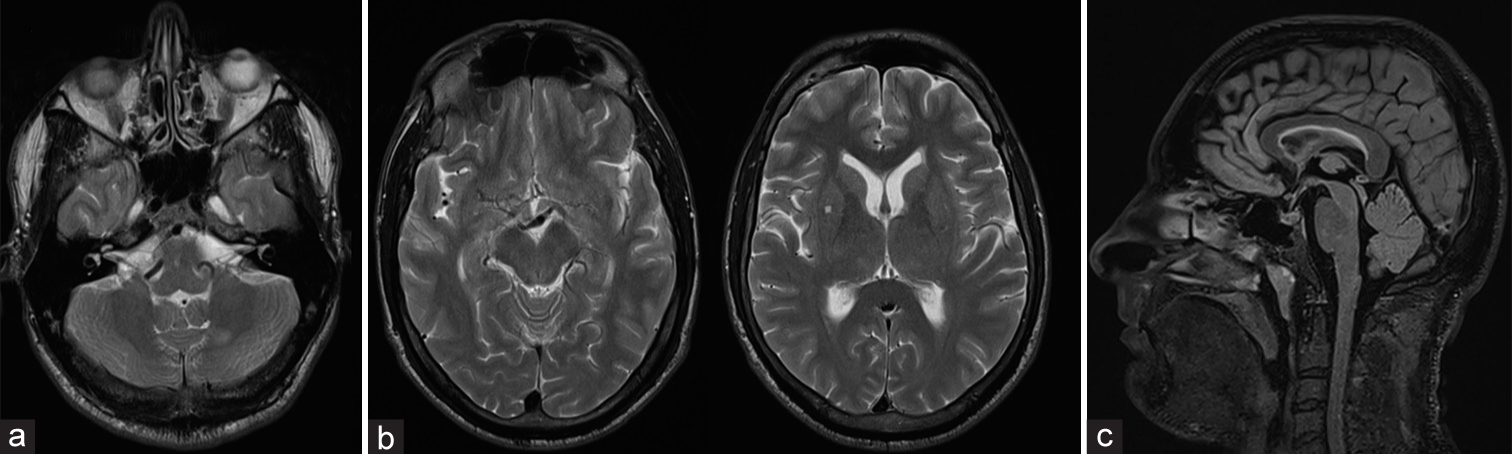
Figure 3:
Magnetic resonance imaging 6 weeks later demonstrating resolution of signal change and swelling of the infratentorial structures and improvement of hydrocephalus (a and c). Occasional T2 hyperintensities in supratentorial white matter persist, presumably due to mild small vessel disease (b).
DISCUSSION
Posterior fossa PRES presenting with acute hydrocephalus is a rare phenomenon. The pathogenesis of PRES is poorly understood but may involve cerebrovascular endothelial dysfunction resulting in impaired autoregulation, vasodilation, and disruption of the blood-brain barrier leading to vasogenic edema.[
Hypertensive encephalopathy can affect both supra- and infratentorial structures. Cerebellar edema resulting from PRES is a known entity, but this is often associated with concomitant supratentorial edema.[
An important distinguishing feature of posterior fossa PRES may be the clinical-radiological dissociation that we observed, which corroborates with findings elsewhere.[
CONCLUSION
This report highlights that hypertensive encephalopathy of the posterior fossa can present with obstructive hydrocephalus which may resolve with aggressive control of blood pressure. However, close monitoring and a threshold for rapid decompression must remain in the treatment armamentarium. Radiological findings that manifest with this condition warrant awareness as a differential, as prompt recognition and treatment of underlying significant hypertension can be associated with good outcomes. Further larger scale studies are needed to elucidate this clinical syndrome further, particularly with respect to predictive factors for the varying degree of clinical presentations.
Statement of ethics
Patient consent for publication was obtained.
Author contributions
SM: Drafting and reviewing manuscript. SA: Reviewing and editing the manuscript. NS: Reviewing the manuscript. CD: Reviewing the manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abusabha Y, Petridis AK, Kraus B, Kamp MA, Steiger HJ, Beseoglu K. Life-threatening posterior reversible encephalopathy syndrome in the cerebellum treated by posterior fossa decompression. Acta Neurochir (Wien). 2017. 159: 1325-8
2. Chang GY, Keane JR. Hypertensive brainstem encephalopathy: Three cases presenting with severe brainstem edema. Neurology. 1999. 53: 652-4
3. Cruz-Flores S, de Assis Aquino Gondim F, Leira EC. Brainstem involvement in hypertensive encephalopathy: Clinical and radiological findings. Neurology. 2004. 62: 1417-9
4. Fischer M, Schmutzhard E. Posterior reversible encephalopathy syndrome. J Neurol. 2017. 264: 1608-16
5. Grossbach AJ, Abel TJ, Hodis B, Wassef SN, Greenlee JD. Hypertensive posterior reversible encephalopathy syndrome causing posterior fossa edema and hydrocephalus. J Clin Neurosci. 2014. 21: 207-11
6. Kontos HA, Wei EP, Navari RM, Levasseur JE, Rosenblum WI, Patterson JL. Responses of cerebral arteries and arterioles to acute hypotension and hypertension. Am J Physiol. 1978. 234: H371-83
7. Kumar A, Keyrouz SG, Willie JT, Dhar R. Reversible obstructive hydrocephalus from hypertensive encephalopathy. Neurocrit Care. 2012. 16: 433-9
8. Lee VH, Wijdicks EF, Manno EM, Rabinstein AA. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Arch Neurol. 2008. 65: 205-10
9. Li D, Lian L, Zhu S. Isolated cerebellar involvement in posterior reversible encephalopathy syndrome. J Neurol Sci. 2015. 357: 101-5
10. McKinney AM, Sarikaya B, Gustafson C, Truwit CL. Detection of microhemorrhage in posterior reversible encephalopathy syndrome using susceptibility-weighted imaging. Am J Neuroradiol. 2012. 33: 896-903
11. Nakano H, Tomita Y, Bandoh K, Miyaoka M. Malignant hypertension associated with obstructive hydrocephalus--case report. Neurol Med Chir (Tokyo). 1997. 37: 265-9
12. Sheth RD, Riggs JE, Bodenstenier JB, Gutierrez AR, Ketonen LM, Ortiz OA. Parietal occipital edema in hypertensive encephalopathy: A pathogenic mechanism. Eur Neurol. 1996. 36: 25-8
13. Verrees M, Filho JA, Suarez JI, Ratcheson RA. Primary hypertension-induced cerebellar encephalopathy causing obstructive hydrocephalus. Case report. J Neurosurg. 2003. 98: 1307-11
14. Weingarten K, Barbut D, Filippi CG, Zimmerman RD. Acute hypertensive encephalopathy: Findings on spin-echo and gradient-echo MR imaging. AJR Am J Roentgenol. 1994. 162: 665-70