- Department of Neurosurgery, Nagareyama Central Hospital, Nagareyama, Chiba, Japan.
Correspondence Address:
Takanori Uchida, Department of Neurosurgery, Nagareyama Central Hospital, Nagareyama, Chiba, Japan.
DOI:10.25259/SNI_324_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takanori Uchida, Ryuzaburo Kanazawa, Tetsuhiro Higashida, Saiko Watanabe, Takao Kono. Importance of preoperative coronary artery examination before performing procedures for carotid artery stenosis. 30-Jun-2023;14:229
How to cite this URL: Takanori Uchida, Ryuzaburo Kanazawa, Tetsuhiro Higashida, Saiko Watanabe, Takao Kono. Importance of preoperative coronary artery examination before performing procedures for carotid artery stenosis. 30-Jun-2023;14:229. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12383
Abstract
Background: Carotid artery stenosis and coronary artery disease (CAD) often occur simultaneously, with one being an important risk factor in the treatment of the other. This study aimed to perform coronary computed tomography angiography (CTA) as a preoperative evaluation for carotid artery stenosis treatment.
Methods: We retrospectively reviewed cases of carotid endarterectomy (CEA) and carotid artery stenting (CAS) performed at our hospital as well as CAD complications.
Results: Among the 54 and 166 CEA and CAS cases from May 2014 to February 2022, 53 and 148 cases were analyzed for atherosclerotic stenosis, respectively. Among those who underwent CEA and CAS, 7 (13.2%) and 17 (11.5%) received percutaneous coronary intervention (PCI), 44 (83%) and 97 (65.5%) received symptomatic carotid stenosis treatment and 43 (81.1%) and 110 (74.3%) received preoperative coronary CTA, respectively. Coronary artery stenosis was noted in 14 (32.6%) and 46 (41.8%) patients who had undergone CTA in the CEA and CAS groups, respectively. PCI before carotid treatment was performed in two cases in the CEA group (3.8% of all patients who had undergone CEA) and eight cases in the CAS group (5.4% of all patients who had undergone CAS).
Conclusion: Screening may detect asymptomatic coronary artery lesions in carotid artery stenosis even in patients without chest symptoms and suspicion of ischemic heart disease. Preoperative coronary artery screening is important considering that pre and postoperative coronary artery treatment may improve long-term prognosis.
Keywords: Carotid artery stenosis, Carotid artery stenting, Carotid endarterectomy, Coronary artery disease, Coronary computed tomography angiography
INTRODUCTION
In general, atherosclerotic diseases, including carotid artery stenosis, are strongly associated with systemic vascular lesions, with coronary artery disease (CAD) being particularly common. However, both carotid artery stenosis and CAD are individually important risk factors in the treatment of the other. We have experienced cases of myocardial infarction during the perioperative period of carotid artery stenosis treatment and have since performed coronary computed tomography angiography (CTA) for preoperative evaluation. In the present study, we retrospectively reviewed cases of carotid endarterectomy (CEA) and carotid artery stenting (CAS) performed at our hospital as well as CAD complications.
MATERIALS AND METHODS
Among the 54 and 166 cases who had undergone CEA and CAS from May 2014 to February 2022, 53 and 148 cases were analyzed, respectively, excluding those who had undergone internal carotid artery dissection, acute revascularization, and revision after CAS.
Coronary CTA was preoperatively performed but not in cases with nonatherosclerotic lesions, such as those requiring internal carotid artery dissection, cases in which the patient had already visited another hospital for cardiac examination and treatment, cases who had already undergone retreatment for carotid artery stenosis, and cases in which performing necessary respiratory pause during imaging was difficult due to cognitive impairment.
RESULTS
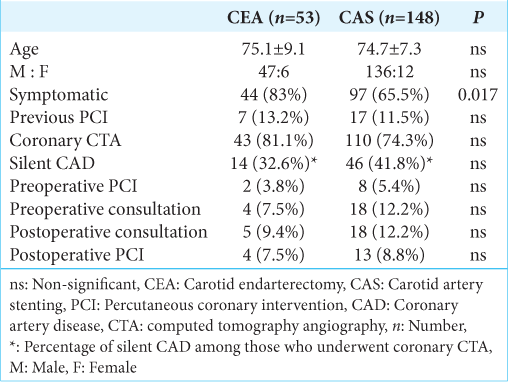
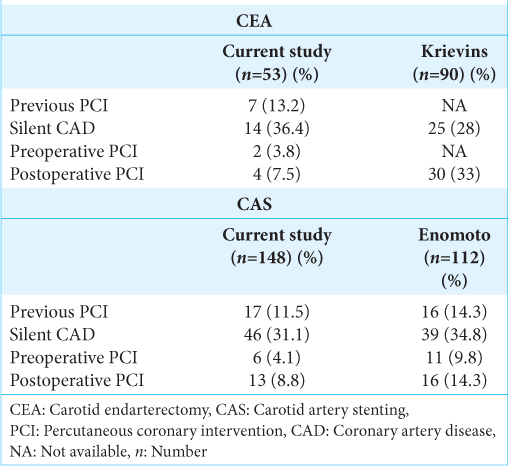
The characteristics of the included patients are summarized in
Preoperative consultations regarding coronary CTA for coronary artery lesions were not performed in patients who had undergone previous examinations or PCI and were still attending the hospital. Preoperative consultation with a cardiologist was performed in four patients in the CEA group, all of whom had an abnormal CTA. In addition, 18 patients in the CAS group underwent preoperative consultation, of whom nine had abnormal coronary CTA. PCI was performed before carotid therapy in two cases in the CEA group (3.8% of all patients who had undergone CEA) and eight cases in the CAS group (5.4% of all patients who had undergone CAS). Postoperative consultation with a cardiologist was performed in five patients in the CEA group, of whom two had abnormalities on coronary CTA, and 18 patients in the CAS group, of whom 14 had abnormalities on CTA. Postoperative PCI was performed in four and 13 patients in the CEA and CAS groups, respectively. Perioperative complications, such as angina pectoris or myocardial infarction, were not observed.
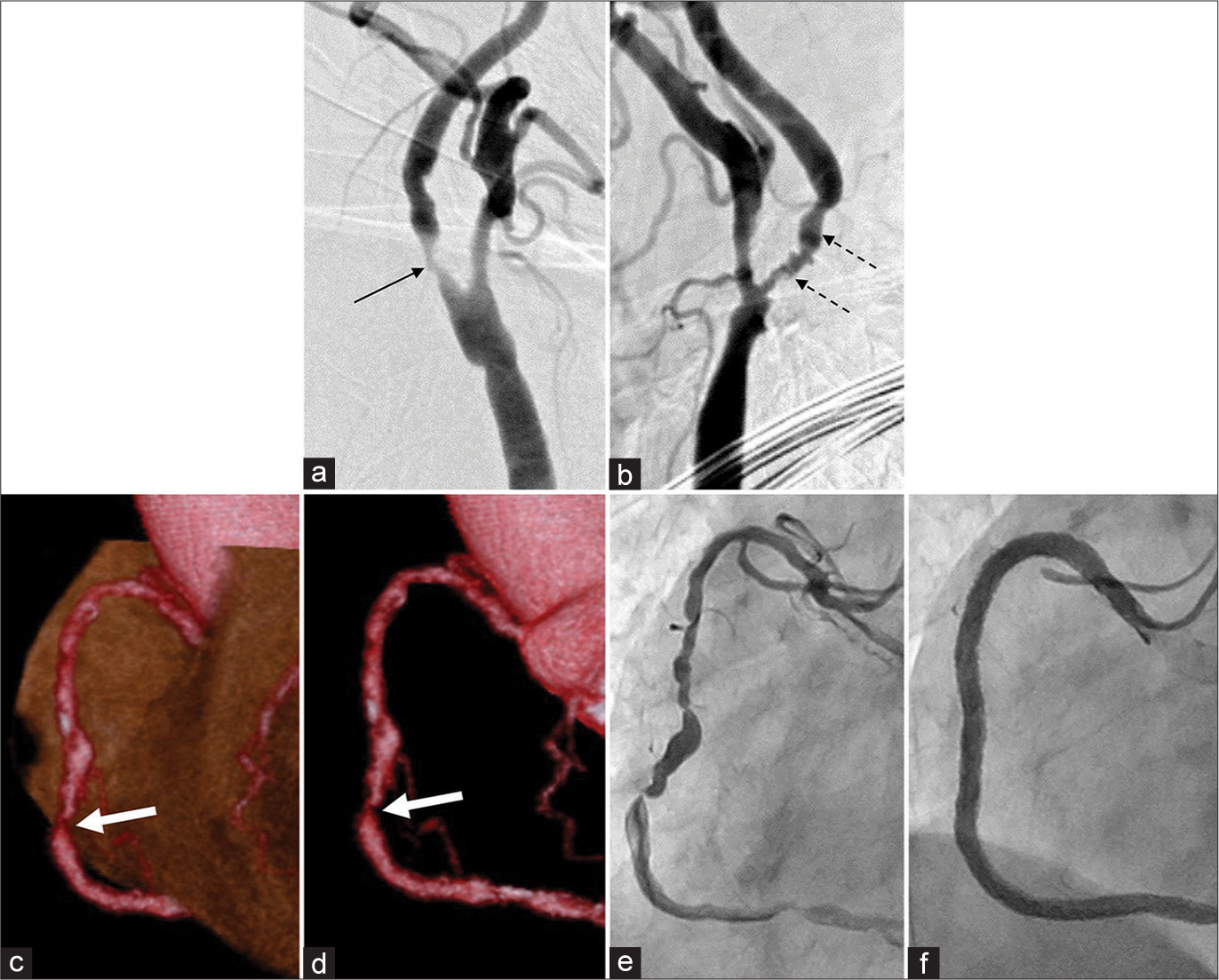
Case 1: 70-year-old female
The patient was 70-year-old during PCI and 71-years-old during carotid artery treatment. She was first examined at our hospital after carotid ultrasonography when bilateral internal carotid artery stenosis was detected. Her peak systolic flow velocity was >400 cm/s bilaterally, and angiography was performed for carotid artery treatment despite no symptoms of stenosis [
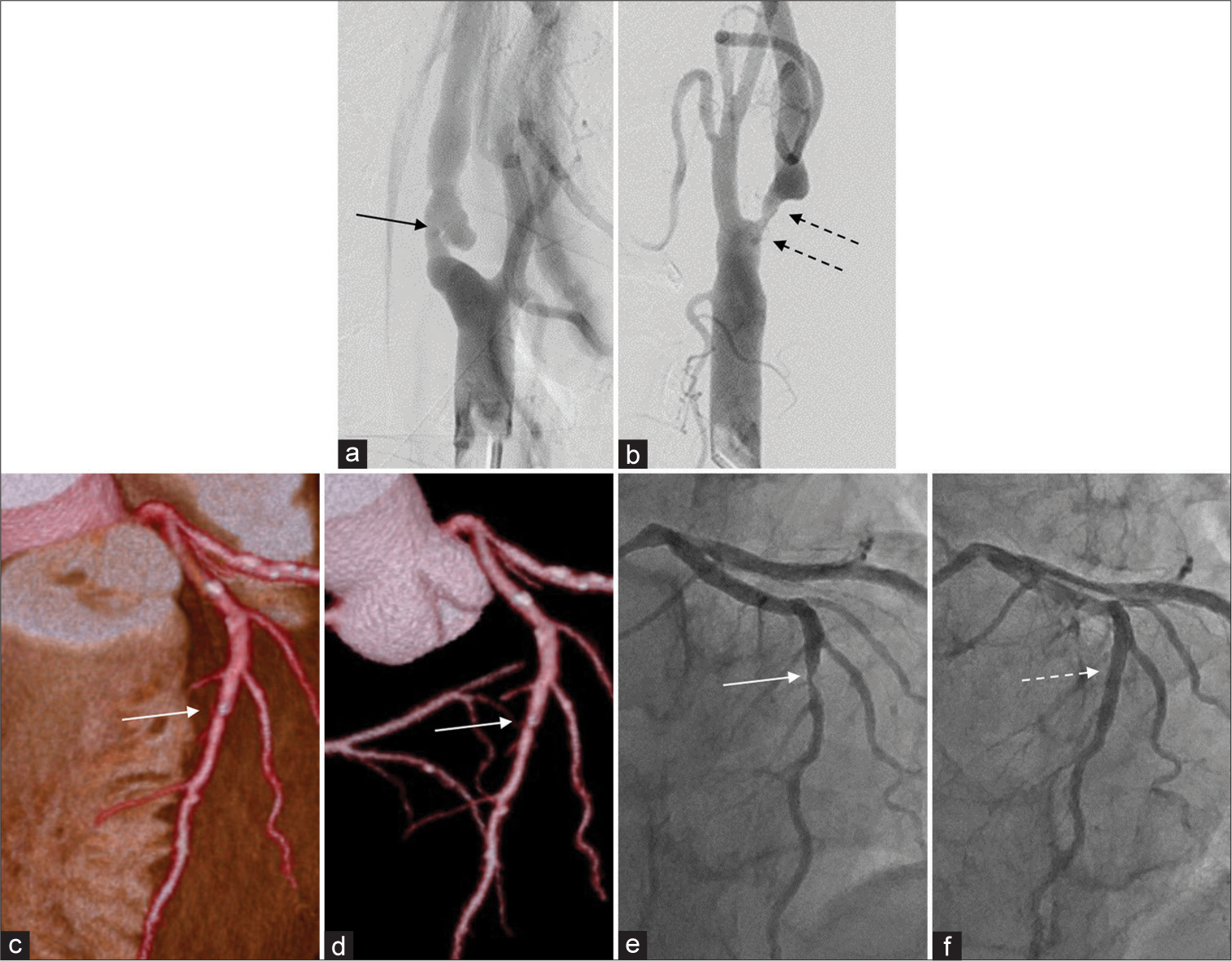
Case 2: 73-year-old male
The patient was 73-year-old during carotid artery treatment and 75-year-old during PCI. He was diagnosed with symptomatic left internal carotid artery stenosis caused by amaurosis fugax. Carotid ultrasonography revealed low echogenicity; time-of-flight magnetic resonance angiography revealed high-intensity plaque and angiography confirmed bilateral internal carotid artery stenosis [
Figure 2:
Case 2. Right carotid artery stenosis (arrow, a) and left carotid artery stenosis (dotted arrows, b). Left anterior descending artery mild calcification (white arrow, c and d) in preoperative examination before carotid artery treatment. After 1½ year, percutaneous coronary intervention was performed in the same artery (e: white arrow, f: white dotted arrow).
DISCUSSION
Regarding the possibility of complications and sequelae between cerebral infarction and CAD, reports have shown that approximately 15.8% of patients with atherothrombotic cerebral infarction had a history of CAD,[
Although CTA is inferior to coronary angiography in terms of its accuracy in assessing stenosis rate, it has comparable ability in detecting the presence of coronary stenotic lesions and myocardial complications during the 1st year after the procedure. Preoperative consultation results and PCI through coronary CTA may have prevented perioperative complications, such as angina pectoris and myocardial infarction, and postoperative consultation with the cardiologist included patients who had no significant abnormalities on preoperative CTA. This indicates the need for follow-up considering CAD even after treatment. The disadvantage of CTA lies in its difficulty in accurately assessing the stenosis rate due to calcification; as such, coronary angiography and FFR of CT exhibit better accuracy in assessing stenosis rate and ischemia. In our case, screening through CTA detected stenosis and ischemia at rates similar to those reported in the previous studies, which may lead to lower perioperative complications and improved long-term prognosis through pre and postoperative coronary artery treatment.
Limitations
The present study had some limitations. Given that not all patients received consultation from a cardiologist before surgery, treatment priorities may have been biased toward carotid artery treatment, although the study was retrospective in nature and the presence of coronary CTA was determined by the radiology department.
CONCLUSION
Screening may detect asymptomatic coronary artery lesions in carotid artery stenosis even in patients without chest symptoms and suspicion of ischemic heart disease. Preoperative coronary artery screening is important considering that pre and postoperative coronary artery treatment may improve long-term prognosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Amarenco P, Bogousslavsky J, Callahan A, Goldstein LB, Hennerici M, Rudolph AE. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006. 355: 549-59
2. Daly C, Rodriguez HE. Carotid artery occlusive disease. Surg Clin North Am. 2013. 93: 813-32
3. Enomoto Y, Yoshimura S, Yamada K, Kawasaki M, Nishigaki K, Minatoguchi S. Silent coronary artery disease in Japanese patients undergoing carotid artery stenting. J Stroke Cerebrovasc Dis. 2013. 22: 1163-8
4. Hertzer NR, Young JR, Beven EG, Graor RA, O’Hara PJ, Ruschhaupt WF. Coronary angiography in 506 patients with extracranial cerebrovascular disease. Arch Intern Med. 1985. 145: 849-52
5. Heyden S, Heyman A, Goree JA. Nonembolic occlusion of the middle cerebral and carotid arteries-a comparison of predisposing factors. Stroke. 1970. 1: 363-9
6. Hoffmann U, Ferencik M, Cury RC, Pena AJ. Coronary CT angiography. J Nucl Med. 2006. 47: 797-806
7. Krievins D, Zellans E, Latkovskis G, Jegere S, Kumsars I, Kaufmanis K. Diagnosis and management of silent coronary ischemia in patients undergoing carotid endarterectomy. J Vasc Surg. 2021. 73: 533-41
8. Leys D, Woimant F, Ferrieres J, Bauters C, Touboul PJ, Guerillot M. Detection and management of associated atherothrombotic locations in patients with a recent atherothrombotic ischemic stroke: Results of the DETECT survey. Cerebrovasc Dis. 2006. 21: 60-6
9. Mahmoudi M, Hill PC, Xue Z, Torguson R, Ali G, Boyce SW. Patients with severe asymptomatic carotid artery stenosis do not have a higher risk of stroke and mortality after coronary artery bypass surgery. Stroke. 2011. 42: 2801-5
10. Mitchell JR, Schwartz CJ. Relationship between arterial disease at different sites. A study of the aorta and coronary, carotid, and iliac arteries. Br Med J. 1962. 1: 1293-301
11. Sanguigni V, Gallu M, Strano A. Incidence of carotid artery atherosclerosis in patients with coronary artery disease. Angiology. 1993. 44: 34-8
12. Silverstein A, Hollin S. Internal carotid vs middle cerebral artery occlusions: Clinical differences. Arch Neurol. 1965. 12: 468-71
13. Solberg LA, McGarry PA, Moossy J, Strong JP, Tejada C, Löken AC. Severity of atherosclerosis in cerebral arteries, coronary arteries, and aortas. Ann N Y Acad Sci. 1968. 149: 956-73
14. Stein PD, Beemath A, Kayali F, Skaf E, Sanchez J, Olson RE. Multidetector computed tomography for the diagnosis of coronary artery disease: A systematic review. Am J Med. 2006. 119: 203-16
15. Tanimoto S, Ikari Y, Tanabe K, Yachi S, Nakajima H, Nakayama T. Prevalence of carotid artery stenosis in patients with coronary artery disease in Japanese population. Stroke. 2005. 36: 2094-8
16. Touze E, Varenne O, Chatellier G, Peyrard S, Rothwell PM, Mas JL. Risk of myocardial infarction and vascular death after transient ischemic attack and ischemic stroke: A systematic review and meta-analysis. Stroke. 2005. 36: 2748-55
17. Zhang J, Xu R, Liu P, Fan X, Ye Z. Prevalence of carotid artery stenosis in Chinese patients with angina pectoris. J Thorac Dis. 2015. 7: 2300-6