- Department of Neurosurgery, SUNY Upstate Medical University, Syracuse, New York, United States
- St. George’s University, School of Medicine, Great River, New York, United States
- Department of Neurosurgery, University of North Carolina, Chapel Hill, North Carolina, United States.
Correspondence Address:
Disep I. Ojukwu, St. George’s University, School of Medicine, Great River, New York, United States.
DOI:10.25259/SNI_402_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Matthew Protas1, Disep I. Ojukwu2, Dan Y. Draytsel1, Michael A. Galgano1,3. Illustrative resection of mixed intra- and extramedullary thoracic spinal cord capillary hemangioma. 30-Jun-2023;14:226
How to cite this URL: Matthew Protas1, Disep I. Ojukwu2, Dan Y. Draytsel1, Michael A. Galgano1,3. Illustrative resection of mixed intra- and extramedullary thoracic spinal cord capillary hemangioma. 30-Jun-2023;14:226. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12382
Abstract
Background: Capillary hemangiomas are typically superficial benign tumors of the cutaneous and mucosal tissues of the face and neck in pediatric patients. In adults, they typically occur in middle-aged males who present with pain, myelopathy, radiculopathy, paresthesias, and bowel/bladder dysfunction. The optimal treatment for intramedullary spinal cord capillary hemangiomas is gross total/en bloc resection.
Methods: Here, we present a 63-year-old male with increasing right greater than left lower extremity numbness/ weakness, attributed to a T8-9 mixed intra- and extramedullary capillary hemangioma.
Results: One year following complete lesion resection, the patient used an assistive device to ambulate and continued to improve neurologically.
Conclusion: We presented a 63-year-old male whose paraparesis was attributed to a T8-9 mixed intra- and extramedullary capillary hemangioma who did well following total en bloc lesion resection. In addition to this case study/technical note, we provide a 2-D intraoperative video detailing the resection technique.
Keywords: Intradural capillary hemangioma, Mixed intramedullary extramedullary capillary hemangioma, Neurosurgery, Spinal tumor surgical video, Thoracic spinal cord
INTRODUCTION
Capillary hemangiomas are typically superficial benign tumors of the cutaneous and mucosal tissues of the face and neck in pediatric patients.[
Video 1
CASE DESCRIPTION
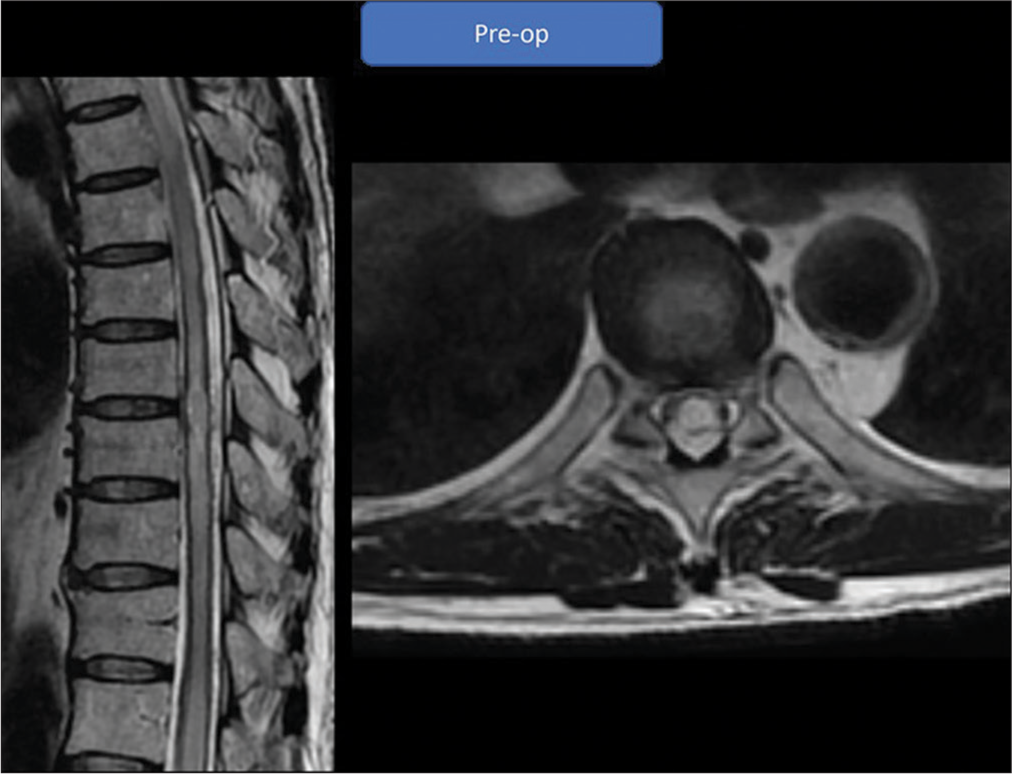
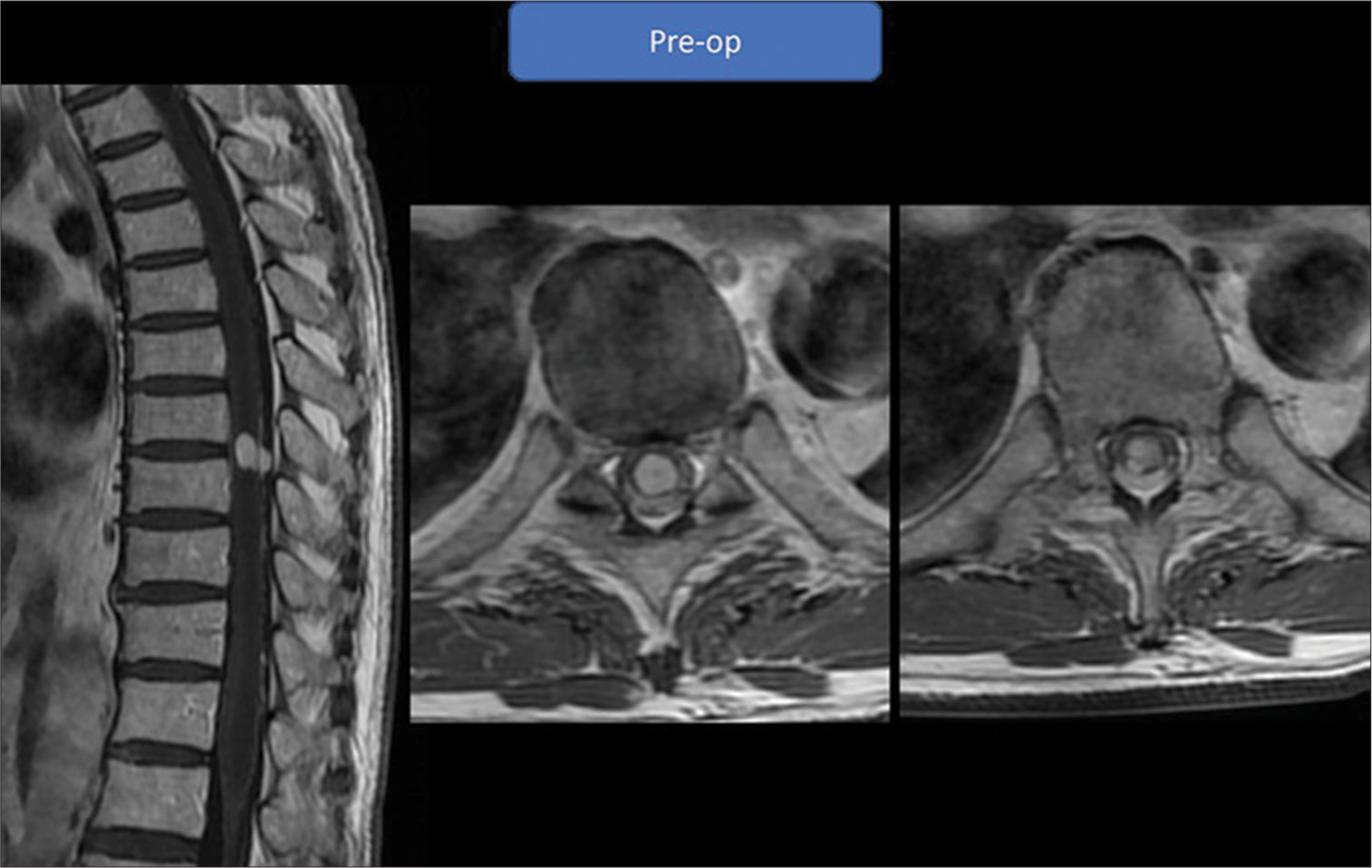
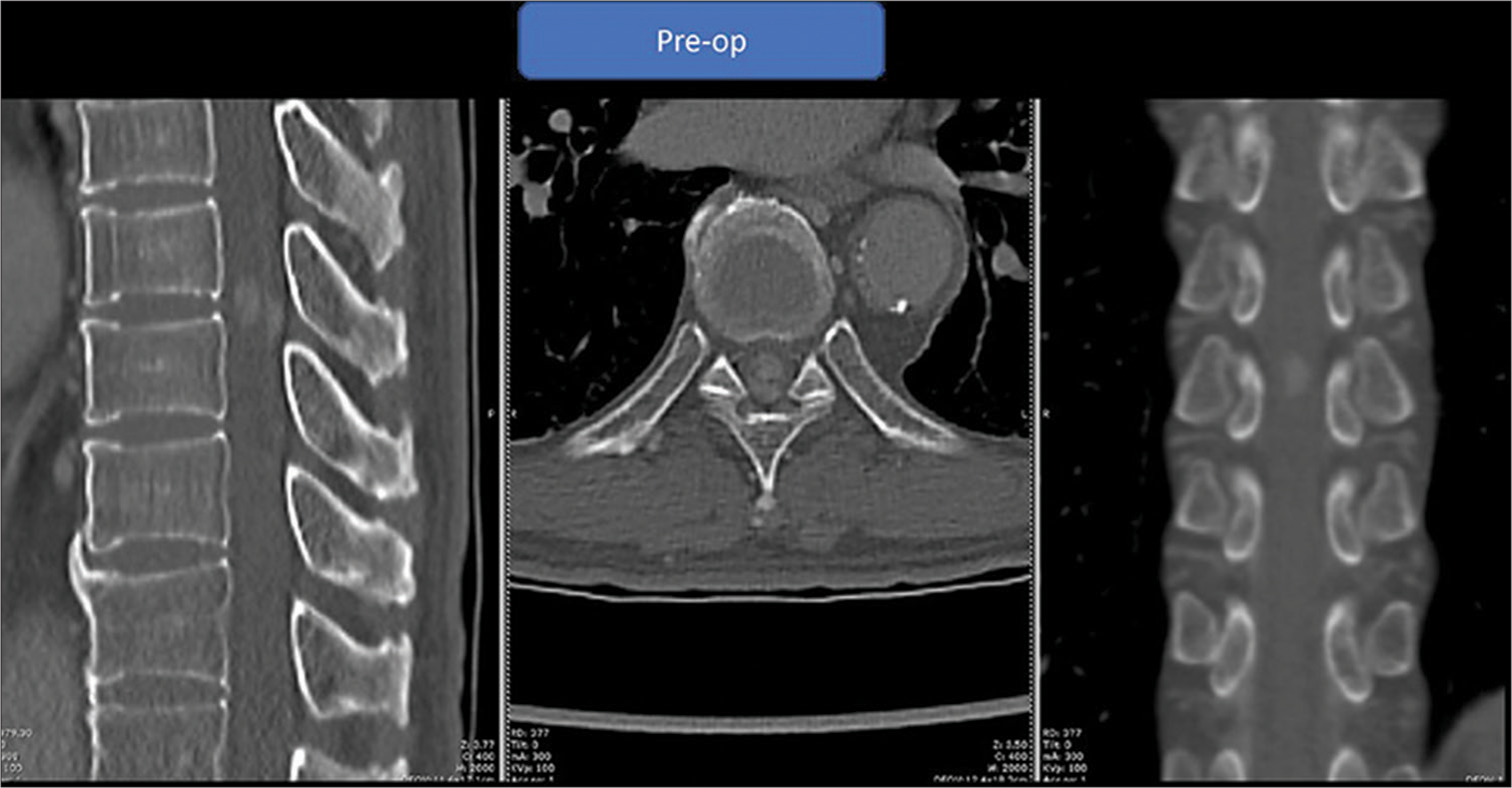
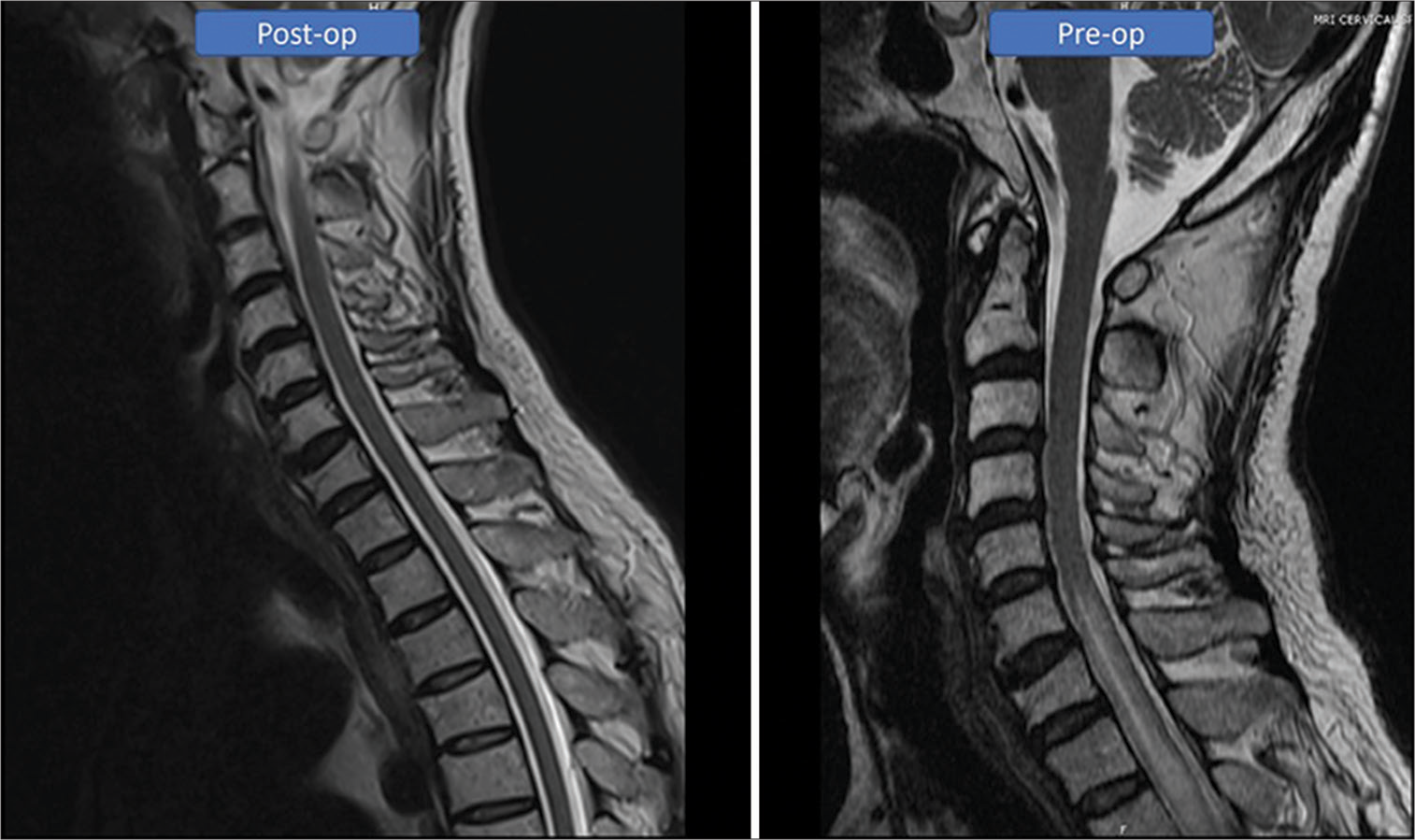
A 63-year-old male initially presented with a history of severe central stenosis for which he underwent an L4-5 laminectomy and in situ fusion performed at a previous facility. His symptoms improved and he was discharged home. However, approximately 2 months later, he developed progressive right leg weakness/numbness that markedly worsened over 2 weeks. On examination, he had 4/5 weakness in the right lower extremity, hyperreflexia, clonus, a T8 level deficit to pinprick appreciation with loss of position/vibration appreciation in both legs. The magnetic resonance imaging (MRI) scan revealed a T8-9 intradural cord lesion with both intra- and extramedullary components. There was also a high T2-weighted cord signal extending from the thoracic through the lower cervical spinal segments [
Neurosurgical intervention
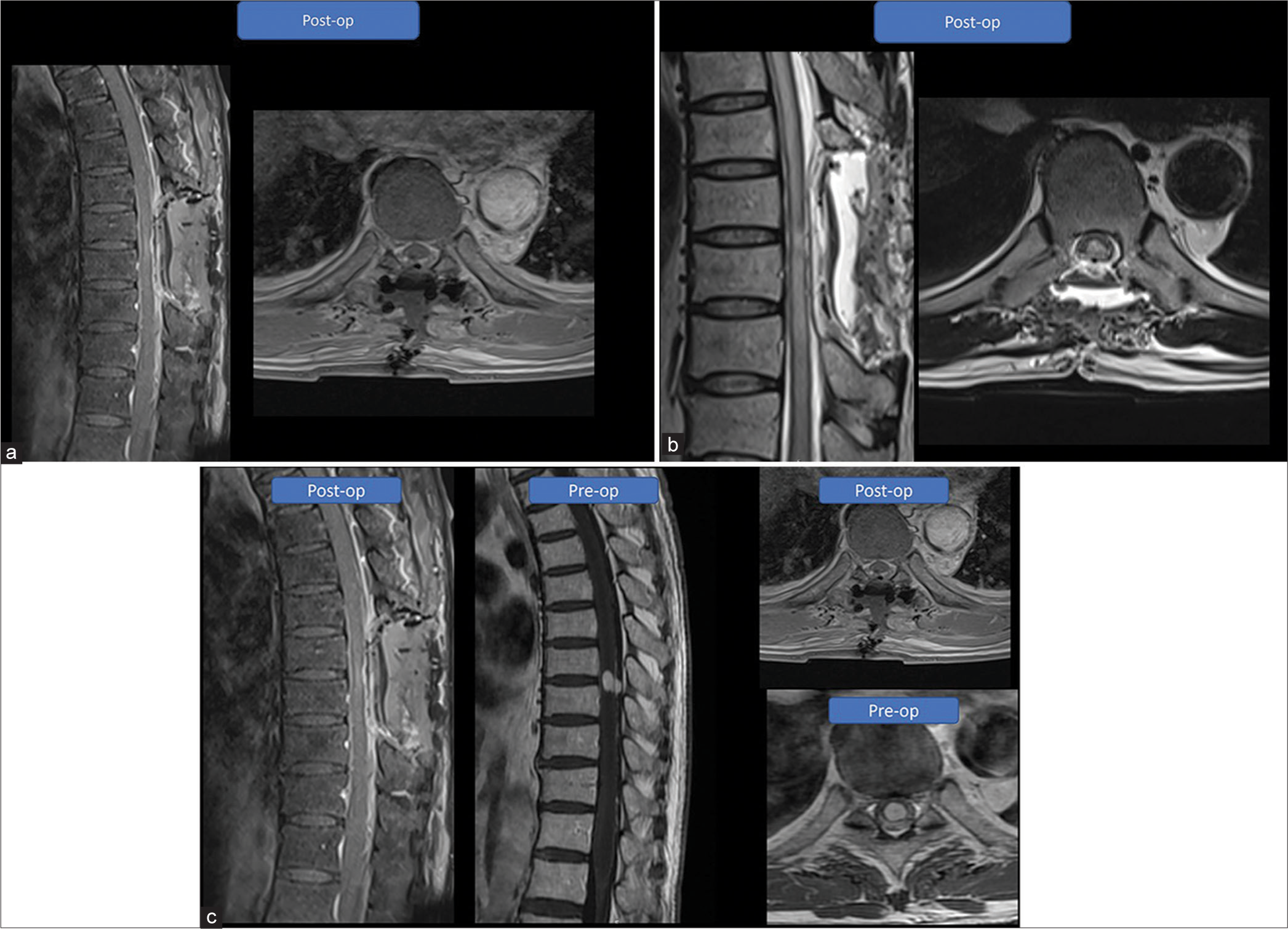
Surgery was performed using intraoperative motor evoked potentials (MEPs), somatosensory evoked potentials (SEPs), and free running electromyography. Before surgery, SEPs were decreased in the right lower extremity versus left. A midline T8-9 laminectomy and durotomy were performed under fluoroscopy. The extramedullary component of the tumor, which appeared hypervascular, was visible on the pial surface. Careful microdissection and excision techniques were used to remove the tumor through a midline myelotomy. As anticipated, SEPs transiently decreased in both lower extremities on splitting the dorsal columns and the MEP in the right lower extremity further decreased during mobilization of the tumor; however, both returned to baseline within several minutes following complete tumor resection. Intraoperative ultrasound confirmed total tumor resection and routine dural/wound closure followed.
Postoperative course
Postoperatively, there were no complications. The MRI demonstrated gross total resection of the tumor and the high T2-weighted cord signal was diminished [
DISCUSSION
Capillary hemangiomas of the spinal cord are rare.[
MRI findings
Capillary hemangiomas are consistently isointense on T1-weighted imaging, hyperintense on T2-weighted imaging, and markedly enhance with contrast. They are typically well-marginated, which is a feature that helps to differentiate them from other intramedullary lesions (i.e., astrocytomas).[
Treatment
The optimal treatment regimen for these lesions is gross total en bloc resection.[
Our patient demonstrated significant improvement in his right lower extremity strength and improved dorsal column dysfunction at 12-month follow-up.
CONCLUSION
We presented a 63-year-old male with an intramedullary/ extramedullary capillary hemangioma at the T8-9 level that was successfully completely excised leaving the patient with a mild residual paraparesis.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abe M, Tabuchi K, Tanaka S, Hodozuka A, Kunishio K, Kubo N. Capillary hemangioma of the central nervous system. J Neurosurg. 2004. 101: 73-81
2. Andaluz N, Balko MG, Stanek J, Morgan C, Schwetschenau PR. Lobular capillary hemangioma of the spinal cord: Case report and review of the literature. J Neurooncol. 2002. 56: 261-4
3. Choi BY, Chang KH, Choe G, Han MH, Park SW, Yu IK. Spinal intradural extramedullary capillary hemangioma: MR imaging findings. AJNR Am J Neuroradiol. 2001. 22: 799-802
4. Gonzalez R, Spears J, Bharatha A, Munoz DG. Spinal lobular capillary hemangioma with an intramedullary component. Clin Neuropathol. 2014. 33: 38-41
5. Hida K, Tada M, Iwasaki Y, Abe H. Intramedullary disseminated capillary hemangioma with localized spinal cord swelling: Case report. Neurosurgery. 1993. 33: 1099-101
6. Kasukurthi R, Ray WZ, Blackburn SL, Lusis EA, Santiago P. Intramedullary capillary hemangioma of the thoracic spine: Case report and review of the literature. Rare Tumors. 2009. 1: e10
7. Kelleher T, Aquilina K, Keohane C, O’Sullivan MG. Intramedullary capillary haemangioma. Br J Neurosurg. 2005. 19: 345-8
8. Nowak DA, Widenka DC. Spinal intradural capillary haemangioma: A review. Eur Spine J. 2001. 10: 464-72
9. Nowak DA, Gumprecht H, Stölzle A, Lumenta CB. Intraneural growth of a capillary haemangioma of the cauda equina. Acta Neurochir (Wien). 2000. 142: 463-7 discussion 467-8
10. Rivierez M, Heyman D, Jouannelle A, Arfi S. Capillary hemangioma of the spinal cord. A new case. Neurochirurgie. 2002. 48: 440-4
11. Roncaroli F, Scheithauer BW, Deen HG. Multiple hemangiomas (hemangiomatosis) of the cauda equina and spinal cord. Case report. J Neurosurg. 2000. 92: 229-32
12. Roncaroli F, Scheithauer BW, Krauss WE. Capillary hemangioma of the spinal cord. Report of four cases. J Neurosurg. 2000. 93: 148-51
13. Tunthanathip T, Rattanalert S, Oearsakul T, Kanjanapradit K. Spinal capillary hemangiomas: Two cases reports and review of the literature. Asian J Neurosurg. 2017. 12: 556-62
14. Weiss S, Goldblum J, editors. Benign tumors and tumorlike lesions of blood vessels. Enzinger and Weiss’s Soft Tissue Tumors. United States: Mosby; 2001. p. 837-890
15. Wu L, Deng X, Yang C, Xu Y. Intramedullary spinal capillary hemangiomas: Clinical features and surgical outcomes: Clinical article. J Neurosurg Spine. 2013. 19: 477-84
16. Zhu K, He D. Intradural extramedullary capillary hemangioma: A case report and review of the literature. Oncol Lett. 2016. 11: 2896-8