- Department of Neurosurgery, Keio University Hospital, Shinjuku-ku, Tokyo, Japan
Correspondence Address:
Ryota Tamura
Department of Neurosurgery, Keio University Hospital, Shinjuku-ku, Tokyo, Japan
DOI:10.4103/2152-7806.184579
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tamura R, Takahashi S, Horikoshi T, Yoshida K. Improvement of long-term blindness caused by compression from inner-third sphenoid wing meningioma after optic canal decompression: An extremely rare case report. Surg Neurol Int 23-Jun-2016;7:67
How to cite this URL: Tamura R, Takahashi S, Horikoshi T, Yoshida K. Improvement of long-term blindness caused by compression from inner-third sphenoid wing meningioma after optic canal decompression: An extremely rare case report. Surg Neurol Int 23-Jun-2016;7:67. Available from: http://surgicalneurologyint.com/surgicalint_articles/improvement-of-long%e2%80%91term-blindness-caused-by-compression-from-inner%e2%80%91third-sphenoid-wing-meningioma-after-optic-canal-decompression-an-extremely-rare-case-report/
Abstract
Background:There has been no previous case report of a patient whose visual acuity improved after long-term blindness caused by tumor invasion into the optic canal.
Case Description:A 65-year-old Asian woman presented with a 6-month history of blindness caused by a meningioma located on the inner third of the sphenoid ridge. An operation was performed to prevent further tumor invasion into the cavernous sinus and contralateral optic nerve. During surgery, optic canal decompression was performed using an epidural approach. Subtotal removal of the tumor was achieved. Two days after the surgery, her left visual acuity recovered from blindness.
Conclusion:Normally, long-term blindness caused by optic nerve compression by a brain tumor is regarded as irreversible, and even a surgical excision of the optic nerve is performed in some cases. However, because we experienced a case in which the patient recovered from long-term blindness after optic canal decompression, we believe that this surgical procedure should definitely be considered as an option.
Keywords: Blindness, inner-third sphenoid wing meningioma, optic canal decompression
INTRODUCTION
Inner-third sphenoid wing meningioma is known to cause partial or complete loss of vision. Once the vision is disturbed, it is considered difficult to achieve good visual outcome after tumor surgery. The difficulty comes from the fact that this type of meningioma involves optic nerve ischemia as well as compression as a mechanism of visual disturbance.[
CASE DESCRIPTION
Onset and course
A 60-year-old Asian woman presented to a nearby hospital with the chief complaint of left facial palsy. A diagnosis of Bell's palsy was made, however at the same time, magnetic resonance imaging (MRI) of the head revealed an incidental meningioma located on the inner-third of the left sphenoid ridge.
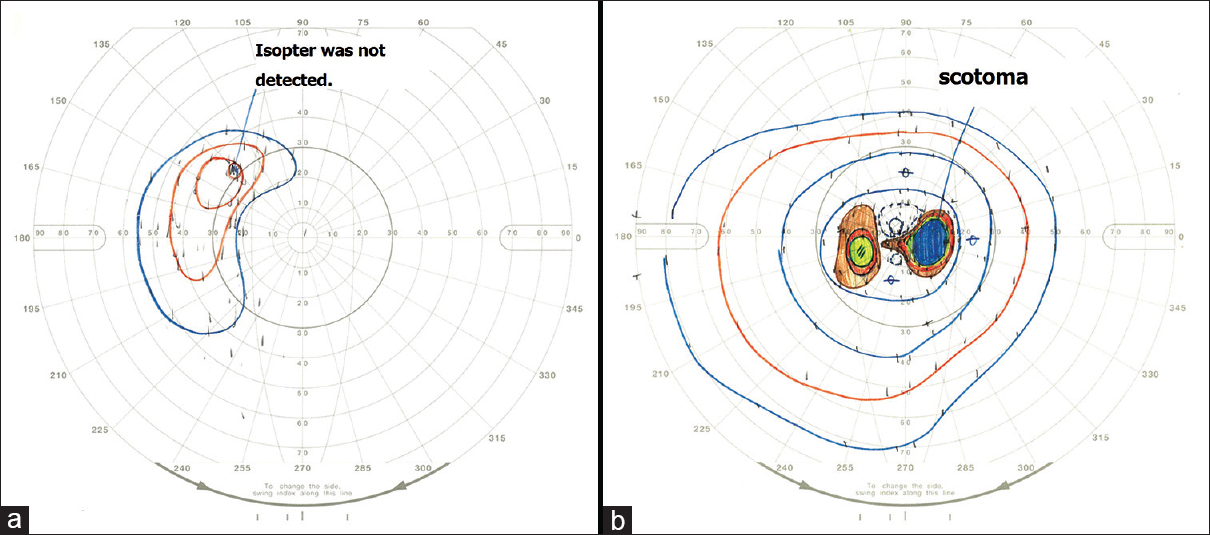
The tumor was initially observed, and meanwhile, symptoms of Bell's palsy gradually relieved. Two years after the diagnosis of meningioma, she began to suffer from progressive visual deterioration and central scotoma on her left eye. The visual acuity was completely lost 2.5 years after the diagnosis. She was finally referred to our hospital 3 years after the diagnosis. Head MRI taken at our hospital showed enlargement of the tumor. A neurological examination revealed no pupillary disturbances, including pupillary light reflex and pupil size. Slight Bell's palsy was also observed, however, it had improved by then. Therefore, we considered that Bell's palsy and the intracranial meningioma had no connection. We consulted with an ophthalmologist about the patient's visual acuity. After the examination by an ophthalmologist, the patient was revealed to be completely blind on her left eye with no light perception. Preoperative visual field examination and visual evoked potential (VEP) was not performed for this reason.
Preoperative radiological findings
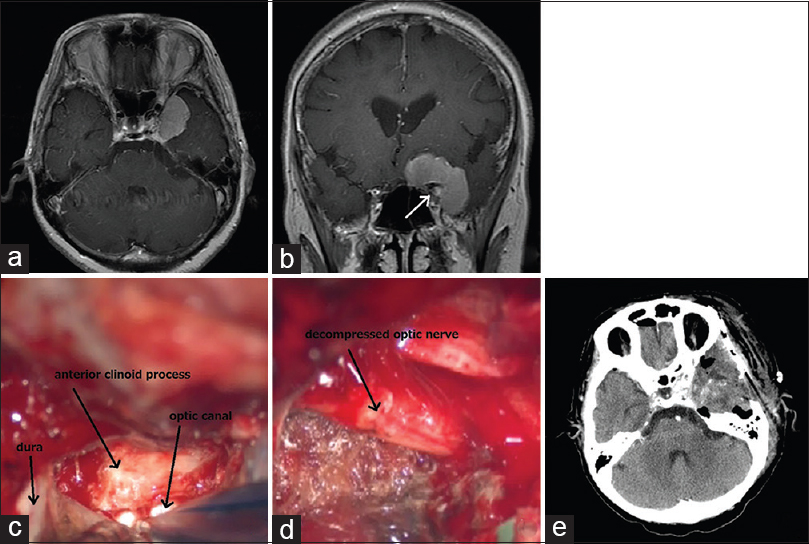
Computed tomography (CT) showed an isodense, well-demarcated mass lesion, 35 mm in diameter, that was attached to the inner-third of the left sphenoid ridge. The lesion showed no apparent calcification inside and was enhanced strongly with intravenous administration of contrast media. Bone-image CT showed thickening of the anterior clinoid process. On MRI, the lesion was hyperintense on T2-weighted imaging. In addition, the lesion was attached to the lateral wall of the cavernous sinus, anterior clinoid process, and frontal skull base [
Figure 1
(a) Contrast-enhanced axial magnetic resonance imaging (MRI) before operation shows the inner-third sphenoid wing meningioma. (b) Contrast-enhanced coronal MRI before operation shows tumor invasion into the optic canal (arrow: Optic canal invasion). (c) The anterior clinoid process was removed, and optic canal decompression was performed. (d) The tumor component around the optic nerve was removed as much as possible. However, the optic nerve had already become thin and slightly atrophic. (e) CT scanning after operation shows 95% removal of the inner-third sphenoid wing meningioma
Operation
The main purpose of the operation was not to improve visual acuity but to prevent further tumor invasion into the cavernous sinus and contralateral optic nerve. This was why VEP was not monitored during the operation. However, because the pupillary light reflex was not disturbed, we considered that there was still a possibility of optic nerve recovery. Thus, we took the precaution of performing optic canal decompression at the same time.
Tumor removal was performed via a left pterional approach. A surgical navigation system (Medtronic, Tokyo, Japan) and electrooculography were used. Briefly, the temporal dura was detached from the middle cranial base, and the middle meningeal artery passing the foramen spinosum was identified, coagulated, and cut.
Then, the left anterior clinoid process was removed, and optic canal decompression was performed by an extradural approach [
Postoperative course
Subtotal resection (95% removal) of the tumor was confirmed by postoperative CT images [
DISCUSSION
There have been some reports regarding the relationship between meningioma and visual acuity disturbance. Meningiomas located on the inner-third of the sphenoid ridge are known to cause visual impairment of the ipsilateral eye in 40~60% of the patients. This is mainly due to the compression of the optic nerve at the entrance and/or within the optic canal; compression of the intraorbital segment of the optic nerve is known to have less impact on visual acuity.[
Prognosis of visual acuity disturbance due to meningioma is known to correlate with the preoperative duration of symptoms and extent of visual impairment.[
As for our case, the duration of visual symptoms was 1 year and the extent of disturbance was complete blindness. Although a poor postoperative visual prognosis was anticipated, we chose to perform optic canal decompression along with tumor resection because papillary light reflex was maintained, which suggested that there was still a chance of optic nerve recovery.
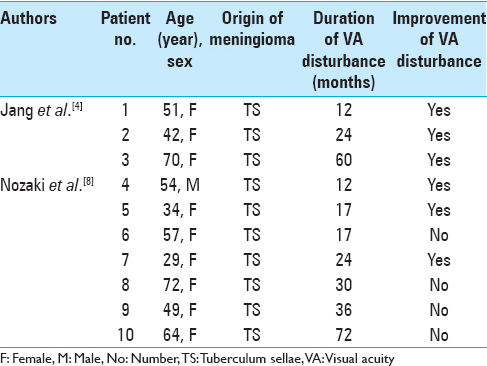
The relationship of symptom duration and postoperative visual outcome in cases of TS meningiomas that underwent optic canal decompression is summarized in
We used reports of TS meningioma because there were no reports of inner-third sphenoid wing meningioma that contained such data. Although it may be difficult to compare the visual prognosis of these two meningiomas, we would like to emphasize that both have similar mechanisms of visual disturbance, which are compression and ischemia of the optic nerve.[
After excluding cases without detailed history of the patients’ visual disturbance, we found 10 cases that underwent optic canal decompression. There were 6 patients with preoperative visual disturbance for 1–2 years. None of them had complete blindness. After operation, all but one experienced visual improvement. There were 4 patients with preoperative visual disturbance for more than 2 years. None of them had complete blindness either. After operation, the case with a 5-year history of visual disturbance experienced visual improvement. The degree of visual acuity improvement was from 0.06 to 0.1. In total, 6 out of 10 cases (60%) had achieved visual improvement after optic canal decompression. The extent of improvement varied among the cases probably due to the differences in duration of symptoms and extent of preoperative visual disturbance, as described earlier.
Taking these results into account, including the result of our case, we believe that optic canal decompression should definitely be considered as an option in cases of meningioma with long-term visual deterioration or blindness. Last, but not the least, we would like to note that the procedure of optic canal decompression is not without risk because it may cause further deterioration of visual acuity and even loss of vision. The surgical indication must certainly take into consideration factors such as age, extent of tumor invasion, and preoperative visual acuity.
CONCLUSION
Because we experienced a case of meningioma in which the patient recovered from long-term blindness, we believe that optic canal decompression should definitely be considered as an option. Factors such as age, degree of tumor invasion, and preoperative visual acuity need to be taken into account when determining surgical indications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Mefty O. Clinoidal meningiomas. J Neurosurg. 1990. 73: 840-9
2. Chicani CF, Miller NR. Visual Outcome in surgically treated suprasellar meningiomas. J Neuroophthalmol. 2003. 23: 3-10
3. Galal A, Faisal A, Al-Werdany M, El Shehaby A, Lotfy T, Moharram H. Determinants of postoperative visual recovery in suprasellar meningioma. Acta Neurochir. 2010. 152: 69-77
4. Jang WY, Jung S, Jung TY, Moon KS, Kim IY. The contralateral subfrontal approach can simplify surgery and provide favorable visual outcome in tuberculum sellae meningiomas. Neurosurg Rev. 2012. 35: 601-7
5. Lee JH, Sade B, Park BJ. A surgical technique for the removal of clinoidal meningiomas. Neurosurgery. 2006. 59: 108-14
6. Mariniello G, Bonavolonta G, Tranfa F, Maiuri F. Management of the optic canal invasion and visual outcome in spheno-orbital meningiomas. Clin Neurol Neurosurg. 2013. 115: 1615-20
7. Mariniello G, de Divitiis O, Bonavolonta G, Maiuri F. Surgical unroofing of the optic canal and visual outcome in basal meningiomas. Acta Neurochir. 2013. 155: 77-84
8. Nozaki K, Kikuta K, Takagi Y, Mineharu Y, Takahashi JA, Hashimoto N. Effect of early canal unroofing on the outcome of visual functions in surgery for meningiomas of the tuberculum sellae and planum sphenoidale. Neurosurgery. 2008. 62: 839-44
9. Schick U, Hassler W. Surgical management of tuberculum sellae meningiomas: Involvement of the optic canal and visual outcome. J Neurol Neurosurg Psychiatry. 2005. 76: 977-83
10. Seol HJ, Park HY, Nam DH, Kong DS, Lee JI, Kim JH. Clinical outcomes of tuberculum sellae meningiomas focusing on reversibility of postoperative visual function. Acta Neurochir. 2013. 155: 25-31
11. Tobias S, Kim CH, Kosmorsky G, Lee JH. Management of surgical clinoidal meningiomas. Neurosurg Focus. 2003. 14: e5-
12. Wang CW, Li YY, Zhu SG, Yang Y, Wang HW, Gong J. Surgical management and evaluation of prognostic factors influence postoperative visual outcome of suprasellar meningiomas. World Neurosurg. 2011. 75: 294-302
13. Yonekawa Y, Ogata N, Imhof H, Olivecrona M, Strommer K, Kwak T. Selective extradural anterior clinoidectomy for supra- and parasellar processes. J Neurosurg. 1997. 87: 636-42