- Department of Neurosurgery, Kanazawa Medical Center, 1-1 Shimoishibikimachi, Kanazawa, Ishikawa, Japan.
DOI:10.25259/SNI_508_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yu Shimizu, Katsuhiro Tsuchiya, Norihiro Fujisawa. Intracerebral steal phenomenon induced focal reversible vasogenic edema and decrease in cerebral blood flow after carotid endarterectomy. 20-Jun-2020;11:161
How to cite this URL: Yu Shimizu, Katsuhiro Tsuchiya, Norihiro Fujisawa. Intracerebral steal phenomenon induced focal reversible vasogenic edema and decrease in cerebral blood flow after carotid endarterectomy. 20-Jun-2020;11:161. Available from: https://surgicalneurologyint.com/surgicalint-articles/10096/
Abstract
Background: Intracerebral steal phenomenon (ISP) is a rare complication following surgical treatment of carotid stenosis. However, the factors responsible remain unknown. We described the rear case of the ISP who had vasogenic edema and cerebral blood flow (CBF) decline and presented with hemiparesis after carotid endarterectomy (CEA).
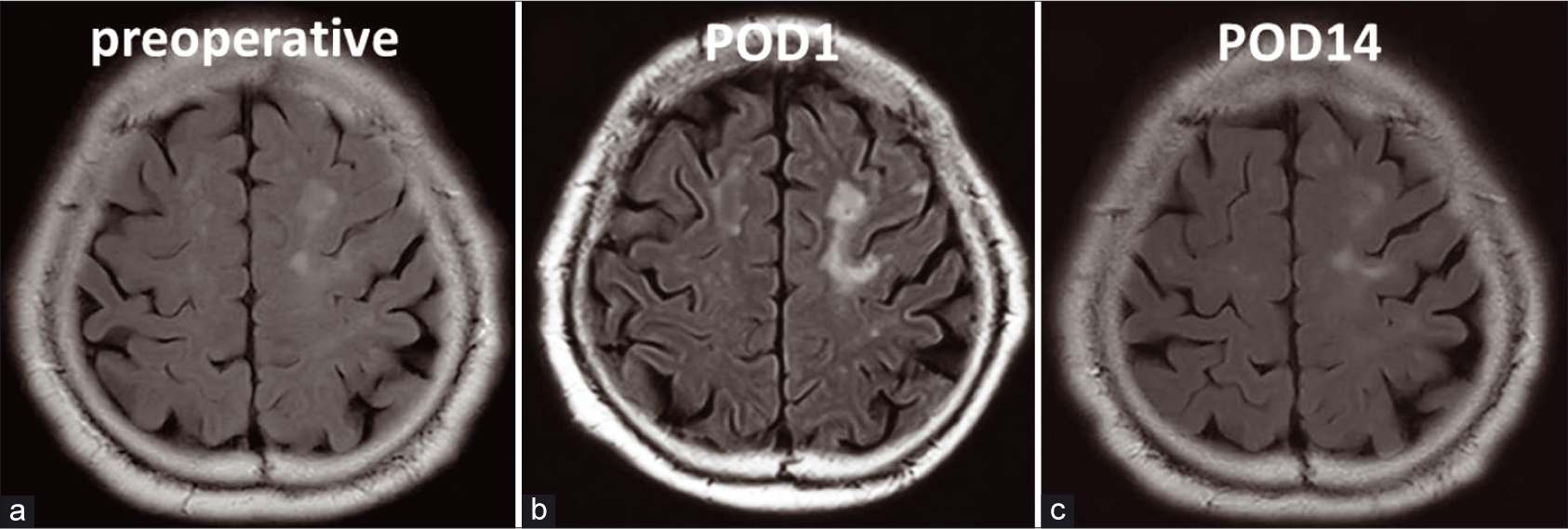
Case Description: A 72-year-old male with stenosis of the bilateral carotid artery (NASCET right 90% and left 70%) presented with cerebral hypoperfusion manifesting as right hemiparesis, after left CEA. Fluid-attenuated inversion recovery images showed edema of the motor area around an old infarction and a decrease in CBF. This lesion was an area of vasogenic edema caused by ISP and focal cerebral hypoperfusion. CBF of the contralateral cerebral hemispheres had increased. The treatment with an intravenous infusion of a free radical scavenger and glycerol improved the patient’s symptoms and brain edema. Magnetic resonance imaging showed a gradual decline in the brain edema, which completely disappeared 2 weeks after CEA. He was discharged with no neurological deficit.
Conclusion: In this report, we described the case of a patient with ISP who had vasogenic edema induced by CBF decline and presented with hemiparesis following CEA. This is the first report of progressing focal vasogenic edema caused by ISP after endarterectomy.
Keywords: Cerebral blood flow, Endarterectomy, Intracerebral steal phenomenon, Single-photon emission computed tomography, Vasogenic edema
INTRODUCTION
Intracerebral steal phenomenon (ISP) is a rare complication after the treatment of carotid artery stenosis. ISP after the stent is reported, but the ISP after the carotid endarterectomy (CEA) has not been reported yet.[
CASE PRESENTATION
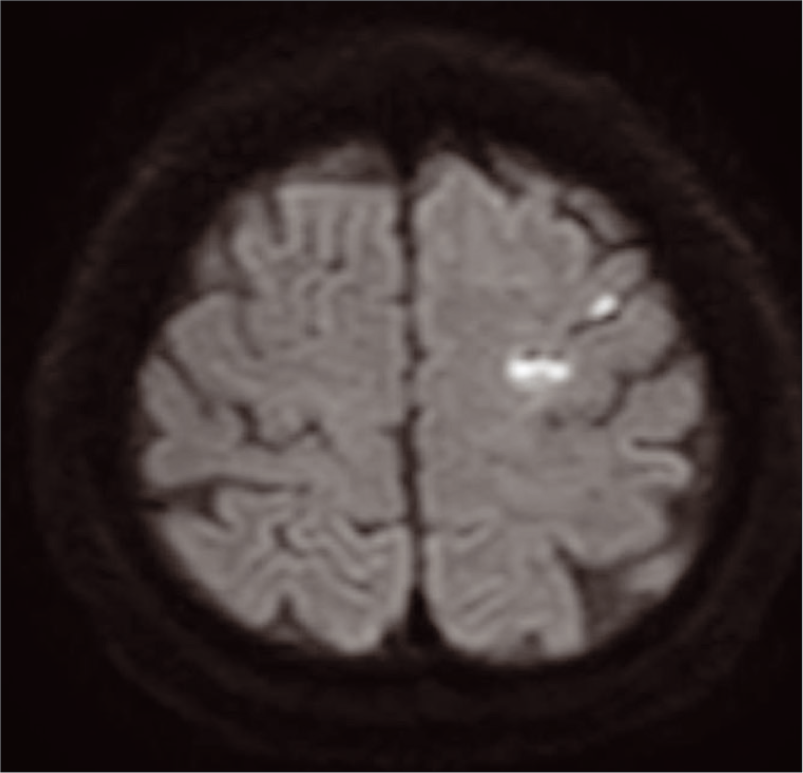
A 72-year-old male initially presented with the right-sided hemiparesis and underwent magnetic resonance (MR) imaging. MR imaging revealed acute infarction of the left frontal lobe [
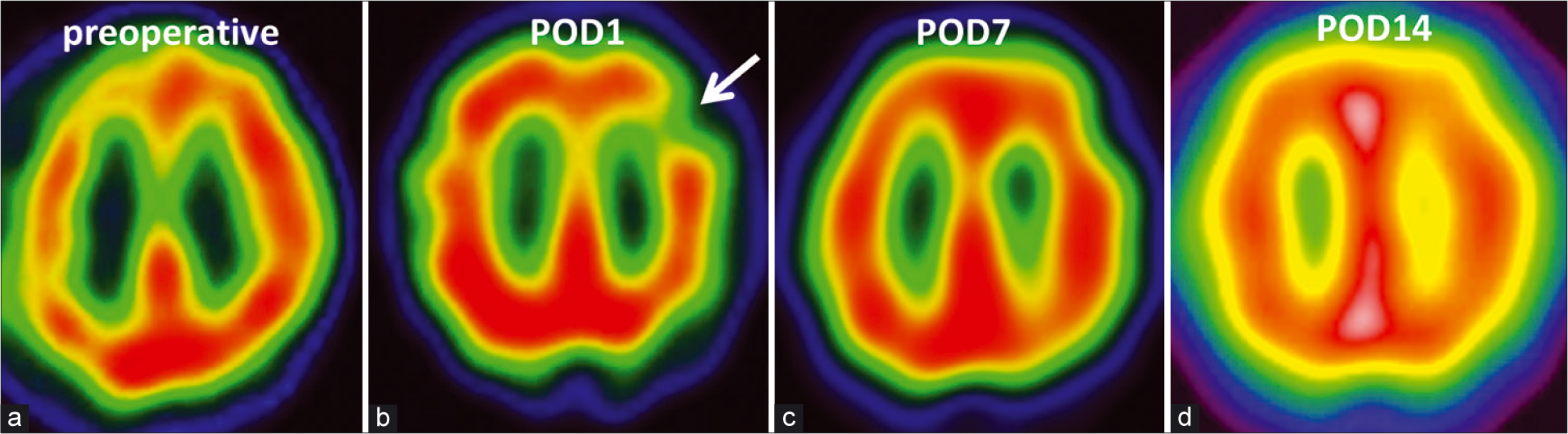
Figure 2:
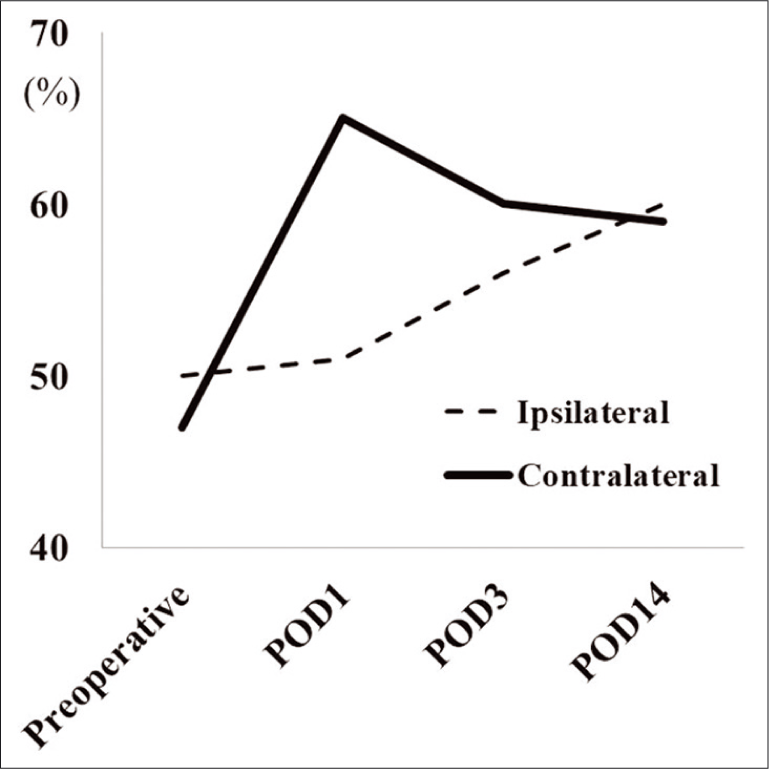
(a) Single-photon emission computed tomography (SPECT) revealing a significant decrease in cerebral blood flow (CBF) in the bilateral hemispheres, predominantly on the right side (CBF of middle cerebral artery area, R: 47 ml/100 g/min and L: 50 ml/100 g/min). (b) SPECT showing focal hypoperfusion (white arrow) around an old infarction (CBF of middle cerebral artery area, R: 65 ml/100 g/min and L: 51 ml/100 g/min). (c) SPECT demonstrating gradually normalized CBF in the lesion (CBF of middle cerebral artery area, R: 60 ml/100 g/min and L: 56 ml/100 g/min). (d) SPECT is demonstrating completely normalized CBF of the lesion (CBF of middle cerebral artery area, R: 59 ml/100 g/min, and L: 60 ml/100 g/min).
DISCUSSION
Following CEA, the previously reduced CBF due to stenosis or occlusion on the contralateral side increased.[
It was reported that communicating arteries caused contralateral CBF increase.[
Vasogenic edema occurs due to local cerebral hypoperfusion and subsequent dis-autoregulation/blood– brain barrier (BBB) disruption after revascularization.[
Sato et al. reported that cortical FLAIR high-intensity signs can be caused by postoperative hemodynamic conditions including hypoperfusion.[
To counteract these deleterious cascades, we used a free- radical scavenger in addition to glycerin in the present case. These postoperative treatments, which were intended to prevent symptomatic cerebral hypoperfusion, may play a role in avoiding further progression of the vasogenic edema. Our patient recovered completely 2 weeks after surgery.
CONCLUSION
ISP caused focal vasogenic edema and neurologic deficits in our patient, who had a prior infarction. MR imaging showed focal vasogenic edema around the old infarction, and SPECT revealed a decrease in focal CBF. Focal vasogenic edema was subsequently found to have occurred around the fragile vessels of the old infarction. After treating the edema and ischemia, the neurologic deficits were alleviated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. AY Lau, Wong EH, Wong A, Mok VC, Leung TW, Wong KS. Significance of good collateral compensation in symptomatic intracranial atherosclerosis. Cerebrovasc Dis. 2012. 33: 517-24
2. Baracchini C, Meneghetti G, Manara R, Ermani M, Ballotta E. Cerebral hemodynamics after contralateral carotid endarterectomy in patients with symptomatic and asymptomatic carotid occlusion: A 10-year follow-up. J Cereb Blood Flow Metab. 2006. 26: 899-905
3. Hamano E, Kataoka H, Morita N, Maruyama D, Satow T, Iihara K. Clinical implications of the cortical hyper intensity belt sign in fluid-attenuated inversion recovery images after bypass surgery for Moyamoya disease. J Neurosurg. 2017. 126: 1-7
4. Hashimoto N, Tominaga T, Miyamoto S, Nagata I, Houkin K, Suzuki N. Guidelines for diagnosis and treatment of Moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo). 2012. 52: 245-66
5. Kataoka T, Hyogo T, Hayase K, Nakamura H. Cerebral blood flow change before and after carotid angioplasty and stenting (CAS) in cases with contralateral carotid artery occlusion. Interv Neuroradiol. 2006. 12: 201-4
6. Lagrèze HL, Levine RL, Pedula KL, Nickles RJ, Sunderland JS, Rowe BR. Contralateral flow reduction in unilateral stroke: Evidence for transhemispheric diaschisis. Stroke. 1987. 18: 882-6
7. Oka F, Ishihara H, Kato S, Higashi M, Suzuki M. Cerebral hemodynamic benefits after contralateral carotid artery stenting in patients with internal carotid artery occlusion. AJNR Am J Neuroradiol. 2013. 34: 616-21
8. Sadato A, Maeda S, Hayakawa M, Adachi K, Toyama H, Nakahara I. Carotid stenting for unilateral stenosis can increase contralateral hemispheric cerebral blood flow. J Neurointerv Surg. 2018. 10: 351-4
9. Sato Y, Ito K, Ogasawara K, Sasaki M, Kudo K, Murakami T. Postoperative increase in cerebral white matter fractional anisotropy on diffusion tensor magnetic resonance imaging is associated with cognitive improvement after uncomplicated carotid endarterectomy: Tract-based spatial statistics analysis. Neurosurgery. 2013. 73: 592-9
10. Takagi Y, Kikuta K, Nozaki K, Hashimoto N. Histological features of middle cerebral arteries from patients treated for Moyamoya disease. Neurol Med Chir (Tokyo). 2007. 47: 1-4