- Department of Neurosurgery, Hospital General de la Plaza de la Salud, Santo Domingo, Dominican Republic.
- Department of Research, Hospital General de la Plaza de la Salud, Santo Domingo, Dominican Republic.
- Department of Nephrology, Hospital General de la Plaza de la Salud, Santo Domingo, Dominican Republic.
Correspondence Address:
Jesús Antonio Echavarría-Uceta, Department of Research, Hospital General de la Plaza de la Salud, Santo Domingo, Dominican Republic.
DOI:10.25259/SNI_821_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lloyd R. Cassó-Troche1, Jesús Antonio Echavarría-Uceta2, Joan Quiñones-Robles1, Caran Haché-Pagan2, Ironelis Herrera1, Johnson Encarnación1, Silvestre De la Rosa1, Dolores Mejía De la Cruz2, Limber Rojas3, Pedro Pablo Díaz Vásquez1. Infective spondylodiscitis in hemodialysis patients. 25-Nov-2022;13:549
How to cite this URL: Lloyd R. Cassó-Troche1, Jesús Antonio Echavarría-Uceta2, Joan Quiñones-Robles1, Caran Haché-Pagan2, Ironelis Herrera1, Johnson Encarnación1, Silvestre De la Rosa1, Dolores Mejía De la Cruz2, Limber Rojas3, Pedro Pablo Díaz Vásquez1. Infective spondylodiscitis in hemodialysis patients. 25-Nov-2022;13:549. Available from: https://surgicalneurologyint.com/surgicalint-articles/12025/
Abstract
Background: Spondylodiscitis is a potentially catastrophic complication in patients on hemodialysis. It is slow and insidious onset and nonspecific symptoms have contributed to the late detection of this infectious process. Here, we reviewed the clinical characteristics and outcomes for patients on hemodialysis who developed spondylodiscitis who were diagnosed with spondylodiscitis.
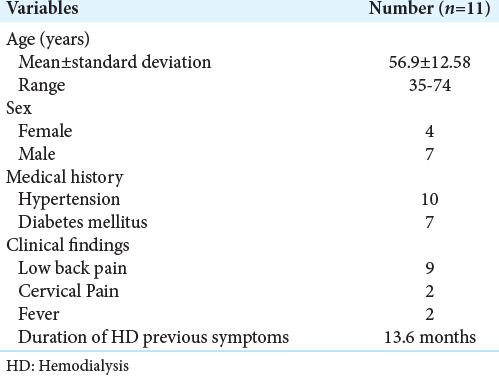
Methods: From 2011 to 2021, 11 (0.4%) of 2557 patients on hemodialysis were diagnosed with spondylodiscitis based on clinical symptoms, patients averaged 56.9 years of age, seven were male, and they presented with fever in just two cases. The most frequent comorbidities included hypertension (ten patients) and diabetes mellitus (seven patients). Here, we reviewed the clinical, radiological (i.e., MR scans), laboratory markers, and treatment choices (i.e., nonsurgical vs. surgical) for these 11 hemodialysis patients.
Results: Ten of the 11 patients underwent spinal surgery, and five were later readmitted for recurrent of infections. There was just one nonsurgical mortality.
Conclusion: For patients on hemodialysis, the new-onset of spinal pain may signal the onset of spondylodiscitis which should be rapidly diagnosed with MR studies and managed in a timely fashion either with antibiotic therapy and/or with surgery/antibiotics.
Keywords: Chronic kidney disease, End-stage renal disease, Hemodialysis, Neurosurgery, Spondylodiscitis
INTRODUCTION
Although the survival of patients with end-stage renal disease on hemodialysis has increased, the mortality rate for those developing bacteremia/sepsis remains high at 9.7% (i.e., due to repeated vascular access, iatrogenic immunosuppression, and urinary tract infections).[
MATERIALS AND METHODS
Spondylodiscitis was diagnosed for 11 (0.4%) of 2557 hemodialysis patients seen over a 10-year period (2011–2021).
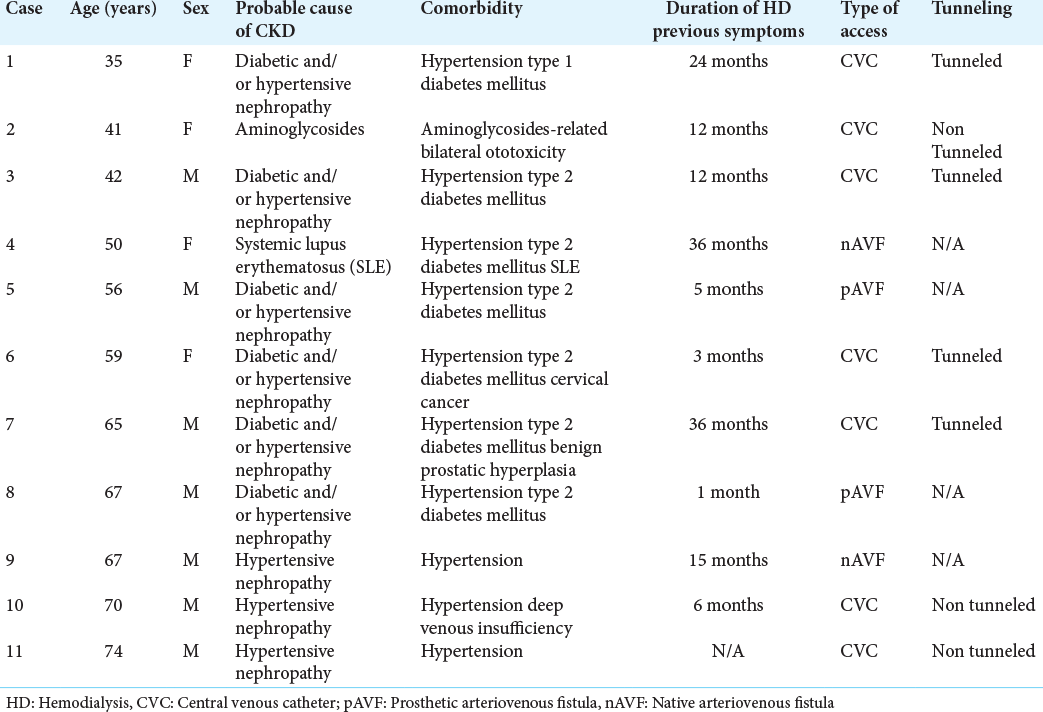
The mean duration of hemodialysis before the onset of this infection was 13.6 months. Patients averaged 56.9 years of age; seven were male. The most frequent comorbidities included hypertension (ten patients) and diabetes mellitus (seven patients). Their most frequent clinical findings included; low back pain (nine patients), cervical pain (two patients), and fever (two patients). Seven had central venous catheters, while prosthetic arteriovenous fistulas were present in two patients, and two others had native arteriovenous fistulas [
RESULTS
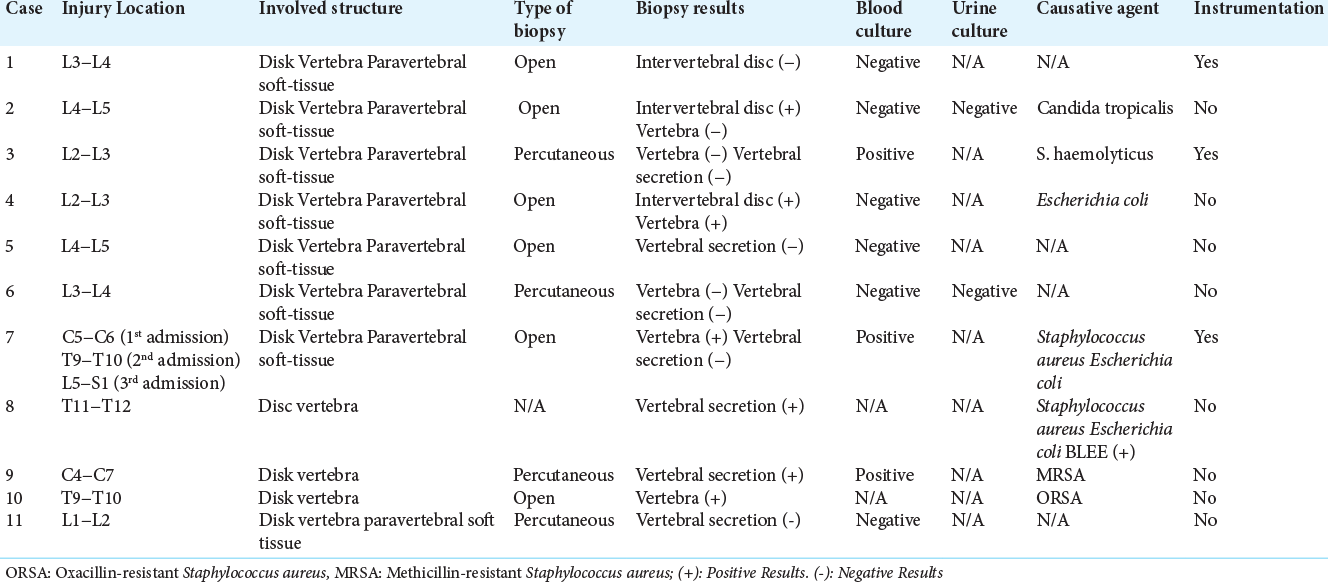
Surgery
Ten patients required surgery; six had an open biopsy (i.e., three required instrumentation), and four had percutaneous biopsies. Readmission due to recurrent infections occurred in five cases, with one patient requiring additional surgery (i.e., extension of arthrodesis). Notably, one nonsurgical patient died due to catheter-associated infection, leading to septic shock 15 months after diagnosis of spondylodiscitis.
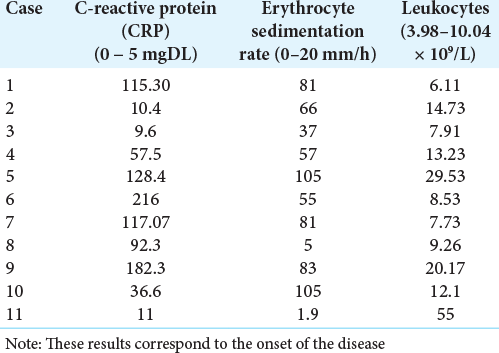
Infection Parameters
The most frequent pathogens were: Staphylococcus aureus (five patients), Escherichia coli (four patients), Candida tropicalis (one patient), and Staphylococcus haemolyticus (one patient [
DISCUSSION
Risk factors for patients with spondylodiscitis on hemodialysis include; uncontrolled diabetes mellitus, catheter-associated infections, infective endocarditis, previous spinal surgery, and immunosuppression. We had seven patients with diabetes and seven using central venous catheter for hemodialysis. Nine patients in our study presented low back pain, while hemodialysis patients with spondylodiskitis in general exhibit combinations of: spinal pain, general malaise, mild stiffness, nausea, and headaches (i.e., often due to water overload).[
Literature review
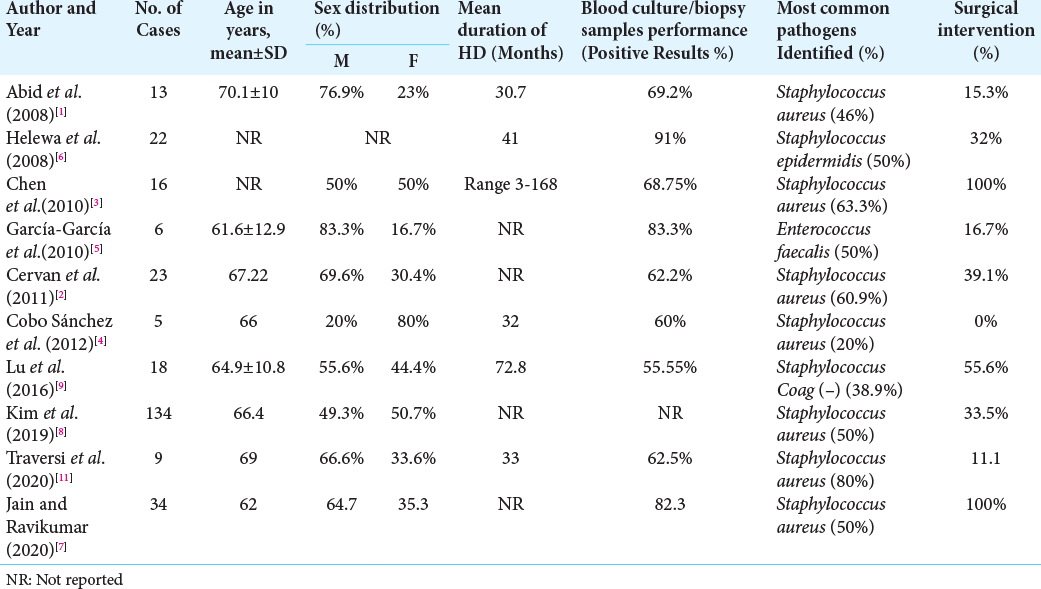
In the literature, infectious spondylodiscitis in hemodialysis patients involves the lumbar spine in from 58 to 68% of cases [
Surgery
Hemodialysis patients with spondylodiscitis often require percutaneous or open disk-vertebral biopsy to appropriately direct antibiotic therapy. We had better results obtaining diagnostic specimens through open biopsies. Surgical debridement may or may not require additional instrumentation for stability, but its’ use remains controversial due to the greater risk of recurrent infection[
CONCLUSION
For patients undergoing hemodialysis, it is critical to diagnose spondylodiscitis early (i.e., looking for the classical triad for of pain, fever, and neurological deficits) and optimally using enhanced MR scans to establish the diagnosis that can then direct optimal treatment (i.e., antibiotics alone vs. antibiotics with surgery).
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abid S, De Silva S, Warwicker P, Farrington K. Infective spondylodiscitis in patients on high-flux hemodialysis and online hemodiafiltration. Hemodial Int. 2008. 12: 463-70
2. Cervan AM, Colmenero JD, Del Arco A, Villanueva F, Guerado E. Spondylodiscitis in patients under haemodyalisis. Int Orthop. 2012. 36: 421-6
3. Chen LH, Fu TS, Kao YH, Tsai TT, Lai PL, Niu CC. Surgical treatment of infectious spondylitis in patients undergoing hemodialysis therapy. Eur Spine J. 2010. 19: 2223-8
4. Cobo Sánchez JL, Revuelta MG, Mantecón ME, Alonso RA, Cano MS. Infectious spondylodiscitis in patients with central venous catheters for haemodialysis: A retrospective study. J Ren Care. 2012. 38: 147-50
5. García-García P, Rivero A, del Castillo N, Jarque A, Getino MA, García-Pérez J. Infectious spondylodiscitis in hemodialysis: Infectious spondylodiscitis in hemodialysis. Semin Dial. 2010. 23: 619-26
6. Helewa RM, Embil JM, Boughen CG, Cheang M, Goytan M, Zacharias JM. Risk factors for infectious spondylodiscitis in patients receiving hemodialysis. Infect Control Hosp Epidemiol. 2008. 29: 567-71
7. Jain KV, Ravikumar TV. Surgical management of thoracolumbar spondylodiscitis in end-stage renal disease. Indian J Orthop. 2021. 55: 176-81
8. Kim J, Lee SY, Jung JH, Kim SW, Oh JK, Park MS. The outcome following spinal instrumentation in haemodialyzed patients with pyogenic spondylodiscitis. Bone Joint J. 2019. 101B: 75-82
9. Lu YA, Hsu HH, Kao HK, Lee CH, Lee SY, Chen GH. Infective spondylodiscitis in patients on maintenance hemodialysis: A case series. Ren Fail. 2017. 39: 179-86
10. Madhavan K, Chieng LO, Armstrong VL, Wang MY. Spondylodiscitis in end-stage renal disease: A systematic review. J Neurosurg Spine. 2019. 30: 1-9
11. Traversi L, Nava E, Xhaferi B, Bigatti GG, Tedoldi S, Mazzullo T. Spondylodiscitis in hemodialysis patients: A new emerging disease? Data from an Italian Center. G Ital Nefrol. 2020. 37: 2020-vol5