- Department of Neurosurgery, Grupo Neurológico de Alta Especialidad, Hospital Angeles Morelia, Morelia Michoacan, Mexico
- Department of Neurosurgery, Instituto Nacional de Neurología y Neurocirugía “Manuel Velasco Suárez”, Ministry of Health, Mexico City, Mexico
- Department of Neurosurgery, Centro Médico Lic. Adolfo López Mateos, Health Institute of the State of Mexico, Toluca, State of Mexico, Mexico.
Correspondence Address:
Abrahan Alfonso Tafur-Grandett, Department of Neurosurgery, Centro Médico Lic. Adolfo López Mateos, Health Institute of the State of Mexico, Toluca, State of Mexico, Mexico.
DOI:10.25259/SNI_1098_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alejandro Ceja Espinosa1,2, Juan Pablo Navarro-Garcia de Llano2, Juan Carlos Balcázar-Padrón2, Abrahan Alfonso Tafur-Grandett3. Intracranial migration of a ventriculoperitoneal shunt: A case report and literature review. 24-Mar-2023;14:103
How to cite this URL: Alejandro Ceja Espinosa1,2, Juan Pablo Navarro-Garcia de Llano2, Juan Carlos Balcázar-Padrón2, Abrahan Alfonso Tafur-Grandett3. Intracranial migration of a ventriculoperitoneal shunt: A case report and literature review. 24-Mar-2023;14:103. Available from: https://surgicalneurologyint.com/surgicalint-articles/12210/
Abstract
Background: The intracranial migration of a ventriculoperitoneal shunt (VPS) has been previously described, it is a very rare event, and the mechanisms of this migration have not yet been elucidated.
Case Description: Newborn at 38 weeks of gestation by cesarean section, with congenital hydrocephalus due to Dandy–Walker malformation that required right Frazier VPS placement. At 2-month follow-up, computed tomography of the skull showed cranial migration of VPS and dysfunction. At evaluation, there were signs of systemic infection. External ventricular drainage was placed and an intravenous antibiotic scheme for Gram-positive bacteria was started. After 3 months, cerebrospinal fluid cultures were negative and definitive VPS was decided.
Conclusion: Different possible mechanisms have been proposed, such as negative intraventricular pressure, positive intra-abdominal pressure, use of valveless catheters, excessive burr hole size, as well as such as occipital ventricular access, thin cortical mantle, incorrect distal and proximal fixation, short distance between the peritoneum and ventricles, and a possible inflammatory reaction to the catheter material (silicone). A combination of these different mechanisms contributes to proximal shunt migration. Although the placement of a VPS is a procedure well taught since the 1st years of neurosurgical residency, it is not exempt from complications. Although, as was previously stated in this paper, the incidence of a complete cranial VPS migration is extremely rare, and only a few cases are documented, it is still important to report this type of cases and to try to elucidate the possible mechanisms involved.
Keywords: Complications, Migration, Ventriculoperitoneal shunt
INTRODUCTION
Intracranial migration of a ventriculoperitoneal shunt (VPS) has been previously described,[
Since 1955, the first case related to VPS migration was reported by Scott et al.,[
CASE REPORT
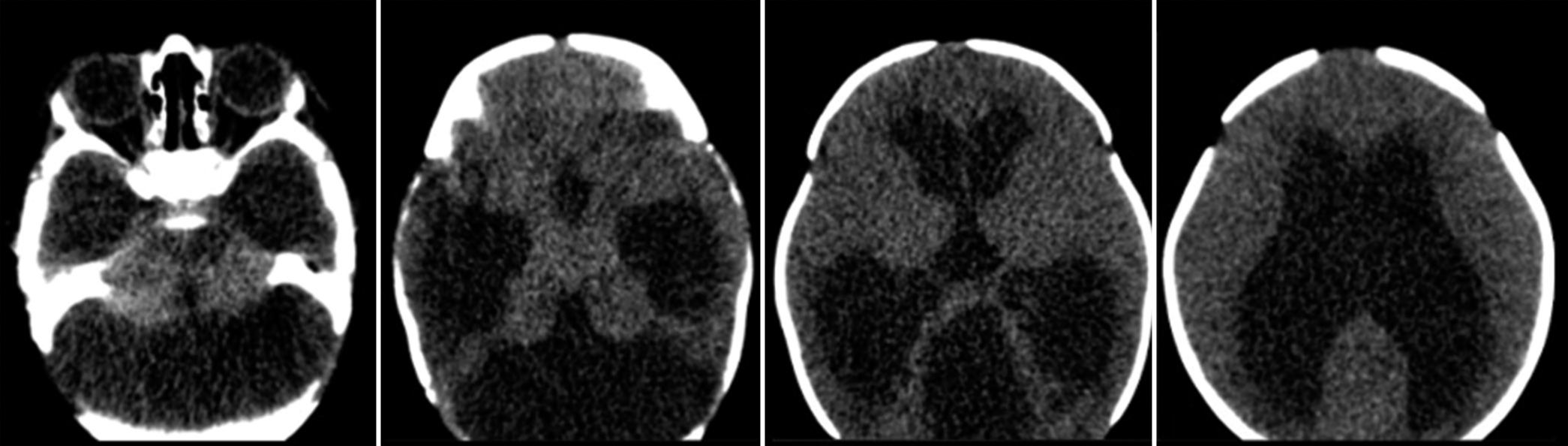
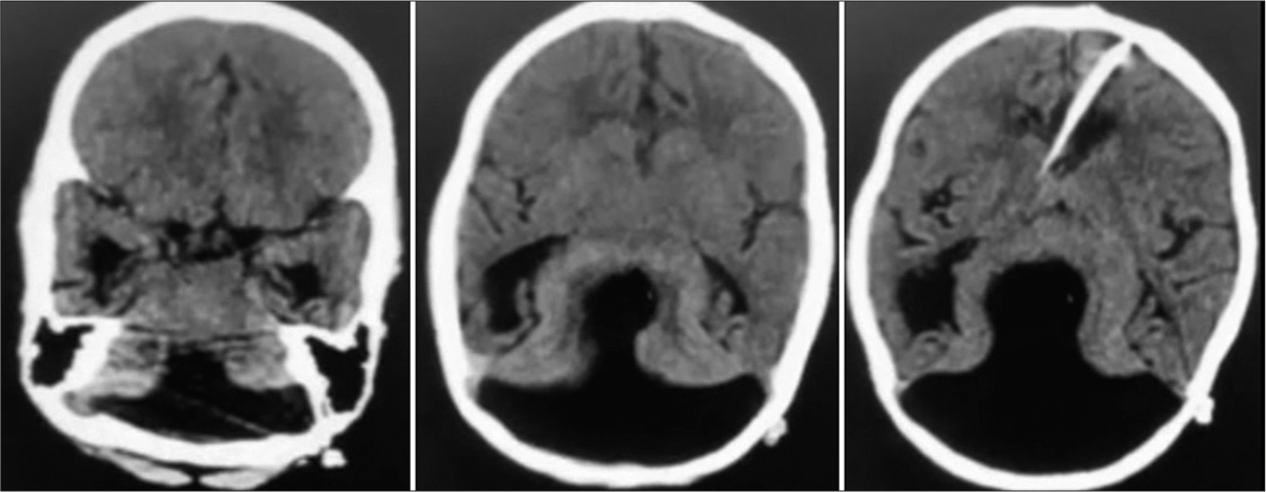
Newborn female delivered at 38 weeks of gestation by cesarean section, suffering from congenital hydrocephalus diagnosed 4 weeks before birth that required the placement of a VPS. At the moment of delivery, the patient presented an Apgar score of 8 and 9 at 1 and 5 min, respectively. On the next day after birth, the patient underwent a simple head computed tomography (CT) scan where Dandy–Walker malformation and radiological signs of hydrocephalus were appreciated [
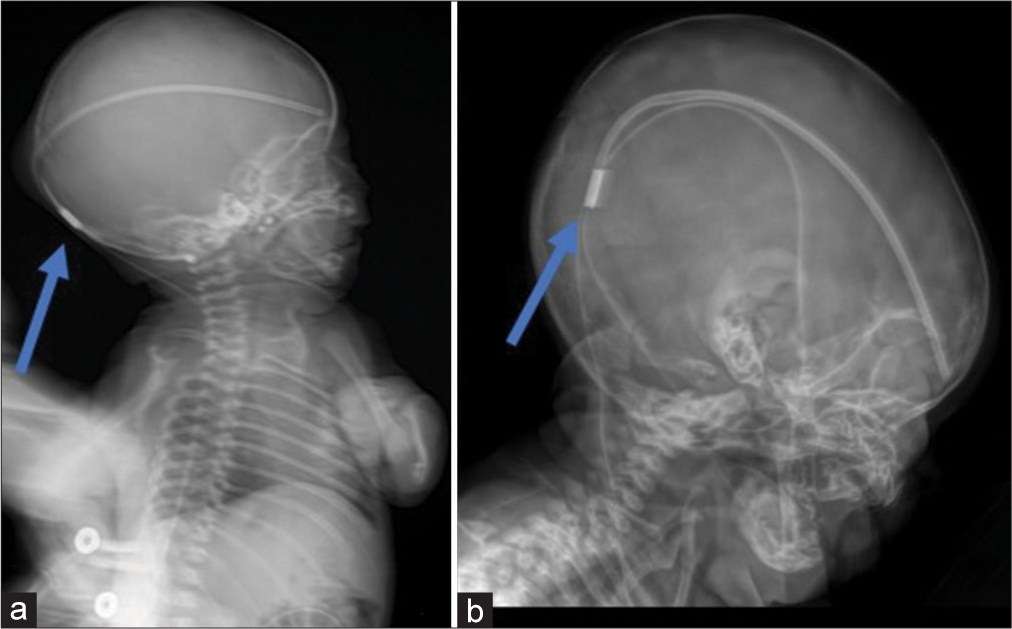
At 1- and 2-months follow-up, the X-rays and simple head CT showed that the VPS cranially migrated and was not appropriately working [
Figure 2:
(a). X-ray 1 month after placement of the ventriculoperitoneal shunt. The blue arrow shows the situation of the system reservoir which is in the extracranial subgaleal space, a bulging in the scalp is noticed. (b). X-ray 2 months after placement of the ventriculoperitoneal shunt. The blue arrow shows the cranial migration of the system.
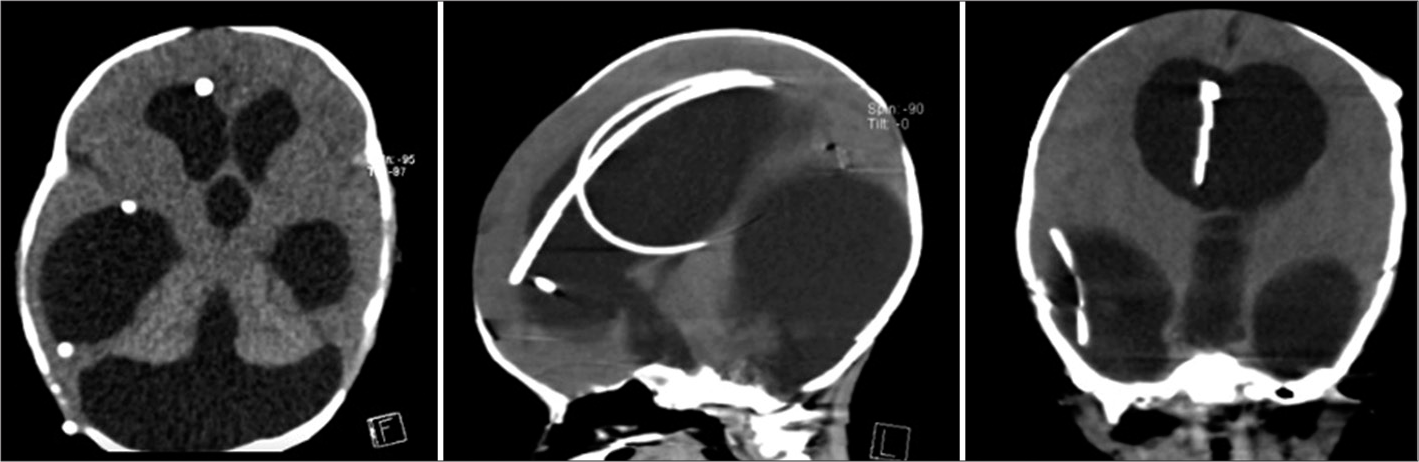
A second VPS was placed in the left Kocher point, which unfortunately failed to work correctly [
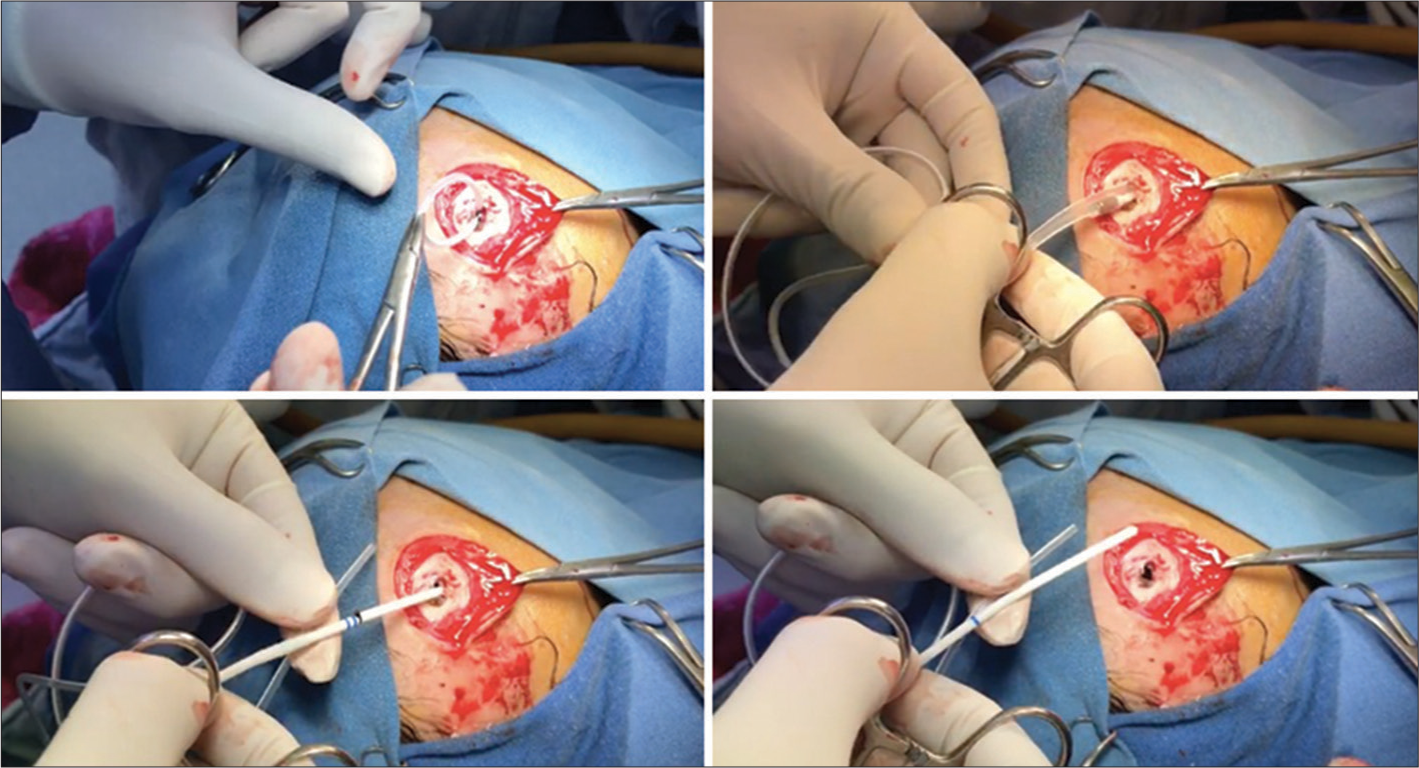
Subsequently, the patient was transferred to our hospital. On her arrival, she presented signs of systemic infection such as fever and leukocytosis, making the removal of both systems and cerebrospinal fluid (CSF) culture the most appropriate approach [
Due to the lack of resources, this had to be done without using a neuroendoscope.
Forty-eight hours later, the cultures growth Gram-positive bacteria. Afterward, external ventricular drainage (EVD) was collocated, and an intravenous antibiotics scheme was initiated. Due to intraventricular infection and the need for EVD replacement, the patient required 12 subsequent surgeries. After these procedures and a lengthy hospital stay of 3 months, CSF cultures were negative, and a definitive VPS was placed.
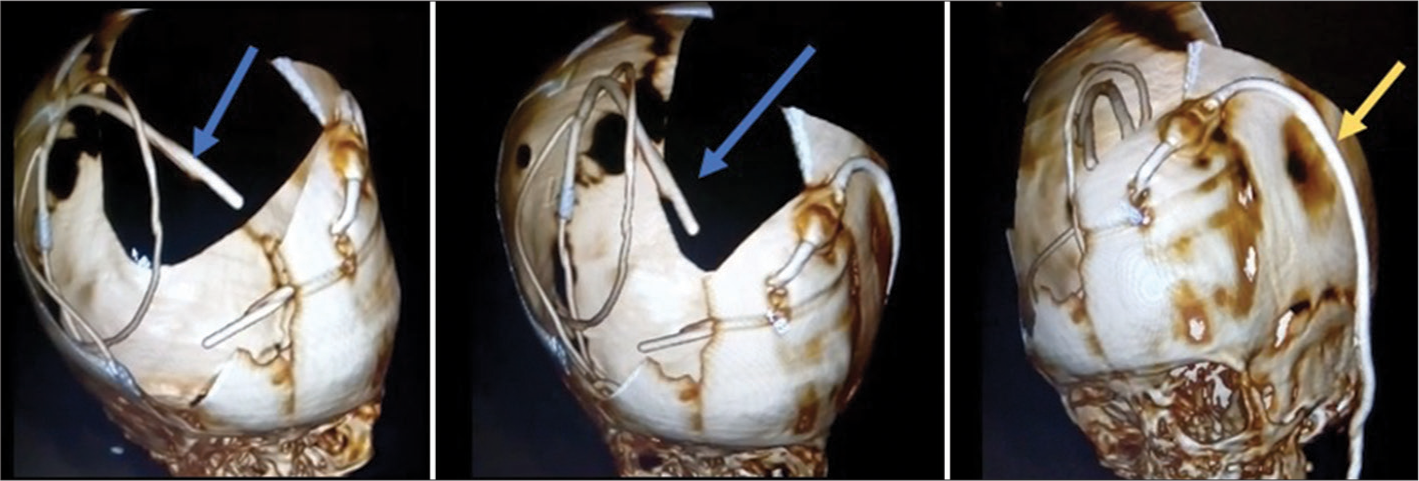
As of November 2021, with the help of physical therapy and rehabilitation, the patient is 3 years old, attends a local school, and the system is still functional with no signs of neurological deficit [
DISCUSSION
A rare complication of ventriculoperitoneal bypass surgery is total cranial migration of the system. Few cases have previously been described and different possible mechanisms have been proposed, which may be avoidable, such as excessive movements of the neck and head, incorrect distal and proximal fixation, supine position, the use of catheters without valves, lack of use of a reservoir, excessive size of the burr hole and dural incision, as well as occipital ventricular access; and unavoidable such as negative intraventricular pressure, positive intra-abdominal pressure, thin cortical mantle, short distance between the peritoneum and ventricles (compared to an adult), and a possible inflammatory reaction to the catheter material (silicone).[
Once the mechanisms involved are considered, we suggest the following tips to avoid this complication: (1). Whenever possible, prefer to use Kocher precoronal point. The authors suggest and prefer to perform Kocher’s precoronal trephine since the distance traveled and the angulation of the catheter is less than if the trephine was performed at Frazier’s point. We also consider that when performing with the precoronal trephine the catheter would have to migrate through the entire curvature of the skull and would be less likely to migrate, but is only a hypothesis, we did not find a justification, support or reference in the literature regarding this surgical decision; (2). The exact size of the burr hole and durotomy according to the size of the silicone catheter (the senior author used a number 15 blade with rotational moves to make the burr hole, the dura is coagulated with bipolar forceps in a circle shape of 5 mm, the dura is opened with a second 15 blade in a circle shape that involves only 3 mm opening); (3). Try to place a flat base system (this has the proximal catheter, valve, and distal catheter, which has to be attached on both sides, against the Hakim type that the valvular system and distal catheter are a single piece); (4). Ensure correct fixation of the proximal catheter to the periosteum and distal catheter to the aponeurosis.
CONCLUSION
Although the placement of a VPS is a procedure well taught since the 1st years of neurosurgical residency, it is not exempt from complications. Even though we are aware, the tips we mentioned could be interpreted as a mandatory part of the surgical technique. We want these recommendations to be well received, and they are always kept in mind to avoid these kinds of complications, which, in some cases, can have catastrophic results. Although, as was previously stated in this paper, the incidence of a complete cranial VPS migration is extremely rare, and only a few cases are documented, it is still important to report this type of cases and to try to elucidate the possible mechanisms involved.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Acharya R, Bhutani A, Saxena H, Madan VS. Complete migration of ventriculoperitoneal shunt into the ventricle. Neurol Sci. 2002. 23: 75-7
2. Ammar A, Nasser M. Intraventricular migration of VP shunt. Neurosurg Rev. 1995. 18: 293-5
3. Deo RC, Acharya A, Senapati SB, Panigrahi S, Mohapatra AK. Complete intraventricular migration of ventriculo-peritoneal shunt: A rare case report. Int J Surg Case Rep. 2022. 101: 107772
4. Eljamel MS, Sharif S, Pidgeon CN. Total intraventricular migration of unisystem ventriculo-peritoneal shunt. Acta Neurochir (Wien). 1995. 136: 217-8
5. Garijo JA, Pecourt JC, de la Resurrección M. Migration of ventriculo-peritoneal shunt into lateral ventricle of an adult. Surg Neurol. 1979. 11: 399-400
6. Gupta PK, Dev EJ, Lad SD. Total migration of a ventriculoperitoneal shunt into the ventricles. Br J Neurosurg. 1999. 13: 73-4
7. Lucantoni D, Magliani V, Galzio R, Zenobii M, Cristuib L. Cranial intraventricular migration of Raimondi uni-shunt system. J Neurosurg Sci. 1985. 29: 157-8
8. Mori K, Yamashita J, Handa H. “Missing tube” of peritoneal shunt: Migration of the whole system into ventricle. Surg Neurol. 1975. 4: 57-9
9. Nadkarni TD, Menon RK, Dange NN, Desai KI, Goel A. Cranial migration of complete ventriculo-peritoneal shunt assembly. J Clin Neurosci. 2007. 14: 92-4
10. Scott M, Wycis HT, Murtagh F, Reyes V. Observations on ventricular and lumbar subarachnoid peritoneal shunts in hydrocephalus in infants. J Neurosurg. 1955. 12: 165-75
11. Villarejo F, Alvarez-Sastre C, Gimenez D, Gonzalez C. Migration of an entire one-piece shunt into the ventricle. Neurochirurgia (Stuttg). 1979. 22: 196-8
12. Young HA, Robb PJ, Hardy DG. Complete migration of ventriculoperitoneal shunt into the ventricle: Report of two cases. Neurosurgery. 1983. 12: 469-71