- Department of Neurological Surgery, University of Miami, Miami, Florida, United States.
DOI:10.25259/SNI_81_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Annelise Claire Sprau, Heather J. McCrea. Intracranial arachnoid cysts in an infant: A technical note on the innovative use of navigation and flexible endoscopy for cyst fenestration. 14-Apr-2021;12:160
How to cite this URL: Annelise Claire Sprau, Heather J. McCrea. Intracranial arachnoid cysts in an infant: A technical note on the innovative use of navigation and flexible endoscopy for cyst fenestration. 14-Apr-2021;12:160. Available from: https://surgicalneurologyint.com/surgicalint-articles/10712/
Abstract
Background: Intracranial arachnoid cysts (ACs) are a cerebral spinal fluid (CSF) collection within the meninges. They typically arise during embryologic development. Some are stable overtime with little consequence, but large or growing cysts may require surgical intervention. The optimal surgical technique is debated and may be more technically challenging in the infant age group.
Case Description: Our unique case report details a 10-month-old (6 months corrected age) infant who presented with a drastic increase in head circumference and was found to have midline shift and three cysts – one large and two smaller ones. He was treated with an innovative surgical approach combining stereotactic introduction of a catheter to facilitate subsequent flexible endoscopy allowing three separate cysts to be treated through one small surgical incision with no complications and a stable examination on 2-year follow-up.
Conclusion: Symptomatic ACs in the infant population that require treatment can be addressed with open surgery to fenestrate the cyst, endoscopic cyst fenestration, or cystoperitoneal shunting. Typically, surgeons must choose between a rigid endoscope which allows stereotactic navigation or a flexible endoscope which allows multiple trajectories but precludes navigation. Our case demonstrates that combining stereotactic ventricular placement before flexible endoscopy provides the benefit of both approaches and allows for successful endoscopic treatment in a young patient with durable results.
Keywords: Endoscopy, Infant, Intracranial arachnoid cysts, Minimally invasive
INTRODUCTION
Intracranial arachnoid cysts (ACs) are collections of cerebrospinal fluid (CSF) within the meninges.[
ILLUSTRATIVE CASE
History
An ex-25.2-week premature infant with extensive complications of prematurity and a history of a 2.2 × 1.2 × 1.4 cm parieto-occipital cystic mass [
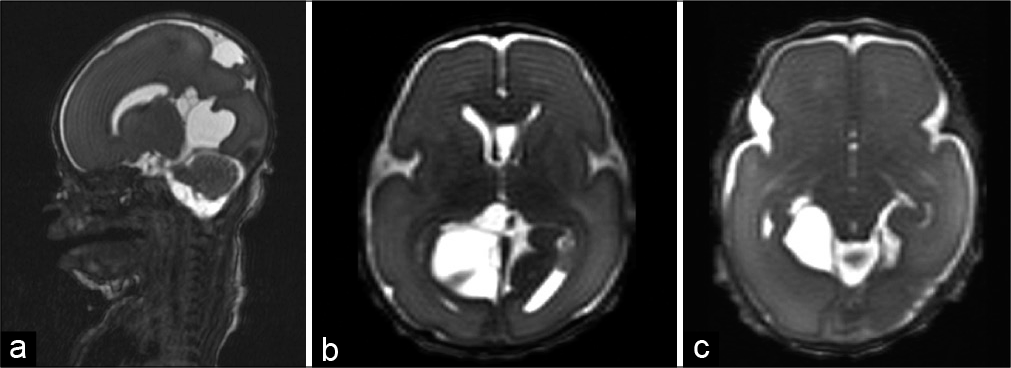
Figure 1:
MRI performed on day of life 4. T2-weighted MRI of sagittal (a) and axial (a&c) cuts demonstrating a multiloculated cystic mass measuring approximately 1.7 × 1.3 × 3.2 cm. There is an additional CSF equivalent cystic mass located superiorly and posteriorly, immediately adjacent to the right side of the superior sagittal sinus.
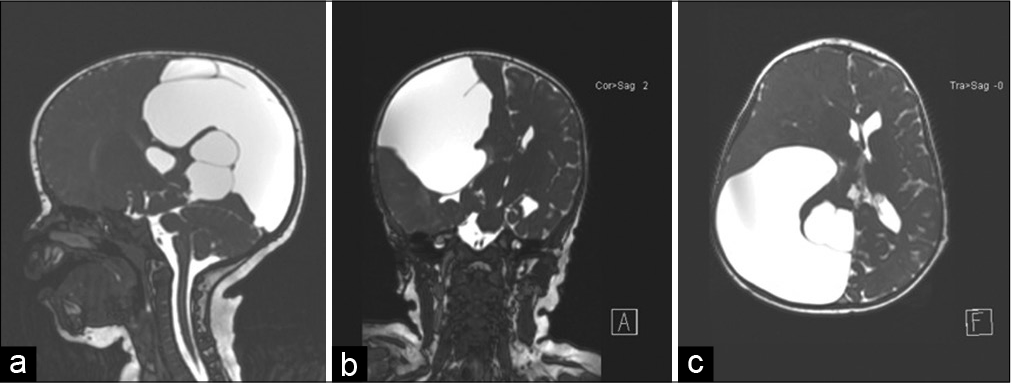
The mother denied any episodes of seizure activity, vomiting, or change in behavior. His head circumference had increased over 1 month to 47.5 cm (>99th percentile) from 46 cm (97th percentile). MRI demonstrated increased mass effect on the adjacent brain and approximately 1.3 cm leftward midline shift. The patient was noted to have three cysts – one large cyst and two smaller ones [
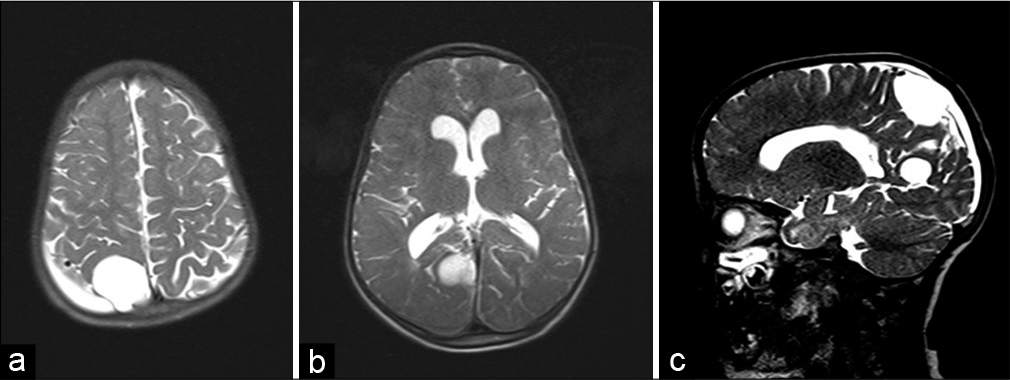
Figure 2:
MRI performed at 10 months old uncorrected (6 months corrected age). T2-weighted MRI of sagittal (a), coronal (b), and axial (c) cuts demonstrating three cysts with significant enlargement of the cysts in the right parieto-occipital temporal lobe causing significant mass effect on the adjacent brain and approximately 1.3 cm leftward midline shift.
Due to the developing midline shift and growing cysts, the patient required surgical treatment. We utilized a combined approach of introducing a ventricular catheter stereotactically to fencepost the site of the fenestration followed by flexible endoscopy to widen the fenestration and fenestrate the two additional cysts into the larger cyst and the system into the temporal horn [
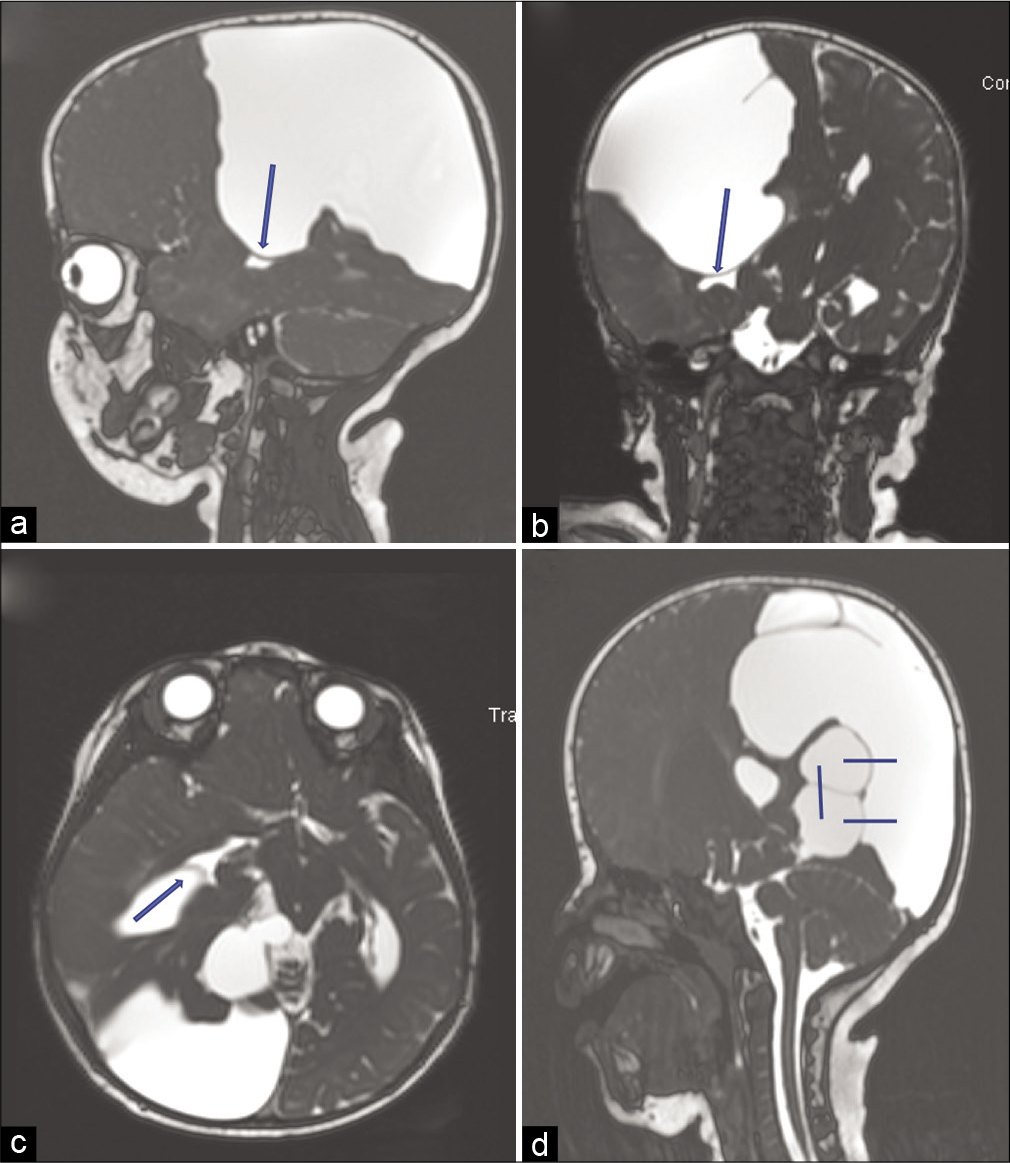
Figure 3:
Preoperative T2-weighted MRI of sagittal (a), coronal (b), and axial (c) cuts with location of planned fenestrations between the large cyst into the right temporal horn (arrow). T2-weighted sagittal MRI (d) demonstrating planned fenestrations from the larger cyst into the two smaller cysts and fenestration between the two smaller cysts (lines).
Operative details
The patient was placed supine with the head turned left exposing the right parieto-occipital region. The patient was registered to the stealth axiom navigation system. We planned a high right parieto-occipital trajectory from the largest cyst into the right temporal horn. We made a small mini-craniotomy in the standard fashion. A ventricular catheter was placed through the largest of the cysts and into the right temporal horn with a direct trajectory utilizing stereotactic navigation of the catheter tip. We then tied off this catheter and cut it, leaving it in place, and subsequently introduced the flexible endoscope into the cyst next to this catheter. The ventricular catheter was visualized with tip puncturing the cyst wall. A Bugbee wire was introduced adjacent to the ventricular catheter which marked the entrance into the temporal horn. Manipulating the wire enlarged the hole, and then after removal of the wire, a #3 embolectomy catheter was placed through the hole and inflated to widen this hole further. We then removed the ventricular catheter and advanced the endoscope into the temporal horn through this fenestration. We were able to visualize ependyma and choroid plexus confirming our presence in the ventricular system. At this point, the large cyst was significantly decompressed.
Next, we withdrew the flexible endoscope back into the larger cyst and redirected it posteriorly to focus on the inferior of the two medial cysts. We also utilized ultrasound adjacent to the endoscope to assess the configuration of the remaining two smaller cysts. We introduced the Bugbee wire through the endoscope to make a hole between the larger cyst we were within and the inferior smaller cyst. This was widened with the #3 embolectomy catheter and then the endoscope was passed into the cyst for visual inspection. We then similarly fenestrated from the largest cyst to the superior small cyst through the same sequence and then repeated this process to fenestrate the superior small cyst into the inferior small cyst [
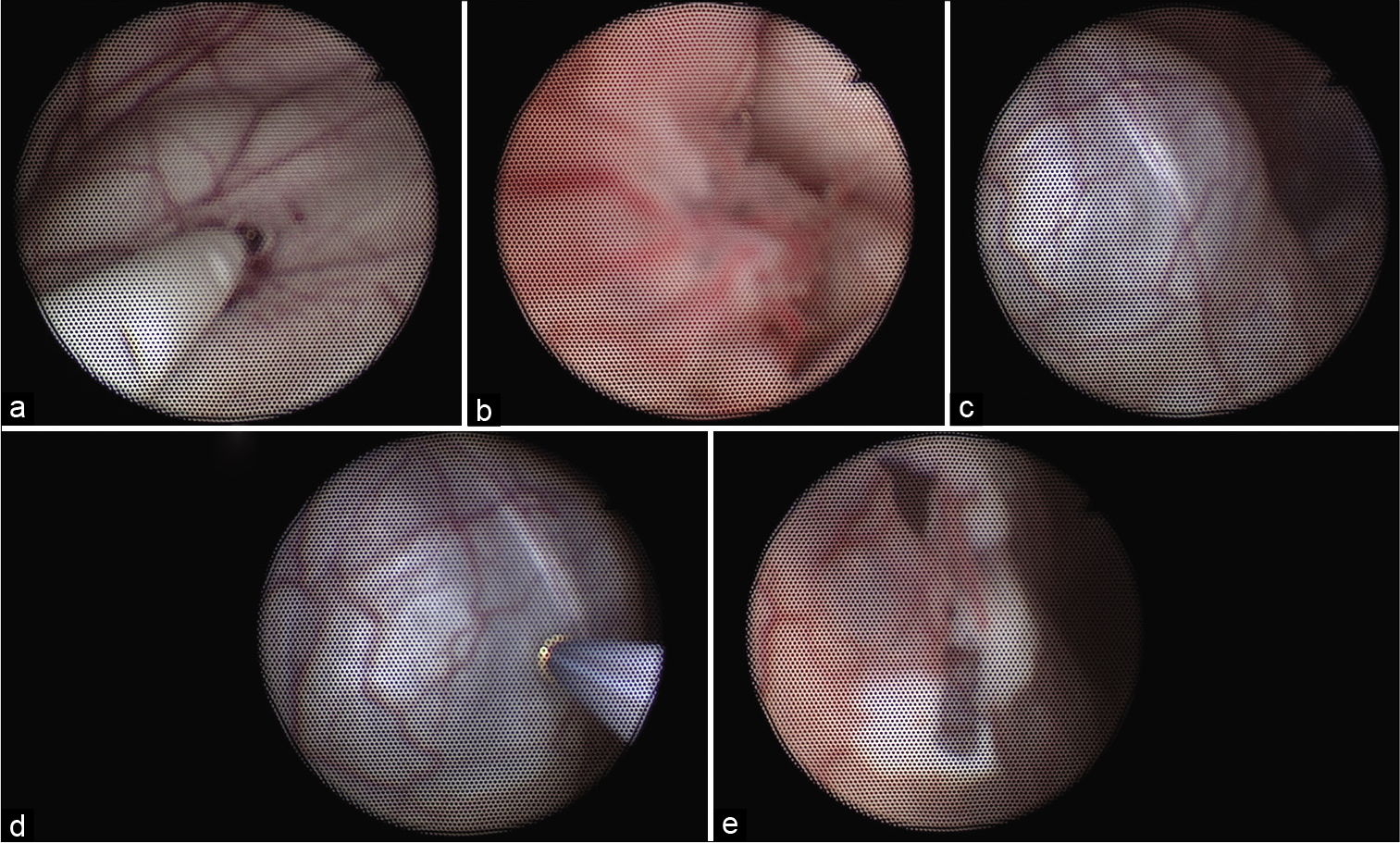
Figure 4:
Intraoperative endoscopic view of a ventricular catheter (a) placed in the largest parieto-occipital cyst with trajectory into the right temporal horn. View through this fenestration into the temporal horn with visualization of choroid plexus to confirm intraventricular location (b). Medial fluid-filled arachnoid cysts (c and d). Fenestrations made from largest cyst into medial arachnoid cysts (e).
In total, we had created four fenestrations – a communication from the large cyst into the right temporal horn, a communication from the large cyst into each of the smaller cysts, and a communication between the two smaller cysts, thus allowing for full communication of the cystic structures and decompression of the mass effect they caused. There were no complications.
Postoperative course
The patient was followed at regular intervals postoperatively. At his 2-year postoperative follow-up, he had a stable head circumference at the 85th percentile for corrected age on CDC growth curve, imaging was stable, and patient demonstrated appropriate developmental progress with significant increase in language maturity [
Figure 5:
Two-year postoperative T2-weighted MRI of axial (a/b) and sagittal (c) cuts demonstrating grossly stable size and appearance of arachnoid cysts in the right parietal and occipital regions and right parieto-occipital subdural fluid collection. There is stable mild dilation of the lateral and third ventricles.
DISCUSSION
We report a rare case of multiple, symptomatic ACs treated with an innovative surgical approach combining stereotactic introduction of a catheter to facilitate subsequent flexible endoscopy allowing three separate cysts to be treated through one small surgical incision.
Natural history
ACs are classically thought to arise from either erroneous arachnoid membrane splitting or duplication, typically during embryologic development. Other etiologies in the literature illustrate de novo cyst formation from head trauma or intraventricular hemorrhage of prematurity.[
A recent single-institution retrospective review of 11,738 patients found a pediatric prevalence rate of 2.6%, an increase from prior studies which reported AC prevalence between 0.2 and 1.7%.[
Treatment
Cysts can be treated through cystoperitoneal shunt, open craniotomy for fenestration, or endoscopic fenestration. CP shunting is relatively straightforward and provides a gradual, predictable change in cyst volume and pressure dynamics.[
Open craniotomy for cyst fenestration allows for the avoidance of a permanent shunt; however, some express concern about its true efficacy due to cyst recurrence, especially in the younger population.[
Neuroendoscopy, a rapidly advancing technique within the field of neurosurgery during the past two decades, has gained momentum for treatment of ACs as a sound compromise which minimizes the extent of surgery while avoiding a permanent shunt.[
Technical pearls from illustrative case
Our patient, with an extensive medical history and multiple cysts causing mass effect, required careful surgical planning. Given the presence of three cysts and need to make four fenestrations, multiple trajectories for fenestration were required. This need for multiple trajectories favored the use of the flexible endoscope. However, flexible endoscopy typically precludes the use of stereotactic navigation, which was critical in this case to identify the site to fenestrate from the larger cyst into the ventricular system. Identifying this site once inside the cyst without navigation would have been challenging and posed a significant risk if the site could not be appropriately identified. By the use of a novel combined approach of introducing a ventricular catheter stereotactically to fencepost the site of this fenestration followed by flexible endoscopy to widen this fenestration, fenestrate the two additional cysts into the larger cyst, and fenestrate the two smaller cysts into each other, the patient was able to safely be treated endoscopically through one small incision. This innovative surgical approach allowed safe, minimally invasive treatment with lasting clinical improvement.
CONCLUSION
The management of symptomatic ACs in infants is mostly based on small, single-center series and there are no current guidelines for management. While craniotomies are performed in older patients, there is thought that this technique is less durable and efficacious in infants compared to their older counterparts. CP shunting is commonly utilized in the infant population as it is less technically challenging but leads to lifelong shunt dependence. Combining stereotactic ventricular placement before flexible endoscopy may allow for a greater number of these cysts to be treated endoscopically in younger patients with durable results.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alexiou GA, Varela M, Sfakianos G, Prodromou N. Shunting for the treatment of arachnoid cysts in children. Neurosurgery. 2010. 67: 1632-6
2. Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr. 2010. 5: 578-85
3. Ali M, Bennardo M, Almenawer SA, Zagzoog N, Smith AA, Dao D. Exploring predictors of surgery and comparing operative treatment approaches for pediatric intracranial arachnoid cysts: A case series of 83 patients. J Neurosurg Pediatr. 2015. 16: 275-82
4. Ali ZS, Lang SS, Bakar D, Storm PB, Stein SC. Pediatric intracranial arachnoid cysts: Comparative effectiveness of surgical treatment options. Childs Nerv Syst. 2014. 30: 461-9
5. Greenfield JP, Souweidane MM. Endoscopic management of intracranial cysts. Neurosurg Focus. 2005. 19: E7
6. Hall S, Smedley A, Sparrow O, Mathad N, Waters R, Chakraborty A. Natural history of intracranial arachnoid cysts. World Neurosurg. 2019. 126: e1315-20
7. Nowoslawska E, Polis L, Kaniewska D, Mikolajczyk W, Krawczyk J, Szymanski W. Neuroendoscopic techniques in the treatment of arachnoid cysts in children and comparison with other operative methods. Childs Nerv Syst. 2006. 22: 599-604
8. Palin M, Anderson I, O’Reilly G, Goodden JR. A suprasellar arachnoid cyst resulting from an intraventricular haemorrhage and showing complete resolution following endoscopic fenestration. BMJ Case Rep. 2015. 2015: bcr2015209290
9. Preuss M, Thome U, Kluge J, Hirsch FW, Viehweger A, Nestler U. Retroclival arachnoid cyst in a preterm infant after ventriculitis and intraventricular hemorrhage-a case report. Childs Nerv Syst. 2015. 31: 347-50
10. Schroeder HW, Gaab MR. Endoscopic observation of a slit-valve mechanism in a suprasellar prepontine arachnoid cyst: Case report. Neurosurgery. 1997. 40: 198-200
11. Shim KW, Park EK, Kim DS, Choi JU. Neuroendoscopy: Current and future perspectives. J Korean Neurosurg Soc. 2017. 60: 322-6
12. Tamburrini G, Caldarelli M, Massimi L, Santini P, Di Rocco C. Subdural hygroma: an unwanted result of Sylvian arachnoid cyst marsupialization. Childs Nerv Syst. 2003. 19: 159-65
13. Turhan T, Ersahin Y, Akinturk N, Mutluer S. ‘Fenestration methods for sylvian arachnoid cysts--endoscopy or microsurgery. Childs Nerv Syst. 2012. 28: 229-35
14. Yokoyama K, Sugie A, Yamada M, Tanaka H, Ito Y, Yamashita M. Formation of de novo symptomatic premedullary arachnoid cyst in adult. World Neurosurg. 2019. 130: 154-6
15. Zhang B, Zhang Y, Ma Z. Long-term results of cystoperitoneal shunt placement for the treatment of arachnoid cysts in children. J Neurosurg Pediatr. 2012. 10: 302-5