- Department of Neurosurgery, General Hospital of Fortaleza, Fortaleza, Brazil.
- Department of Otorhinolaryngology, Leonardo da Vinci Hospital, Fortaleza, Brazil.
- Department of Radiology, General Hospital of Fortaleza, Fortaleza, Brazil.
Correspondence Address:
Tiago S. F. Holanda, Department of Neurosurgery, General Hospital of Fortaleza, Fortaleza, Brazil.
DOI:10.25259/SNI_584_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tiago S. F. Holanda1, Isnara Mara Freitas Pimentel2, Gabriela Oliveira Gosch1, Daniel Gurgel Fernandes Tavora3, Luiz Anderson Bevilaqua Bandeira1, Flavio Leitao Filho1. Immunocompetent patient with isolated primary fourth ventricle lymphoma. Unusual diagnosis, their pitfalls, and challenges. 14-Oct-2022;13:463
How to cite this URL: Tiago S. F. Holanda1, Isnara Mara Freitas Pimentel2, Gabriela Oliveira Gosch1, Daniel Gurgel Fernandes Tavora3, Luiz Anderson Bevilaqua Bandeira1, Flavio Leitao Filho1. Immunocompetent patient with isolated primary fourth ventricle lymphoma. Unusual diagnosis, their pitfalls, and challenges. 14-Oct-2022;13:463. Available from: https://surgicalneurologyint.com/surgicalint-articles/11935/
Abstract
Background: Primary central nervous system lymphoma (PCNSL) is an uncommon lesion and represent 4% of all central nervous system (CNS) cancers. There have been few reports of localized isolated lymphoma developing in the fourth ventricle, with only 8 previous cases described. We present a case of an immunocompetent patient with isolated fourth ventricle lymphoma who did not have diffusion-weighted imaging (DWI) restriction.
Case Description: A 45-year-old man presented a history of headache, vomiting and weigh loss. Upon clinical examination, he presented bilateral papilledema, multidirectional nystagmus, and gait imbalance. Magnetic resonance imaging showed a solid tumor in fourth ventricle with 1.8 × 1.6 × 1.1 cm. The patient was submitted to a suboccipital telovelar approach. The pathological study showed a neoplasm composed of loose round cells. Immunohistochemistry showed positivity for CD-45 and CD-23. The diagnosis of primary CNS lymphoma of the fourth ventricle was certified. Patient was sent to complementary treatment with hematologist and radiotherapy and chemotherapy were started.
Conclusion: PCNSL is a rare and aggressive pathology with high rates of mortality and recurrence. It requires a multidisciplinary team and multiple therapies to control the disease and deliver better quality of life and prognosis to the patient.
Keywords: Cancer, Central nervous system, Fourth ventricle, Lymphoma
INTRODUCTION
Primary central nervous system lymphoma (PCNSL) is an uncommon lesion. They represent 4% of all CNS cancers. The PCNSL is an aggressive form of extranodal non-Hodgkin’s lymphoma, which represent 6% of the total.[
The anatomical involvement is in deep brain structures such as corpus callosum and basal ganglia. The supratentorial location represents 87% of all cases. In posterior fossa, the brainstem and cerebellum are the most common sites of presentation.[
CASE REPORT
A previously healthy 45-year-old man was admitted to the neurosurgical department with a history of headache, vomiting, and weight loss. The symptoms had started 2 months before admission, and the patient sought medical assistance in others two hospitals. On clinical examination, he presented bilateral papilledema, multidirectional nystagmus, and gait imbalance. Complementary examinations were negative for HIV and the defense cells count was normal.
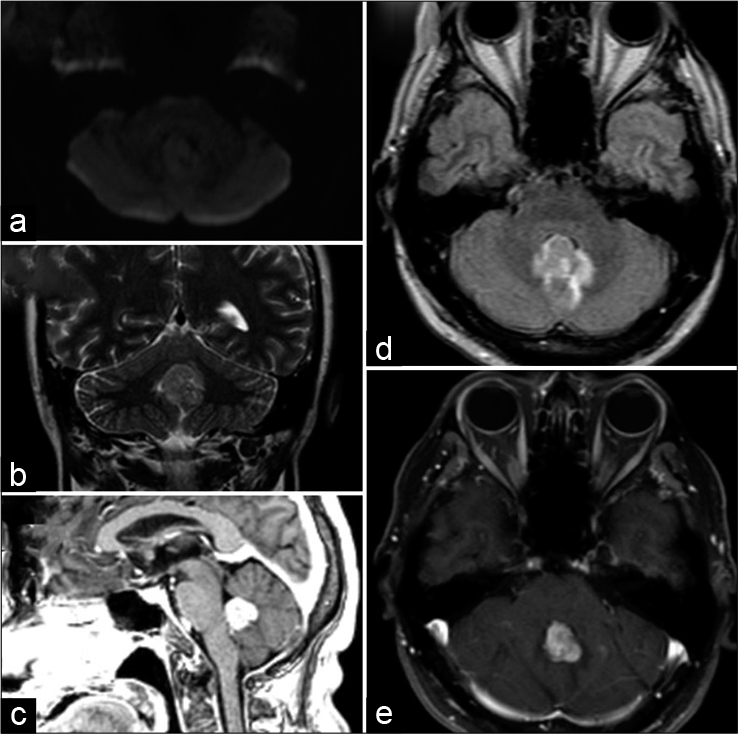
During the radiological investigation, magnetic resonance imaging (MRI) showed a solid tumor in the fourth ventricle with 1.8 × 1.6 × 1.1 cm of size and with the hyper signal on T2 and high contrast uptake on T1, however, with no diffusion-weighted imaging (DWI) restriction [
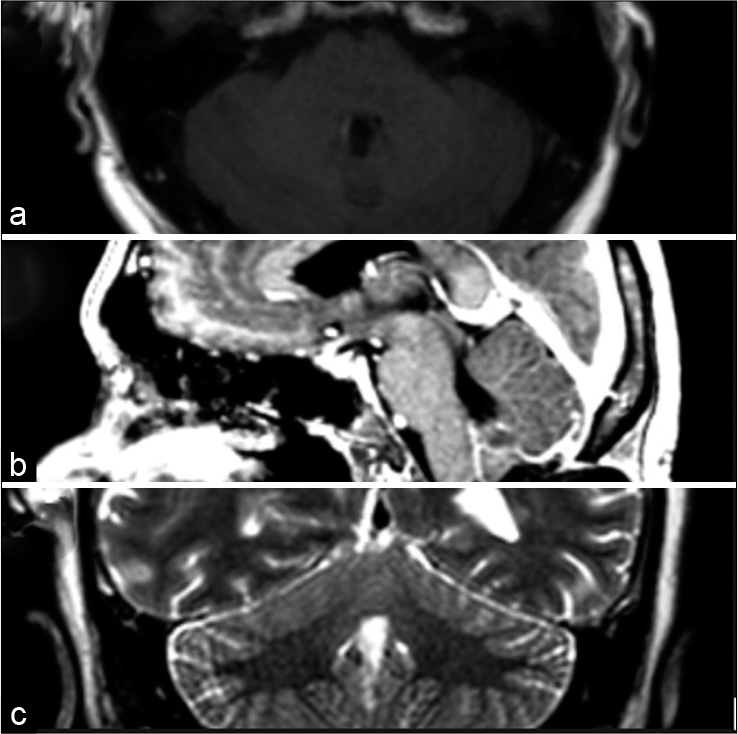
Because of the intracranial hypertension syndrome and the presence of an expansive lesion of the fourth ventricle, the patient was submitted to a suboccipital telovelar approach. During the surgery, a solid gray lesion adherent to the cerebellar vermis and infiltrated the floor of the fourth ventricle was seen, with higher adherence to the roof of the ventricle, however, the tumor appeared to be low vascularized and was pale in color. After debulking, an extracapsular resection was realized. After the surgery, the patient was submitted to a new MRI which showed complete tumor resection [
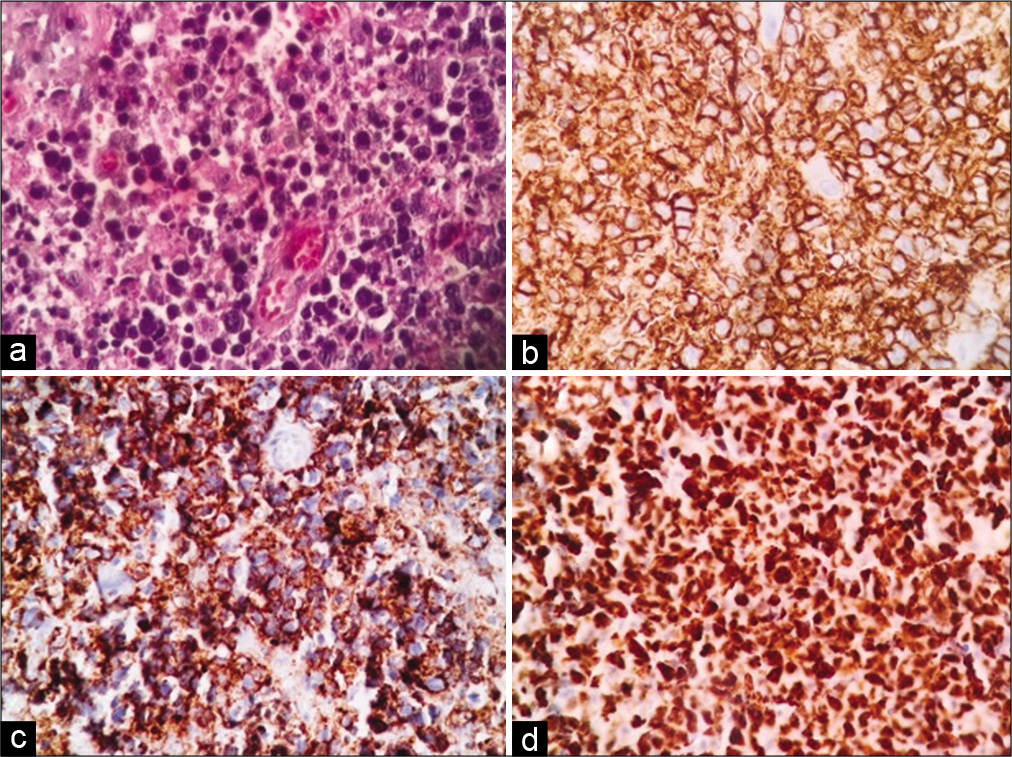
The pathological study showed a neoplasm composed of loose round cells. Immunohistochemistry showed positivity for CD-45, CD-23, and Ki67 in 90% of the cells which concluded the diagnosis of primary CNS lymphoma of the fourth ventricle [
With the lymphoma diagnosis, the patient was sent to complementary treatment with a hematologist, and radiotherapy and chemotherapy were started. Since then, the patient keeps in ambulatorial assistance.
DISCUSSION
PCNSL is an aggressive form of non-Hodgkin lymphoma which is localized in the CNS. They are uncommon lesions that represent approximately 6% of all Lymphomas.[
Immunosuppression is a risk factor for the growth of this pathology and however is more prevalent in descriptions of cases in immunocompetent patients. The onset in adulthood is more prevalent, nevertheless, the mean age of presentation is 65 years[
Clinical presentation is variable.[
The radiologic criteria of evaluation can help with suspicion. If possible, MRI is mandatory because of some specific changes observed as bellow described. In deep brain structures or on multifocal presentation, the presence of contrast uptake and DWI restriction increase the possibility of diagnosis.[
Despite the radiologic information, pathologic confirmation is necessary and can be made for many possible approaches; however, the stereotaxic biopsy and navigation-guided needle biopsy are the most cited because of the minimally invasive technique.[
The lymphoma subtype diagnosed is in 90% of cases B-cell Lymphomas. Less commonly can be present in Burkitt or T-Cell forms. In general, the histologic aspect includes centroblastic cytology and perivascular tropism. CD markers offer a specific diagnosis. CD20, CD19, and CD79 for B-Cell type are the most commonly finds.[
The management is challenging. A multidisciplinary team is necessary, and the stratification depends on age, comorbidities, performance status, and neurologic conditions. Chemotherapy and radiotherapy can be used isolated or combined.[
Surgical approaches are discouraged. The previous analysis showed no benefit in outcome when used alone or combined with adjuvant therapy. Another explanation is that here the disease is multifocal and has infiltrative nature, besides can induce permanent neurological deficits. From this perspective, the surgical approaches are not adequate for incomplete resection.[
The prognosis depends on many variables. Age and performance status are independent prognostic factors. Some authors also describe Ki-67, MUM1, and bcl-6 markers as possible prognosis definers[
Within recent gains in lymphoma therapy, the targeted treatment with immunomodulators has to be noted as an important weapon, mainly reducing tumor recurrence rates.[
CONCLUSION
Despite expansive lesions of fourth ventricle being considered more commonly ependymomas, medulloblastomas, and metastasis, it is possible the diagnosis of lymphoma. In this case, no DWI restriction was observed, which led to microsurgical resection as the first-choice therapy due to the low possibility of lymphoma.
PCNSL is a rare and aggressive pathology with high rates of mortality and recurrence. It is necessary for a multidisciplinary team and multiple therapies to control the disease and deliver better quality of life and prognosis to the patient.
Surgery is necessary to confirm the diagnosis; however, minimally invasive such as stereotaxic biopsy and navigation-guided needle biopsy is important tools for accessing tumor tissue for diagnostic confirmation. Chemotherapy and radiotherapy keep as the principal way of treatment, nevertheless, recent studies showed the importance of immunotherapy in overall survival and recurrence of pathology.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
1. Alabbdulsalam A, Zaidi SZ, Tailor I, Orz Y, Al-Dandan S. Primary Burkitt lymphoma of the fourth ventricle in an immunocompetent young patient. Case Rep Pathol. 2014. 2014: 630954
2. Ansell SM, Caligaris-Cappio F, Maloney DG. Immunotherapy in lymphoma. Hematol Oncol. 2017. 35: 88-91
3. Bokhari R, Ghanem A, Alahwal M, Baeesa S. Primary isolated lymphoma of the fourth ventricle in an immunocompetent patient. Case Rep Oncol Med. 2013. 2013: 614658
4. Calimeri T, Steffanoni S, Gagliardi F, Chiara A, Ferreri AJ. How we treat primary central nervous system lymphoma. ESMO. 2021. 6: 1-5
5. Citterio G, Reni M, Gatta1 G, Ferreri AJ. Primary central nervous system lymphoma. Crit Rev Oncol Hematol. 2017. 113: 97-110
6. Correia CE, Schaff LR, Grommes C. Central nervous system lymphoma. Cancer J. 2020. 26: 241-52
7. Fabiano A, Syriac S, Fenstermaker RA, Qiu J. Primary fourth ventricular B-cell lymphoma in an immunocompetent patient. Clin Neurophatol. 2014. 33: 94-7
8. Haegelen C, Riffaud L, Bernard M, Morandi X. Primary isolated lymphoma of the fourth ventricle: Case report. J Neurooncol. 2001. 51: 129-31
9. Hill CS, Khan AF, Bloom S, McCartney S. A rare case of vomiting: Fourth ventricular B-cell lymphoma. J Neurooncol. 2009. 93: 261-2
10. Hsu H, Lai PH, Tseng HH, Hsu SS. Primary solitary lymphoma of the fourth ventricle. Int J Surg Case Rep. 2015. 14: 23-5
11. Liao CH, Lin SC, Hung SC, Hsu SP, Ho DM, Shih YH. Primary large B-cell lymphoma of the fourth ventricle. J Clin Neurosci. 2014. 21: 180-3
12. Ollila TA, Olszewski AJ. Extranodal diffuse large B cell lymphoma: Molecular features, prognosis, and risk of central nervous system recurrence. Curr Treat Options Oncol. 2018. 19: 19-38
13. Werneck LC, Hatschbach Z, Mora AH, Novak EM. Meningitis caused by primary lymphoma of the central nervous system. Report of a case. Arq Neuropsiquiatr. 1977. 35: 366-72