- Department of Neurosurgery, UHC Nene Tereza, Tirane, Albania.
- Department of Emergency, UHC Nene Tereza, Tirane, Albania.
- Department of Anesthesia-Reanimation UHC Nene Tereza, Tirane, Albania.
- Department of Plastic and Reconstructive Surgery, UHC Nene Tereza, Tirane, Albania.
Correspondence Address:
Artur Xhumari, Department of Neurosurgery, UHC Nene Tereza, Tirane, Albania.
DOI:10.25259/SNI_722_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Artur Xhumari1, Edmond Zaimi2, Myfit Saraci3, Gentian Zikaj4. Intracranial hypotension as a unique complication of the rupture of an anterior sacral meningocele into a recurrent pilonidal cyst. 13-Sep-2021;12:463
How to cite this URL: Artur Xhumari1, Edmond Zaimi2, Myfit Saraci3, Gentian Zikaj4. Intracranial hypotension as a unique complication of the rupture of an anterior sacral meningocele into a recurrent pilonidal cyst. 13-Sep-2021;12:463. Available from: https://surgicalneurologyint.com/surgicalint-articles/11107/
Abstract
Background: Intracranial hypotension (IH) is an underdiagnosed, but important cause of new-onset, daily persistent headache, especially among the young- and middle-aged population. It results from a cerebrospinal fluid (CSF) leak with subsequent lowered CSF pressure.
Case Description: A 37-year-old female presented to the emergency department with sudden onset severe headaches. Two years earlier, she had undergone surgery for resection of a pilonidal cyst (PC). The night before admission, she had watery discharge from the recurrent PC and severe diffuse positional headaches associated with photophobia and neck pain. The head computed tomography showed pneumocephalus in the posterior fossa and a spine magnetic resonance imaging revealed an anterior sacral meningocele (ASM) in close contact with the recurrent PC. A final diagnosis was made of headaches due to IH. The leakage site was the rupture of the ASM in the PC. The surgical repair of the ASM was achieved suturing two overlapping dural flaps. There was no more CSF leakage from the PC and the headaches disappeared.
Conclusion: This is a unique case of IH due to the rupture of an ASM into a recurrent PC. The association of an ASM and PC, at the best of our knowledge, is unique. Moreover, the fistulation of the ASM to the PC is exceptional. ASM can be successfully closed with a posterior approach, using two overlapping dural flaps.
Keywords: Anterior sacral meningocele, Intracranial hypotension, Pilonidal cyst
INTRODUCTION
Intracranial hypotension (IH) is an underdiagnosed, but important cause of new-onset, daily persistent headache, especially among the young- and middle-aged population. It results from a cerebrospinal fluid (CSF) leak with subsequent lowered CSF pressure. Here, we present a 37-year-old female with IH. The CSF leak was found to be the rupture of an anterior sacral meningocele (ASM) into a recurrent pilonidal cyst (PC). Surgical repair of the ASM resulted in the long-term resolution of the headaches.
CASE REPORT
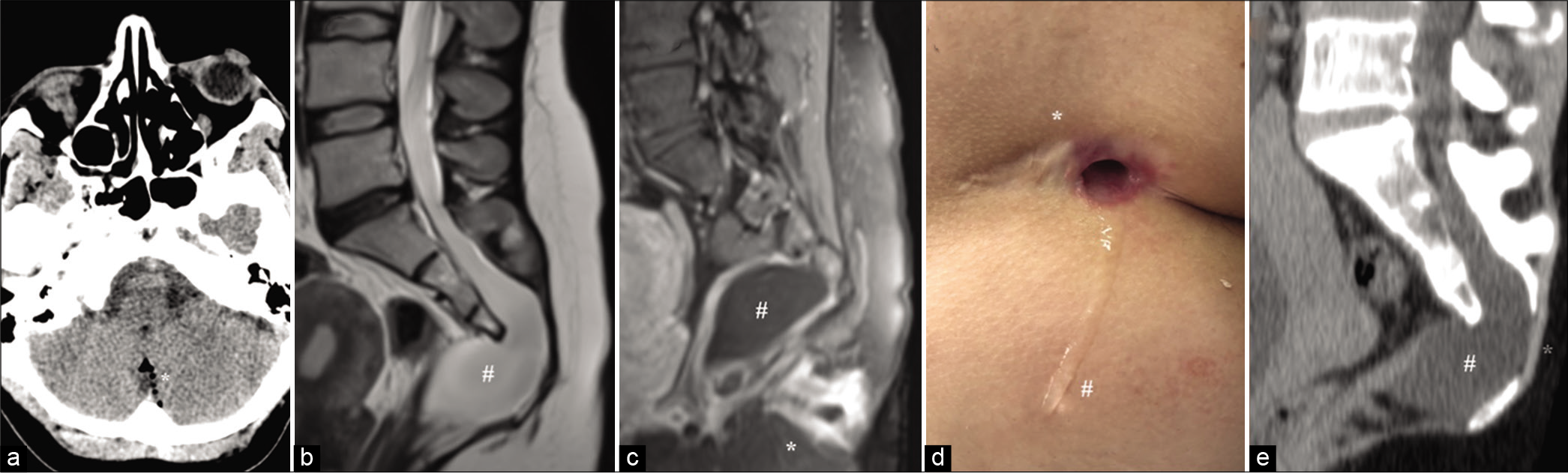
A 37-year-old female presented to the emergency department (ED) with sudden onset severe headaches. Two years earlier, she had undergone surgery for resection of a PC. A year and a half later, the cyst recurred and was also associated with intermittent purulent discharge. The night before admission, she had watery discharge from the cyst and severe diffuse positional headaches associated with photophobia and neck pain. Differential diagnosis included migraine, meningitis, and subarachnoid hemorrhage. The head computed tomography (CT) obtained in ED showed pneumocephalus in the posterior fossa [
Figure 1:
(a) Head computed tomography (CT) shows pneumocephalus in the posterior fossa (*). (b) T2-weighted sacral sagittal magnetic resonance imaging (MRI) revealed an anterior sacral meningocele (ASM) (#). (c) Contrast T1-weighted sacral sagittal MRI revealed an ASM whose caudal pole (#) was in contact with the recurrent pilonidal cyst (PC) (*). (d) Clear liquid (#) draining from the PC (*), increasing with Valsalva maneuver. (e) Sacral sagittal CT showed spina bifida (*) and the agenesis of a portion of the anterior sacrum (#).
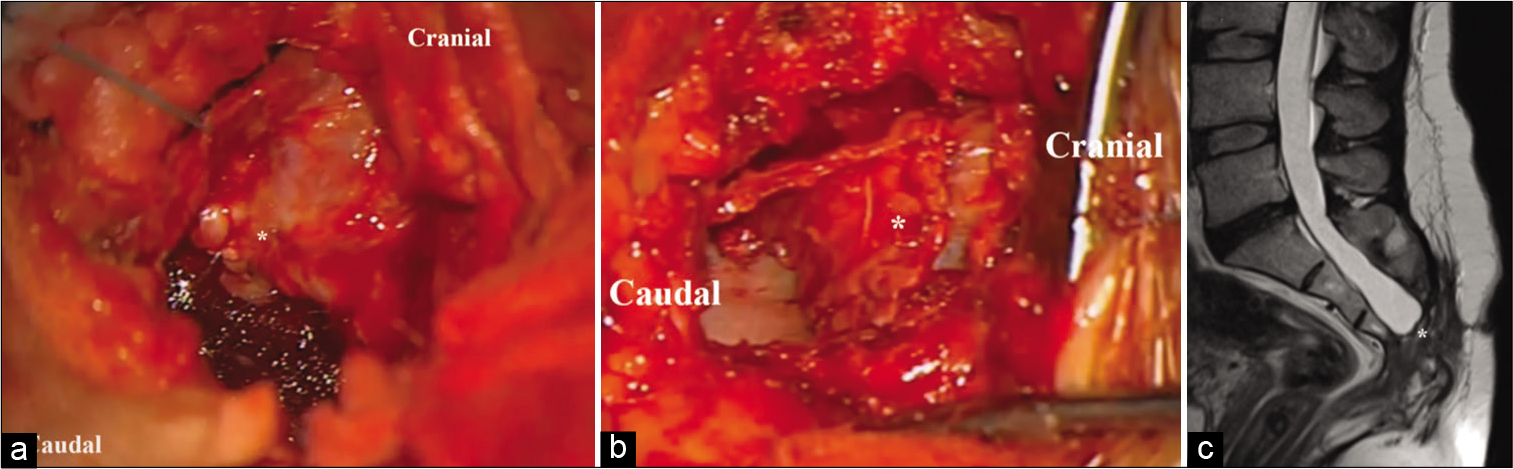
A final diagnosis was made of headaches due to IH. The leakage site was the rupture of the ASM in the recurrent PC. We decided to repair the ASM. The patient was positioned prone. A transverse incision exposed and enlarged the posterior sacral defect. Under operating microscope, we opened the dura in “U” fashion flap. There were no nerves entering the anterior meningocele. The dural flap was sutured in watertight fashion to the spinal canal dura [
Figure 2:
Intraoperative view showing (a) the first dural flap (*) suture over the spinal canal dura and (b) the second flap (*) sutured in a watertight fashion over the first flap. (c) Follow-up T2-weighted sagittal sacral magnetic resonance imaging confirmed the total closure of the anterior sacral meningocele (*).
DISCUSSION
This is a unique case of IH due to the rupture of an ASM in to a recurrent PC. IH is characterized clinically by severe headaches which typically worsen on standing up and get better when lying down. It results from a CSF leak with subsequent lowered CSF pressure. Spontaneous IH (SIH) is an underdiagnosed, but important cause of new-onset, daily persistent headache, especially among the young- and middle-aged population. The diagnosis of SIH is rarely made at the initial physician visit and typically patients endure weeks, months, or even years of treatment for a variety of neurologic disorders. Most likely, this is due to the unfamiliarity of physicians with the syndrome of SIH.[
In the presented case, even though the patient described the watery discharge from the fistula and the appearance of the headaches immediately after, the diagnosis of SIH was not made from the ED physician who still is not aware of SIH symptoms. It was the neuroradiologist who suspected the CSF leakage based on the presence of intracranial air on CT.
ASM is a rare congenital defect seen in the anterior aspect of the spine. It is defined as a meningeal cyst that occurs in the presacral space secondary to agenesis of a portion of the anterior sacrum. ASM is more common in white females and usually becomes symptomatic in the second or third decades of life (e.g., at childbearing age). As ASM is not typically associated with cutaneous abnormalities or posterior spina bifida, many patients with ASM remain asymptomatic or show minor symptoms (e.g., constipation, dysuria, and dysmenorrhea pressure on the rectum, urinary bladder/ female genital organ findings).[
In the presented case, ASM was, till the rupture, asymptomatic and was an unexpected discovery in the spine MRI performed to find the CSF leakage site. When an ASM is symptomatic, surgical treatment is recommended.[
PC is a hair-containing sacrococcygeal dermoid cyst or sinus, often opening at a postanal dimple, believed to result from an infolding of skin in which hair continues to grow. Incidence of pilonidal disease is about 26 per 100,000 population. Pilonidal disease occurs predominantly in males, at a ratio of about 3–4:1. It occurs predominantly in white patients, typically in the late teens to early twenties, decreasing after age 25 and rarely occurs after age 45.[
The association of an ASM and PC, at the best of our knowledge, is unique. Nevertheless, this association, in our opinion, does not impose the systematic search for an accompanying condition to the PC. Moreover, the fistulation of the ASM to the PC is exceptional. We suggest that the recurrent infections of the PC have slowly eroded and finally caused the rupture of the ASM. If the PC had not recurred, the ASM, on long term, might have remained asymptomatic.
CONCLUSION
This is an exceptional case of IH due to the rupture of an ASM into a recurrent PL. The association of an ASM and PC, at the best of our knowledge, is unique. Moreover, the fistulation of the ASM to the PC is exceptional. ASM can be successfully closed with a posterior approach, using two overlapping dural flaps. Neurologist and neurosurgeons must raise awareness of the syndrome of IH as still it is an underdiagnosed syndrome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. da Silva JH. Pilonidal cyst: Cause and treatment. Dis Colon Rectum. 2000. 43: 1146-56
2. Fitzpatrick MO, Taylor WA. Anterior sacral meningocele associated with a rectal fistula. Case report and review of the literature. J Neurosurg. 1999. 91: 124-7
3. Hull TL, Wu J. Pilonidal disease. Surg Clin North Am. 2002. 82: 1169-85
4. Koksal A, Canyigit M, Kara T, Ulus A, Gokbayir H, Sarisahin M. Unusual presentation of an anterior sacral meningocele: Magnetic resonance imaging, multidetector computed tomography, and fistulography findings of bacterial meningitis secondary to a rectothecal fistula. Jpn J Radiol. 2011. 29: 528-31
5. Mankotia DS, Sawarkar DP, Singh PK, Kumar A, Verma SK, Chandra PS. Rare case of cerebrospinal fluid proctorrhea caused by anterior sacral meningocele with rectothecal fistula. World Neurosurg. 2018. 114: 323-5
6. Massimi L, Calisti A, Koutzoglou M, di Rocco C. Giant anterior sacral meningocele and posterior sagittal approach. Childs Nerv Syst. 2003. 19: 722-8
7. Phillips JT, Brown SR, Mitchell P, Shorthouse AJ. Anaerobic meningitis secondary to a rectothecal fistula arising from an anterior sacral meningocele: Report of a case and review of the literature. Dis Colon Rectum. 2006. 49: 1633-5
8. Rahimizadeh A, Ehteshami S, Rahimizadeh A, Karimi M. Anterior sacral meningocele complicated by rectothecal fistula and rectorrhea: A case report and review of the literature. Surg Neurol Int. 2020. 11: 117
9. Sánchez AA, Iglesias CD, López CD, Cecilia DM, Gómez JA, Barbadillo JG. Rectothecal fistula secondary to an anterior sacral meningocele. J Neurosurg Spine. 2008. 8: 487-9
10. Schievink WI, Dodick DW, Mokri B, Silberstein S, Bousser MG, Goadsby PJ. Diagnostic criteria for headache due to spontaneous intracranial hypotension: A perspective. Headache. 2011. 51: 1442-4
11. Schievink WI. Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol. 2003. 60: 1713-8
12. Tani S, Okuda Y, Abe T. Surgical strategy for anterior sacral meningocele. Neurol Med Chir (Tokyo). 2003. 43: 204-9