- Department of Neurosurgery, Fundación Jiménez Díaz University Hospital, Madrid, Spain.
- Department of Pathology, Rey Juan Carlos University Hospital, Madrid, Spain.
Correspondence Address:
Jorge Cabrera-Montes, Department of Neurosurgery, Fundación Jiménez Díaz University Hospital, Madrid, Spain.
DOI:10.25259/SNI_870_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jorge Cabrera-Montes1, Daniela Fuel-Gómez2, Monica Lara-Almunia1. Ileal signet-ring cell carcinoma with brain metastases: A case report. 06-Jan-2023;14:6
How to cite this URL: Jorge Cabrera-Montes1, Daniela Fuel-Gómez2, Monica Lara-Almunia1. Ileal signet-ring cell carcinoma with brain metastases: A case report. 06-Jan-2023;14:6. Available from: https://surgicalneurologyint.com/surgicalint-articles/12093/
Abstract
Background: Signet-ring cell carcinoma (SRCC) is a rare subtype of adenocarcinoma that frequently originates in the stomach. Uncommonly, this tumor can lead to brain metastases; an event rarely reported in the literature.
Case Description: A 76-year-old man with a history of cognitive impairment was diagnosed with two brain space-occupying lesions. A whole-body 18F-FDG PET/computed tomography scan revealed a hypermetabolic lesion in a segment of the ileum corresponding to mural thickening and an ulcerated lesion detected on colonoscopy. A brain biopsy, using an immunohistochemistry protocol, showed signet-ring cells with a pattern that suggested an intestinal origin. The diagnosis of SRCC brain metastases with an ileal origin was made, and a treatment protocol was designed. However, the patient rapidly deteriorated, and passed away shortly afterward.
Conclusion: To the best of our knowledge, this is the first case report of an ileal SRCC with brain metastases.
Keywords: Adenocarcinoma, Brain metastases, Ileum, Signet-ring cell, Small bowel
INTRODUCTION
Signet-ring cell carcinoma (SRCC) is an aggressive and rare type of adenocarcinoma, most frequently found in the stomach.[
Metastatic sites commonly reported in the literature are the liver, lungs, bones, and lymphatics.[
The aim of this article is to present the rare case of a patient with brain metastases in the setting of a primary SRCC of the ileum, as well as to assess, by a search for similar cases in the literature, the particularity of such an occurrence.
CASE DESCRIPTION
Herein, we present the case of a 76-year-old man with no clinical history other than well-controlled arterial hypertension, who came to the emergency department accompanied by his daughter, after a 20-day period of progressive cognitive impairment, characterized by forgetfulness, and decreased attentional capacity. Initial physical and neurological examination was notable for confusion, as the patient was not oriented to time nor space. No other clinical signs were detected.
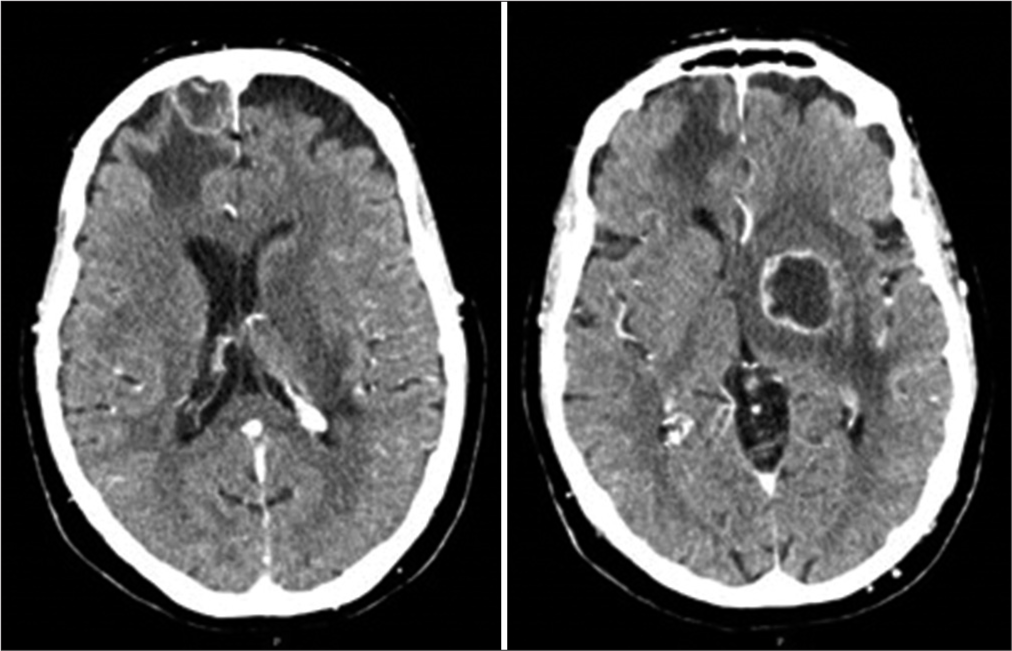
A computed tomography (CT) brain scan [
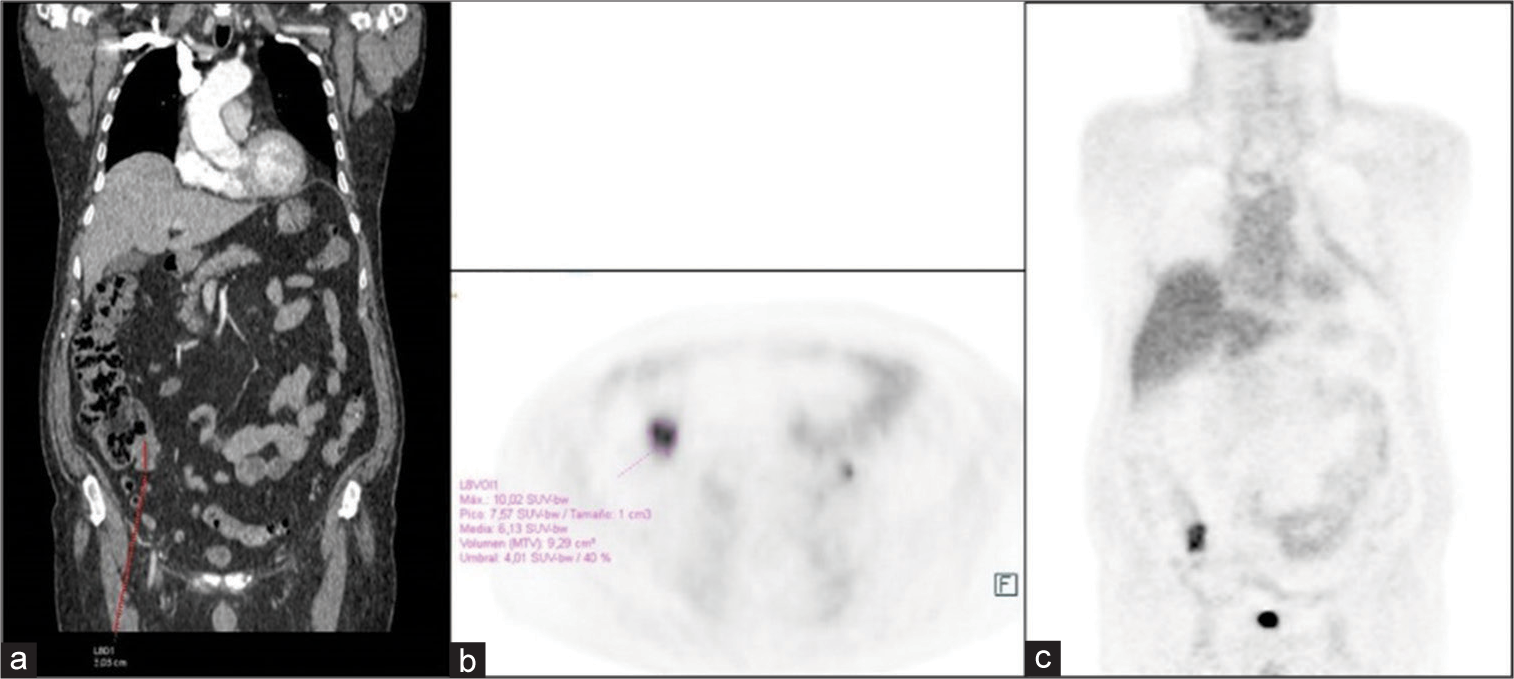
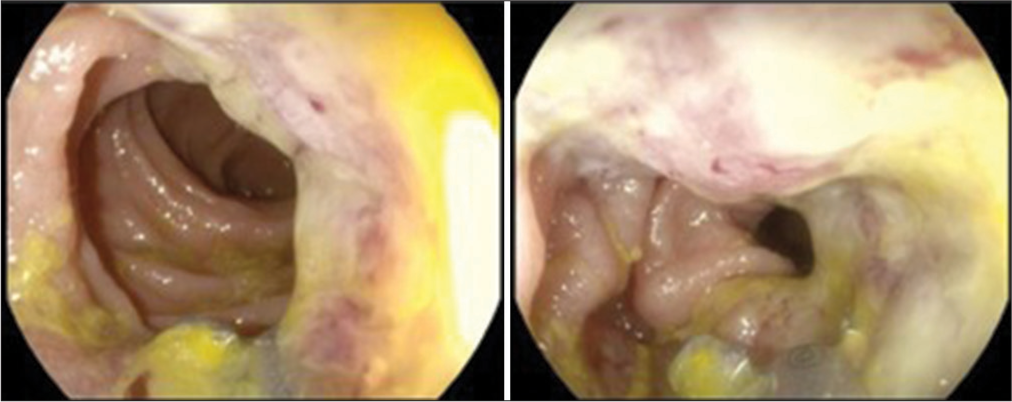
The patient was subsequently admitted and administered IV corticosteroids (Dexamethasone 4 mg/8 h) for symptomatic treatment. As he had no known medical or family history of an oncologic disease, the detection of a possible primary tumor, once the patient was stabilized, became the priority. A whole-body CT and a 18F-FDG PET/CT scan were performed [
A brain biopsy was proposed and accepted by the patient and family, and planned for the next few days, after informed consent was signed. However, the patient began presenting with gait instability and a significant neurological decline, with progressive loss of strength in his right leg; thus, the brain biopsy was prioritized and performed the next day.
Surgical management
An open brain biopsy targeting the right frontal lobe lesion was performed under general anesthesia and a burr-hole was made in the bone overlying the lesion. A cruciate opening of the dura was made, exposing a gray tumor-like infiltrated cortex underneath. Macroscopic pathologic material was obtained in all directions. Adequate hemostasis was assured, and soft-tissue closure was completed without difficulty. There were no intraoperative complications and sufficient tissue was obtained for a pathology and immunohistochemistry (IHC) examination.
Pathological findings
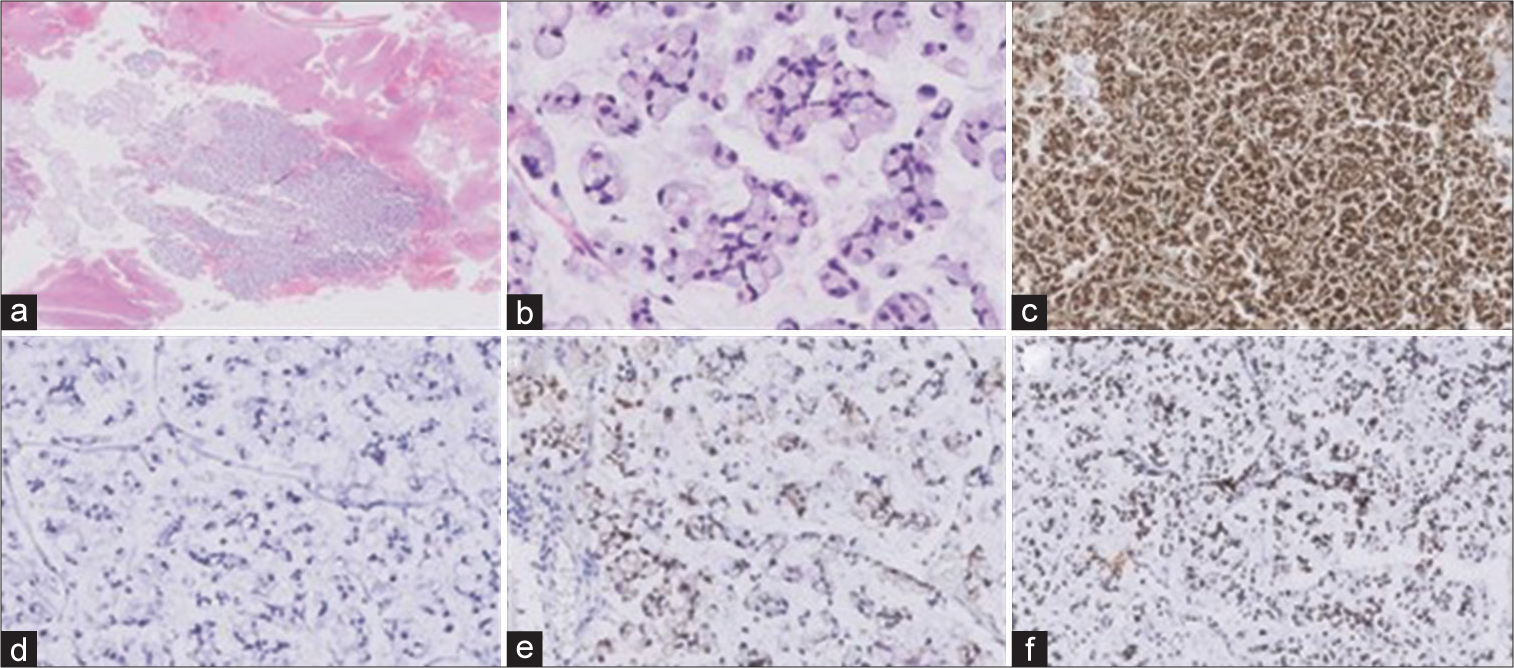
Pathological examination showed the presence of an abundant number of signet-ring cells, with large amounts of mucin displacing the nucleus to the cell periphery, as classically described in the literature.[
The IHC analysis showed a particular pattern (CK7−, CK20+, CEA+, and CDX2+) suggestive of gastrointestinal tract origin [
Given the imaging and pathology findings, a diagnosis of the primary SRCC of the gastrointestinal tract with brain metastases was made, establishing the location of the primary tumor at the distal ileum.
Clinical course and outcome
A therapeutic plan for systemic chemotherapy and holocraneal radiation was proposed and discussed in a multidisciplinary committee. However, the patient’s clinical and neurological status rapidly declined, and he had become aphasic, apathetic, and abulic with impairment in motor function and gait, limiting his ability to eat, bathe, or move independently. After discussion with a second multidisciplinary committee, he was transferred to a medium-stay center for palliative care and symptomatic treatment, where he died shortly thereafter. The total time course from the initial diagnosis of brain metastases to his death was 2 months.
DISCUSSION
SRCC is a rare variant of adenocarcinoma, most frequently found in the stomach,[
Two large series have been published, describing one group of patients with SRCC of the colon,[
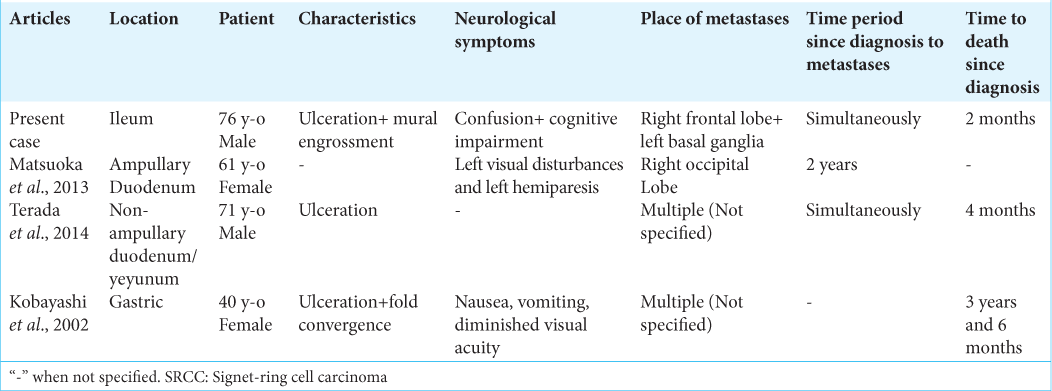
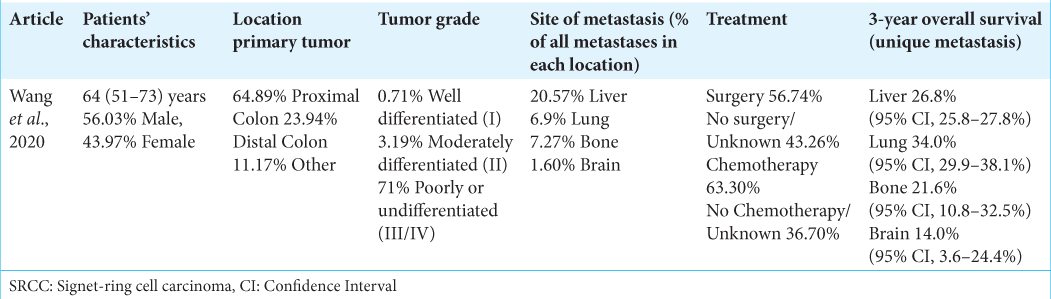
Table 2:
Characteristics of SRCC of the colon extracted from a series in Wang et al., 2020.[
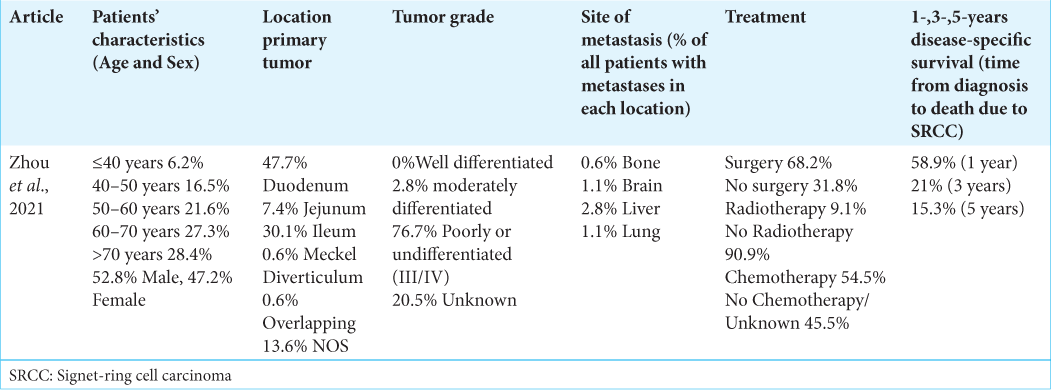
Table 3:
Characteristics of small bowel SRCC, extracted from a series in Zhou et al., 2021.[
As previously mentioned, few cases of brain metastases secondary to SRCC of digestive tract origin have been reported in the literature, with a small percentage of cases of brain metastases documented in series involving SRCC of the colon and small bowel.[
The patient in this reported case initially presented with neurological symptoms as a manifestation of a previously unknown metastatic lesion. Macroscopic analysis of the intestinal tumor in this case (see “Case Description”) revealed characteristics in line with the ones described previously, making this lesion easily misdiagnosed as Chron’s Disease.[
Given the combination of clinical, radiologic, and pathological findings, the diagnosis of brain metastases from a primary ileal SRCC was established.
Limitations
The most notable limitation was an inconclusive intestinal biopsy. However, as has been shown, several reports have found intestinal biopsies to be negative or inconclusive more frequently than in other types of tumors.
Given the rapid decline of the patient’s clinical course, retrieving repeat biopsies of the intestinal lesion and performing additional diagnostic tests were not possible. However, whole-body CT and PET/CT scans only showed pathological findings at the distal ileum.
Necropsy and post-mortem analysis were not performed.
CONCLUSION
SRCC brain metastases arising from the digestive tract, and particularly from ileal segments, are extremely rare. To the best of our knowledge, this report presents the first case of ileal-origin SRCC brain metastases.
Our analysis of different reported cases, published series and available literature, has offered us valuable information to describe this kind of tumor as an aggressive subtype with a poor prognosis. In addition, this tumor is reported to have histological similarities to Crohn’s Disease, allowing for misdiagnosis. Given these findings, in cases where response to adenocarcinoma treatment is inadequate, or in an unclear workup of Crohn’s Disease, suspicion for SRCC should be high. Early diagnosis and early treatment may improve the prognosis of this complex histological variant.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of our institution, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Achneck HE, Pradhan SK, Kavic SM, Longo WE. Primary signet-ring cell carcinoma mimicking segmental Crohn’s colitis. Dig Liver Dis. 2005. 37: 537-41
2. Assi R, Hamieh L, Mukherji D, Haydar A, Temraz S, El-Dika I. Leptomeningeal metastasis as initial manifestation of signet ring colorectal adenocarcinoma: A case report with review of literature. J Gastrointest Oncol. 2015. 6: E89-101
3. Carvalho JR, Tavares J, Goulart I, Santos PM, Vitorino E, Ferreira C. SRCC, ileal crohn disease or both?-A case of diagnostic challenge. GE Port J Gastroenterol. 2018. 25: 47-51
4. Chen JS, Hsieh PS, Chiang JM, Yeh CY, Tsai WS, Tang R. Clinical outcome of SRCC and mucinous adenocarcinoma of the colon. Chang Gung Med J. 2010. 33: 51-7
5. Hammami MB, Aboushaar R, Musmar A, Azhar M. Ileal SRCC masked by Crohn disease. Ochsner J. 2020. 20: 323-5
6. Huang L, Wang L, Shi Y, Zhao Y, Xu C, Zhang J. Brain metastasis from gastric adenocarcinoma: A large comprehensive population-based cohort study on risk factors and prognosis. Front Oncol. 2022. 12: 897681
7. Jarabin JA, Klivényi P, Tiszlavicz L, Molnár FA, Gion K, Földesi I. Late simultaneous carcinomatous meningitis, temporal bone infiltrating macro-metastasis and disseminated multi-organ micro-metastases presenting with mono-symptomatic vertigo-a clinico-pathological case reporT. Ideggyogy Sz. 2020. 73: 354-60
8. Kobayashi M, Araki K, Matsuura K, Kawai S, Moriki T. Early gastric cancer giving rise to bone and brain metastases--a review of the Japanese literature. Hepatogastroenterology. 2002. 49: 1751-4
9. Lee D, Son SY, Kim YB, Han SU, Hur H. Neural invasion is a significant contributor to peritoneal recurrence in signet ring cell gastric carcinoma. Ann Surg Oncol. 2018. 25: 1167-75
10. Lin DM, Park JW, Gattuso P. Metastatic signet-ring cell carcinoma of the bladder in cerebrospinal fluid. Diagn Cytopathol. 2017. 45: 73-6
11. Lui IO, Kung IT, Lee JM, Boey JH. Primary colorectal SRCC in young patients: Report of 3 cases. Pathology. 1985. 17: 31-5
12. Matsuoka G, Wanifuchi H, Suzuki S, Honda K, Okada Y. A brain metastasis from ampullary carcinoma: A case report. No Shinkei Geka. 2013. 41: 143-8
13. Overman MJ, Pozadzides J, Kopetz S, Wen S, Abbruzzese JL, Wolff RA. Immunophenotype and molecular characterisation of adenocarcinoma of the small intestine. Br J Cancer. 2010. 102: 144-50
14. Paparo F, Piccardo A, Clavarezza M, Piccazzo R, Bacigalupo L, Cevasco L. Computed tomography enterography and 18F-FDG PET/CT features of primary SRCC of the small bowel in a patient with Crohn’s disease. Clin Imaging. 2013. 37: 794-7
15. Terada T. SRCC of the nonampullary duodenum and proximal jejunum: A case report with an immunohistochemical study. Endoscopy. 2014. 46: E348
16. Wang J, Li S, Liu Y, Zhang C, Li H, Lai B. Metastatic patterns and survival outcomes in patients with stage IV colon cancer: A population-based analysis. Cancer Med. 2020. 9: 361-73
17. Winter MW, Dokmak A, Marnoy Z, Sinagare S, Levy AN. Metastatic gastric signet ring cell carcinoma mimicking Crohn’s disease. ACG Case Rep J. 2018. 5: e36
18. Zhou YW, Xia RL, Chen YY, Ma XL, Liu JY. Clinical features, treatment, and prognosis of different histological types of primary small bowel adenocarcinoma: A propensity score matching analysis based on the SEER database. Eur J Surg Oncol. 2021. 47: 2108-18