- Department of Neurosurgery, Hospital Getulio Vargas, Recife, Pernambuco, Brazil.
- Department of Neurosurgery, Universidade Federal do Vale do São Francisco, Petrolina, Pernambuco, Brazil.
- Department of Neurosurgery, Rede D’Or Sao Luiz, Recife, Pernambuco, Brazil.
DOI:10.25259/SNI_284_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Claudio Henrique F. Vidal1, Ricardo Brandao Fonseca2, Bruno Leimig1, Walter F. Matias-Filho3, Geraldo Sa Carneiro-Filho3. Increase of the clivus-canal angle in patients with basilar invagination, without atlantoaxial displacement, treated with a simple maneuver of indirect decompression of the odontoid with the head clamp, during posterior occipitocervical arthrodesis. 07-Jun-2021;12:260
How to cite this URL: Claudio Henrique F. Vidal1, Ricardo Brandao Fonseca2, Bruno Leimig1, Walter F. Matias-Filho3, Geraldo Sa Carneiro-Filho3. Increase of the clivus-canal angle in patients with basilar invagination, without atlantoaxial displacement, treated with a simple maneuver of indirect decompression of the odontoid with the head clamp, during posterior occipitocervical arthrodesis. 07-Jun-2021;12:260. Available from: https://surgicalneurologyint.com/surgicalint-articles/10867/
Abstract
Background: Basilar invagination (BI) can be defined as the insinuation of the content of the craniovertebral junction through the foramen magnum toward the posterior fossa. BI is a prevalent condition in Northeast Brazil. The present study describes the changes in the clivus-canal angle (CCA) in the postoperative period in patients with symptomatic BI operated by a posterior approach, using a simple technique of indirect reduction of the odontoid associated with occipitocervical fixation.
Methods: Patients underwent radiological evaluations by magnetic resonance imaging in the pre and postoperative periods, where the height of the odontoid tip was measured in relation to the Chamberlain line and the ACC. All patients underwent posterior occipitocervical fixation with specific maneuvers of distraction and extension of the cephalic segment with the aid of a head clamp with three fixation points for anterior reduction of the odontoid.
Results: Among the 8 patients evaluated in the series, all had increased ACC in the postoperative period, with a mean of 14.81 ± 1.54°, and statistically significant difference between the pre and postoperative periods (P
Conclusion: The indirect surgical reduction of the odontoid process by a posterior approach through the manipulation (distraction-extension) of a “Mayfield” type of head clamp followed by occipitocervical fixation proved to be effective in improving the ACC, being easily reproducible.
Keywords: Arnold Chiari malformation, Foramen magnum, Odontoid process, Skull base, Sphenoid bone
INTRODUCTION
Basilar invagination (BI) is part of a larger spectrum of malformations in the development of the craniovertebral junction (CJV) and can be defined as the insinuation of the content of the CJV through the foramen magnum toward the posterior fossa.[
Symptomatic BI is usually a progressively debilitating condition and its failure to be recognized and treated can predispose patients to develop disabling neurological deficits that can proceed until death.[
In the present study, the authors describe the changes in the clivus-canal angle (CCA) in patients with “Goel type B” BI, after the application of a simple surgical maneuver to reduce indirectly the odontoid peg, by a posterior approach alone, with the user of a Mayfield head clamp and a posterior occipitocervical fixation (POCF).
MATERIALS AND METHODS
Patients
The local review board approved the study protocol (CAAE-77722017.7.00005200) and all patients gave written consent for data analysis. The study was a retrospective review of medical records of patients with symptomatic BI, with surgical indication, and who underwent the technique under analysis between 2015 and 2017, in a single institution and with the same surgeon (CV).
The inclusion criteria were as follow: (a) primary BI; (b) symptoms and signs compatible with compression at the foramen magnum such as: ataxias, pyramidal, sensitive, and lower cranial nerve dysfunctions; and (c) tip of the odontoid process 5 mm above in relation to the Chamberlain’s line during magnetic resonance imaging (MRI) evaluation.
The following exclusion criteria were adopted: (a) patients not submitted to POCF; (b) patients previously submitted to odontoidectomy or posterior fossa bone decompression; (c) injuries to CVJ secondary to trauma, neoplasia, or inflammatory diseases; and (d) unavailability of imaging exams in the pre or postoperative periods.
Procedures
Surgical technique
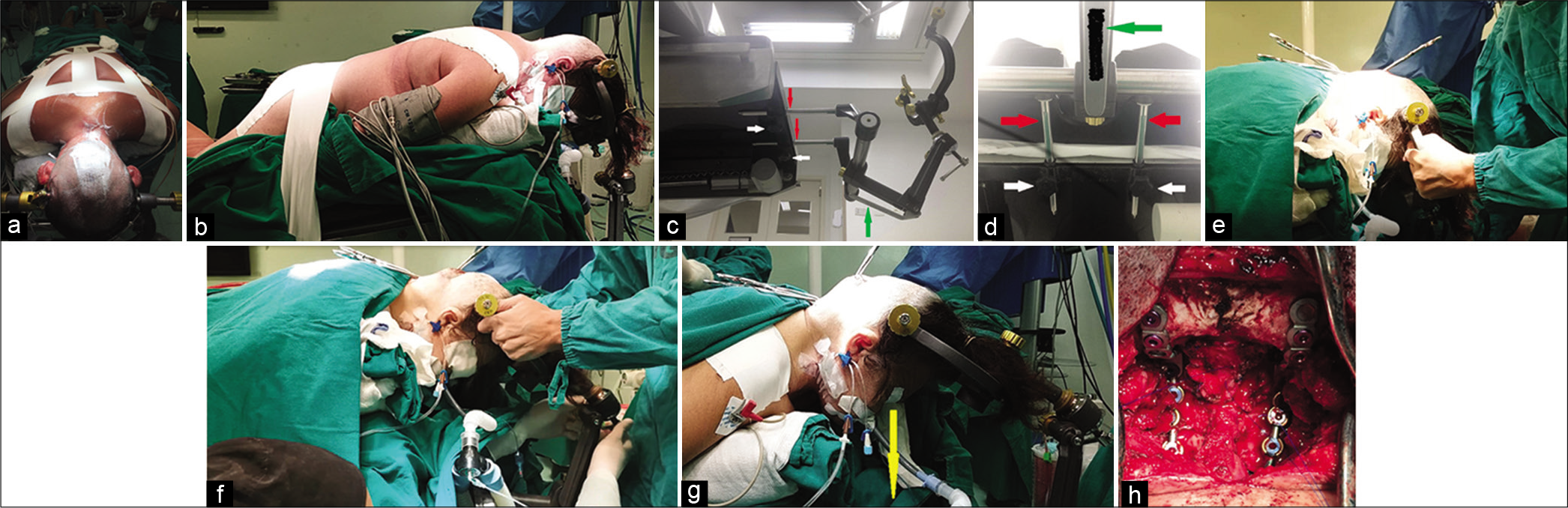
After anesthetic induction, the “Mayfield” head clamp (HeadFix® Micromar, São Paulo) is installed with the three pins, which should be in the same axial plane at the level of the parietal eminences and upper temporal line. Afterward, the patient is placed in prone position. It is extremely important to ensure that the patient’s trunk is fixed to the operating table with strips of adhesive tape [
Figure 1:
Patient positioning and sequence of movements with emphasis on structures of the operating table and head clamp (“Mayfield” type) that are manipulated during transoperative distraction-extension maneuver of the CVJ in patients with BI of type B of Goel. (a) The patient’s trunk is fixed to the operating table with adhesive tapes. Cranial fixation with Mayfield type head clamp, with the 3 fixation points which should be in the same axial plane at the level of the parietal eminences and upper temporal line. At this moment, the cephalic segment is in slight flexion in order to make the planes more superficial (in BI the CVJ is deeper than usual), facilitating the osteodural decompression performed initially. (b) Lateral view of another patient, where can be observed: fixation to the table of the pelvic girdle and trunk with adhesive tapes; head is positioned, above the heart, with slight flexion to facilitate CVJ bone decompression; head clamp with 3 pins in the same axial plane (parietal eminences and upper temporal line). (c and d) Inferolateral and inferior view, respectively, of the Mayfield head clamp attached to the operating table, where the components handled in the CVJ distraction-extension maneuver during POCF are observed: lock screws (white arrows); sliding metallic fitting on the table rails (red arrows); lever (green arrow). (e) Transoperative aspect of the distraction-extension maneuver. The surgeon stands in front of the patient’s head while the assistant (not shown) loosened the screw on the head clamp’s rails and unlocked the Mayfield lever. Horizontal CVJ was perceived due to the positioning of the head in semi-flexion. (f) The distraction-extension maneuvers of the CVJ were then applied to the cranial fixator, allowing the displacement of the device along the tracks of the operating table. The surgeon mobilized the patient’s head back and up, observing the clear reduction in the posterior CVJ space. The assistant’s gloved right hand is seen in the lower portion of the figure. (g) The position was considered appropriate when the patient’s line of sight was in a plane perpendicular to the floor (yellow arrow). After that, the assistant locked the head clamp in reverse order. The proximity of the surgical clamps inserted in the wound is perceived in relation to the images that precede the application of the maneuver. (h) Final view of the procedure, where a rod-plate POCF system was inserted bilaterally, after its manual molding in the CVJ region. The system was blocked with the use of locking caps in the subaxial region (lateral mass screws were inserted bilaterally at the beginning of the procedure) and bicortical screws in the occipital bone. The central portion of the surgical field demonstrates the craniectomy of the occipital bone with the opening of the foramen magnum and removal of the posterior arch of C1. The dura mater of the CVJ was also opened and expanded with an autologous pericranium graft. Note the extreme impaction of the first subaxial screws at the base of the skull. BI: Basilar invagination, CVJ: Craniovertebral junction, POCF: Posterior occipitocervical fixation.
After skin incision and dissection through the midline avascular planes, the posterior bone elements of the occipital bone, CVJ, and subaxial spine are exposed. In this study, all patients were submitted to craniectomy of the occipital bone with the opening of the foramen magnum and removal of the posterior arch of C1. The dura mater of the CVJ was also opened and expanded with an autologous pericranium graft. No patient underwent aspiration or resection of the cerebellar tonsils.
Lateral mass screw was positioned bilaterally, including levels C3, C4, and C5, using the Roy-Camille technique. The deformity associated with BI in this series was so pronounced that the insertion of screws at levels C1 and C2 was not possible due to the impaction at the skull base of these segments and the large associated anatomical variations.
The surgeon positioned himself in front of the patient’s head, and the assistant loosened the screw locks on the head clamp’s rails and unlocked the Mayfield lever [
A rod-plate POCF system was then inserted bilaterally, and after its manual molding in the CVJ region, the system was blocked with the use of locking caps in the subaxial region and bicortical screws in the occipital bone [
The procedure was completed by firstly closing the aponeurotic galea, then the subcutaneous and the skin, thereby reducing dead spaces and the formation of collections. No drain was used.
Radiological evaluation
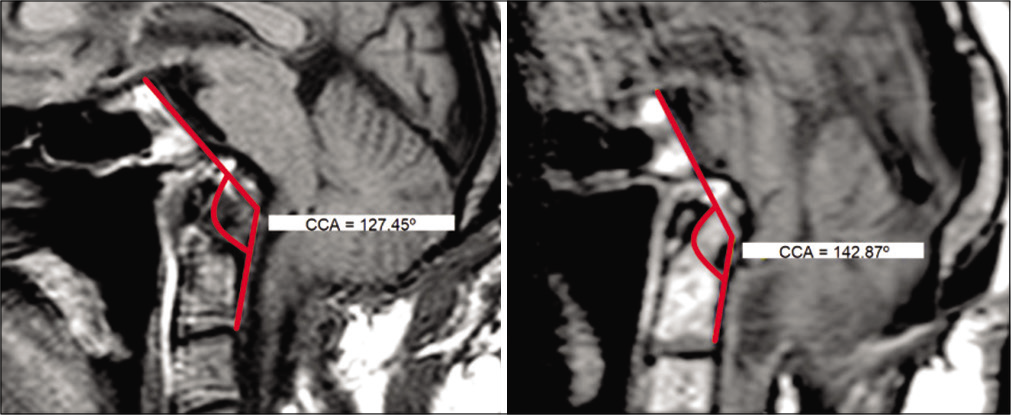
All patients underwent an MRI in the pre and postoperative periods using a 1.5 Tesla scanner (Intera, Philips Medical Systems, Best, The Netherlands). The odontoid height (OH), in centimeters, was defined by the height of the odontoid tip in relation to the Chamberlain line. It was calculated in all patients only in the preoperative period, as the patients underwent suboccipital craniectomy. The clivus-canal angle (CCA) was measured, in degrees, using median sagittal slices in the T1 sequence, and compared in the pre and postoperative periods. The CCA was obtained by measuring the angle between drawn lines tangent to posterior surfaces of the clivus and odontoid process, respectively [
Figure 2:
Measurement of CCA in the preoperative (left, 127°) and postoperative (right, 142°) periods in the T1 sagittal MRI sequence. The CCA was obtained by measuring the angle between drawn lines tangent to posterior surfaces of the clivus and odontoid process, respectively. CCA: Clivus-canal angle, MRI: Magnetic resonance imaging.
Statistical analysis
All data were stored on an Excel 2010 worksheet and statistical calculations were performed on PRISM®, version 6 for Windows (GraphPad Software Incorporated). The data were presented in terms of absolute and percentage values and measures of descriptive statistics such as: mean, standard deviation, minimum, and maximum values. For comparison between the pre and postoperative periods, the paired t-test was used. The margin of error adopted was 5.0%.
RESULTS
Initially, data from 22 patients with CVJ diseases operated on by one of the authors (CV) was collected at a single institution between March 2015 and July 2017. Of these, 14 patients were excluded from the study, 9 for not having undergone to POCF, and 5 for not having sufficient radiological data, leaving only 8 patients for analysis.
In relation to sex, five patients (62.5%) were women and three (37.5%) were men. The minimum age was 33 years and the maximum 68 years, with a mean of 49.25 ± 11.29 years. All patients in the study had associated Chiari type 1 malformation.
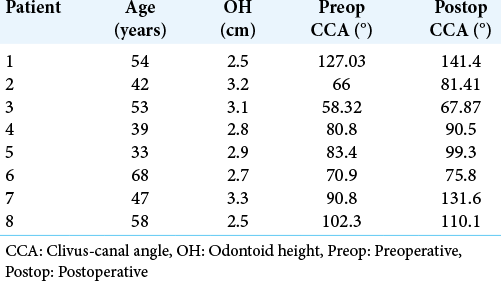
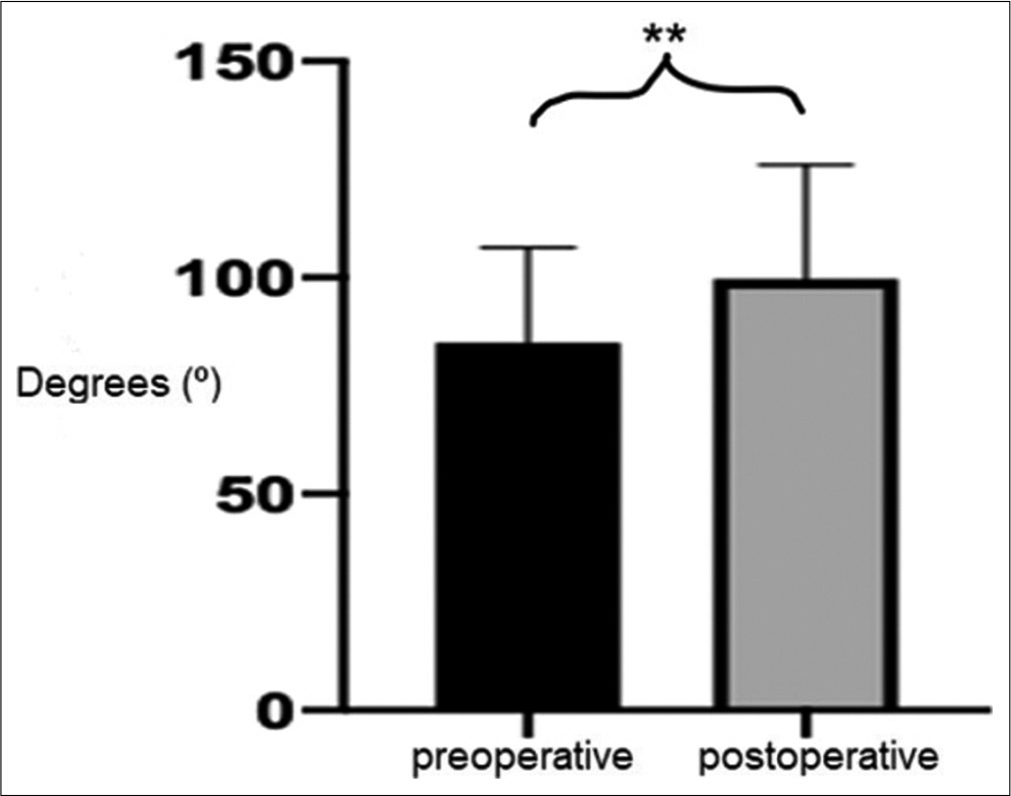
The mean of OH was 2.87 ± 0.3 cm. The minimum and maximum values were 2.5 and 3.3 cm, respectively. The CCA in the preoperative period varied between 66 and 100.7°, with a mean of 83.6 ± 13.1° [
The CCA in the postoperative period varied between 67.87 and 142.4°, with a mean of 99.75 ± 26.37° [
In all patients, an increase in CCA was observed in the postoperative period. The mean of this increase was 14.81 ± 1.54°, ranging from 4.9 to 40.8°. There was a statistically significant difference between the pre and postoperative periods in relation to CCA (P = 0.0073, paired t-test).
Surgical postoperative complications that required active interventions occurred in two (25%) patients. One patient developed cerebrospinal fluid leakage on the fifth postoperative day, requiring a new surgical intervention for dural graft suture. Another patient developed meningitis in the postoperative period and was treated with a broad-spectrum antibiotic regimen for 14 days. Both had no additional sequelae. Two patients still had transient horizontal nystagmus, observed only in the first 48 h of the postoperative period. There were no deaths.
DISCUSSION
BI is a prevalent condition in the Northeast of Brazil, associated with other craniometric changes such as platybasia and brachycephaly.[
Goel proposed that type B patients of his classification should be submitted to posterior decompression of the foramen magnum as a fundamental step in their treatment.[
Of the anterior decompression techniques, the transoral approach to removing the odontoid peg was the classic route until recently.[
Since its anatomical description in 2002,[
Endonasal endoscopic odontoidectomy requires high expertise from the surgeon, as the working distance is quite long, especially in retroverted odontoids, and it is difficult to do it in obese patients and in the presence of associated subaxial deformities of the cervical spine.[
The indirect reduction of the odontoid by the application of trans-skeletal external traction or by intraoperative maneuvers during POCF has been used in patients with associated AAD (Goel Type A), even in cases considered irreducible, thus eliminating the need for ventral approach to remove the odontoid peg.[
Kim et al. in 2004[
In the region of the current study, these patients with BI of Type B of Goel have an eversion into the posterior fossa of the constituent components of the margins of the foramen magnum. The deformity goes far beyond the simple insinuation of the odontoid through the foramen magnum. It is probable that fixation restricted to segments C1 and C2 is not able to reverse, even partially, the complex deformities present in these patients that include the clivus and occipital bone (personal communication).
The technique discussed here is simple and highly reproducible in any neurosurgery service without requiring major technological resources, except for a 3-point “Mayfield” type head clamp. All patients submitted to the present technique showed an increase in the CCA, a mean of 14.81 ± 1.54°, with a statistically significant difference between the pre and postoperative periods, as described by Kim et al. in children.[
The present manuscript is intended to describe a suitable technique for treating patients with BI of the “type B” of Goel associated with pronounced CVJ deformities, usually found in the study region. The lack of clinical outcomes analysis should be the focus of forthcoming analyses. Although not the subject of the present study, none of the patients required posterior decompression at a later stage. There was an appreciable neurological improvement in all patients. The rate of complications was low and manageable.
Probably, ventral approaches for removing the odontoid peg will remain only as a rescue procedure in patients who underwent an attempt to indirect posterior decompression and who did not obtain a satisfactory clinical response associated with radiological evaluation showing persistence of brainstem compression.[
There were many limitations to this study, particularly the small number of patients and the lack of clinical data, especially for long-term follow-up. Since it was carried out in a public health system hospital in one of the poorest regions of Brazil (Northeast), there was no access to technologies such as intraoperative neurophysiological monitoring and transoperative image acquisition system and navigation, which have been shown to be beneficial.[
CONCLUSION
The indirect decompression of the brainstem by the odontoid peg during POCF, using distraction-extension maneuvers of the cephalic segment with the aid of the “Mayfield” head clamp in patients with BI of type B of Goel, seems to be a promising technique in this complex group of patients with multiple CVJ malformations. It has the advantage of single approach reduction and fixation, decreasing surgical morbidity. All patients in this series showed radiological improvement of the CCA and associated neurological improvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alfieri A, Jho HD, Tschabitscher M. Endoscopic endonasal approach to the ventral cranio-cervical junction: Anatomical study. Acta Neurochir (Wien). 2002. 144: 219-25
2. Botelho RV, Ferreira ED. Angular craniometry in craniocervical junction malformation. Neurosurg Rev. 2013. 36: 603-10
3. Caetano de Barros M, Farias W, Ataíde L, Lins S. Basilar impression and Arnold-Chiari malformation. A study of 66 cases. J Neurol Neurosurg Psychiatry. 1968. 31: 596-605
4. Caird J, Bolger C. Preoperative cervical traction in cases of cranial settling with halo ring and Mayfield skull clamp. Br J Neurosurg. 2005. 19: 488-9
5. Chamberlain WE. Basilar impression (platybasia): A bizarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Yale J Biol Med. 1939. 11: 487-96
6. Chandra PS, Kumar A, Chauhan A, Ansari A, Mishra NK, Sharma BS. Distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation: A novel pilot technique. Neurosurgery. 2013. 72: 1040-53
7. Chopra JS, Sawhney IM, Kak VK, Khosla VK. Craniovertebral anomalies: A study of 82 cases. Br J Neurosurg. 1988. 2: 455-64
8. Crockard HA, Pozo JL, Ransford AO, Stevens JM, Kendall BE, Essigman WK. Transoral decompression and posterior fusion for rheumatoid atlanto-axial subluxation. J Bone Joint Surg Ser B. 1986. 68: 350-6
9. da Silva JA, Brito JC, da Nóbrega PV, Costa MD, de Souza AB. Surgical findings in 260 cases of basilar impression and/ or Arnold-Chiari malformation. Arq Neuropsiquiatr. 1994. 52: 363-9
10. da Silva JA, de Almeida Holanda MM. Basilar impression, chiari malformation and syringomyelia: A retrospective study of 53 surgically treated patients. Arq Neuropsiquiatr. 2003. 61: 368-75
11. da Silva JA.editors. Impressão Basilar. Malformações Occipitocervicais. Recife, PE: Editora Universitária UFPE; 2003. p. 169-300
12. Di Lorenzo N, Fortuna A, Guidetti B. Craniovertebral junction malformations. Clinicoradiological findings, long-term results, and surgical indications in 63 cases. J Neurosurg. 1982. 57: 603-8
13. Dickman CA, Locantro J, Fessler RG. The influence of transoral odontoid resection on stability of the craniovertebral junction. J Neurosurg. 1992. 77: 525-30
14. Dlouhy BJ, Dahdaleh NS, Menezes AH. Evolution of transoral approaches, endoscopic endonasal approaches, and reduction strategies for treatment of craniovertebral junction pathology: A treatment algorithm update. Neurosurg Focus. 2015. 38: 1-16
15. El-Sayed IH, Wu JC, Dhillon N, Ames CP, Mummaneni P. The importance of platybasia and the palatine line in patient selection for endonasal surgery of the craniocervical junction: A radiographic study of 12 patients. World Neurosurg. 2011. 76: 183-8
16. Erbengi A, Öge HK. Congenital malformations of the craniovertebral junction: Classification and surgical treatment. Acta Neurochir (Wien). 1994. 127: 180-5
17. Ferreira JA, Botelho R V. The odontoid process invagination in normal subjects, Chiari malformation and Basilar invagination patients: Pathophysiologic correlations with angular craniometry. Surg Neurol Int. 2015. 6: 118
18. Frade HC, França CC, do Nascimento JJ, de Almeida Holanda MM, da Silva Neto EJ, Araújo Neto SA. Craniovertebral transition assessment by magnetic resonance imaging in a sample of a northeast Brazilian population. Arq Neuropsiquiatr. 2017. 75: 419-23
19. Gladi M, Iacoangeli M, Specchia N, Re M, Dobran M, Alvaro L. Endoscopic transnasal odontoid resection to decompress the bulbo-medullary junction: A reliable anterior minimally invasive technique without posterior fusion. Eur Spine J. 2012. 21: S55-60
20. Goel A, Sathe P, Shah A. Atlantoaxial fixation for basilar invagination without obvious atlantoaxial instability (group b basilar invagination): Outcome analysis of 63 surgically treated cases. World Neurosurg. 2017. 99: 164-70
21. Goel A. Basilar invagination, chiari malformation, syringomyelia: A review. Neurol India. 2009. 57: 235-46
22. Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004. 1: 281-6
23. Guppy KH, Chakrabarti I, Banerjee A. The use of intraoperative navigation for complex upper cervical spine surgery. Neurosurg Focus. 2014. 36: E5
24. Hadley MN, Spetzler RF, Sonntag VK. The transoral approach to the superior cervical spine. A review of 53 cases of extradural cervicomedullary compression. J Neurosurg. 1989. 71: 16-23
25. Kassam AB, Snyderman C, Gardner P, Carrau R, Spiro R, Sonntag VK. The expanded endonasal approach: A fully endoscopic transnasal approach and resection of the odontoid process: Technical case report. Neurosurgery. 2005. 57: E213
26. Kim LJ, Rekate HL, Klopfenstein JD, Sonntag VK. Treatment of basilar invagination associated with chiari I malformations in the pediatric population: Cervical reduction and posterior occipitocervical fusion. J Neurosurg. 2004. 101: 189-95
27. Landeiro JA, Boechat S, Christoph DD, Gonçalves MB, de Castro I, Lapenta MA. Transoral approach to the craniovertebral junction. Arq Neuropsiquiatr. 2007. 65: 1166-71
28. Levy WJ, Mason L, Hahn JF. Chiari malformation presenting in adults: A surgical experience in 127 cases. Neurosurgery. 1983. 12: 377-90
29. Menezes AH, VanGilder JC. Transoral-transpharyngeal approach to the anterior craniocervical junction. Ten-year experience with 72 patients. J Neurosurg. 1988. 69: 895-903
30. Menezes AH. Anterior approaches to the craniocervical junction. Clin Neurosurg. 1991. 37: 756-69
31. Menezes AH. Surgical approaches: Postoperative care and complications transoral-transpalatopharyngeal approach to the craniocervical junction. Childs Nerv Syst. 2008. 24: 1187-93
32. Morales-Valero SF, Serchi E, Zoli M, Mazzatenta D, Van Gompel JJ. Endoscopic endonasal approach for craniovertebral junction pathology: A review of the literature. Neurosurg Focus. 2015. 38: E5
33. Nascimento JJ, Carreiro NM, Oliveira GT, Ribeiro EC, Holanda MM, Neto EJ. Relationship between basilar invagination and brachycephaly in Northeastern Brazil. Eur J Radiol. 2018. 104: 58-63
34. Salunke P, Sahoo S, Khandelwal NK, Ghuman MS. Technique for direct posterior reduction in irreducible atlantoaxial dislocation: Multi-planar realignment of C1-2. Clin Neurol Neurosurg. 2015. 131: 47-53
35. Shriver MF, Kshettry VR, Sindwani R, Woodard T, Benzel EC, Recinos PF. Transoral and transnasal odontoidectomy complications: A systematic review and meta-analysis. Clin Neurol Neurosurg. 2016. 148: 121-9
36. Smith JS, Shaffrey CI, Abel MF, Menezes AH. Basilar invagination. Neurosurgery. 2010. 66: 39-47
37. Tong HY, Qiao GY, Zhao B, Yin YH, Li T, Yu XG. Can posterior reduction replace odontoidectomy as treatment for patients with congenital posterior atlantoaxial dislocation and basilar invagination?. Oper Neurosurg. 2020. 18: 660-7
38. Vidal CH, Brainer-Lima AM, Valença MM, de Lucena Farias R. Chiari 1 malformation surgery: Comparing non-violation of the arachnoid versus arachnoid opening and thermocoagulation of the tonsils. World Neurosurg. 2019. 121: e605-13
39. Vidal CH, da Silva JC, Pacheco Lins CJ, Brainer-Lima AM, Moraes Valença M. Craniovertebral junction malformation in Northeastern Brazil: The myth of the Dutch colonization. Arq Neuropsiquiatr. 2013. 71: 405-7
40. Vidal CH. In reply to do we need to perform duroplasty and tonsillar resection in the surgical treatment for patients with chiari 1 malformation?. World Neurosurg. 2019. 125: 538
41. Vidal CH. Surgical treatment of Type I chiari malformation: The role of Magendie’s foramen opening e tonsils manipulation. Arq Neuropsiquiatr. 2015. 73: 179
42. Yu X, Li L, Wang P, Yin Y, Bu B, Zhou D. Intraoperative computed tomography with an integrated navigation system in stabilization surgery for complex craniovertebral junction malformation. J Spinal Disord Tech. 2014. 27: 245-52
43. Zileli M, Çagli S. Combined anterior and posterior approach for managing basilar invagination associated with Type I chiari malformation. J Spinal Disord Tech. 2002. 15: 284-9