- Department of Cerebrovascular Surgery, International Medical Center, Saitama Medical University, Hidaka, Japan.
Correspondence Address:
Kaima Suzuki, Department of Cerebrovascular Surgery, International Medical Center, Saitama Medical University, Hidaka, Japan.
DOI:10.25259/SNI_99_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Monami Dai, Kaima Suzuki, Hiroki Sato, Shinya Tabata, Haruka Kume, Masaya Nishikata, Keita Tamada, Hidetoshi Ooigawa, Hiroki Kurita. Intracranial mycotic aneurysm rupture following cupping therapy. 05-Apr-2024;15:119
How to cite this URL: Monami Dai, Kaima Suzuki, Hiroki Sato, Shinya Tabata, Haruka Kume, Masaya Nishikata, Keita Tamada, Hidetoshi Ooigawa, Hiroki Kurita. Intracranial mycotic aneurysm rupture following cupping therapy. 05-Apr-2024;15:119. Available from: https://surgicalneurologyint.com/surgicalint-articles/12844/
Abstract
Background: Cupping therapy is an alternative treatment that uses a small glass cup to suck the skin with a needle and has been used to manage skin problems and pain. However, serious complications have been reported. Herein, we describe a case of intracranial mycotic aneurysm rupture after cupping therapy.
Case Description: A 25-year-old male patient presented with a headache and fever after cupping therapy for atopic dermatitis. He was diagnosed with infective endocarditis, and antibiotic therapy was initiated. After that, he suddenly lost consciousness, and head imaging revealed a cerebral hemorrhage due to a ruptured intracranial mycotic aneurysm. He underwent craniotomy, which was successful, and he was transferred to a rehabilitation center with a modified Rankin scale score of 2 at three months post-stroke.
Conclusion: This case serves as a reminder of life-threatening infectious complication risks after cupping therapy. A patient who has a compromised skin barrier may experience serious adverse effects, especially when cupping is performed without implementing suitable infection prevention measures.
Keywords: Aneurysm rupture, Atopic dermatitis, Cerebral hemorrhage, Cupping therapy, Infective endocarditis, Mycotic aneurysm
INTRODUCTION
Cupping therapy is a traditional treatment method that uses a small round cup made of thick glass to suck the skin; when a needle is used, it is known as wet cupping. Cupping therapy is widely used as an alternative intervention in East Asian and Middle Eastern countries.[
CASE DESCRIPTION
The patient was a 25-year-old male presenting with atopic dermatitis, and wet cupping therapy was performed without disinfection to treat atopic dermatitis. Three days later, he developed a fever in the 40°C range and persistent headache. He was admitted to another hospital where meningitis was suspected, and ceftriaxone (6 g/d) was initiated. Blood cultures were positive for methicillin-sensitive Staphylococcus aureus, and echocardiography revealed vegetation at the mitral valve, with mild mitral regurgitation. He also developed hypoesthesia in the left lower limb, and magnetic resonance imaging showed multiple bilateral acute cerebral infarcts [
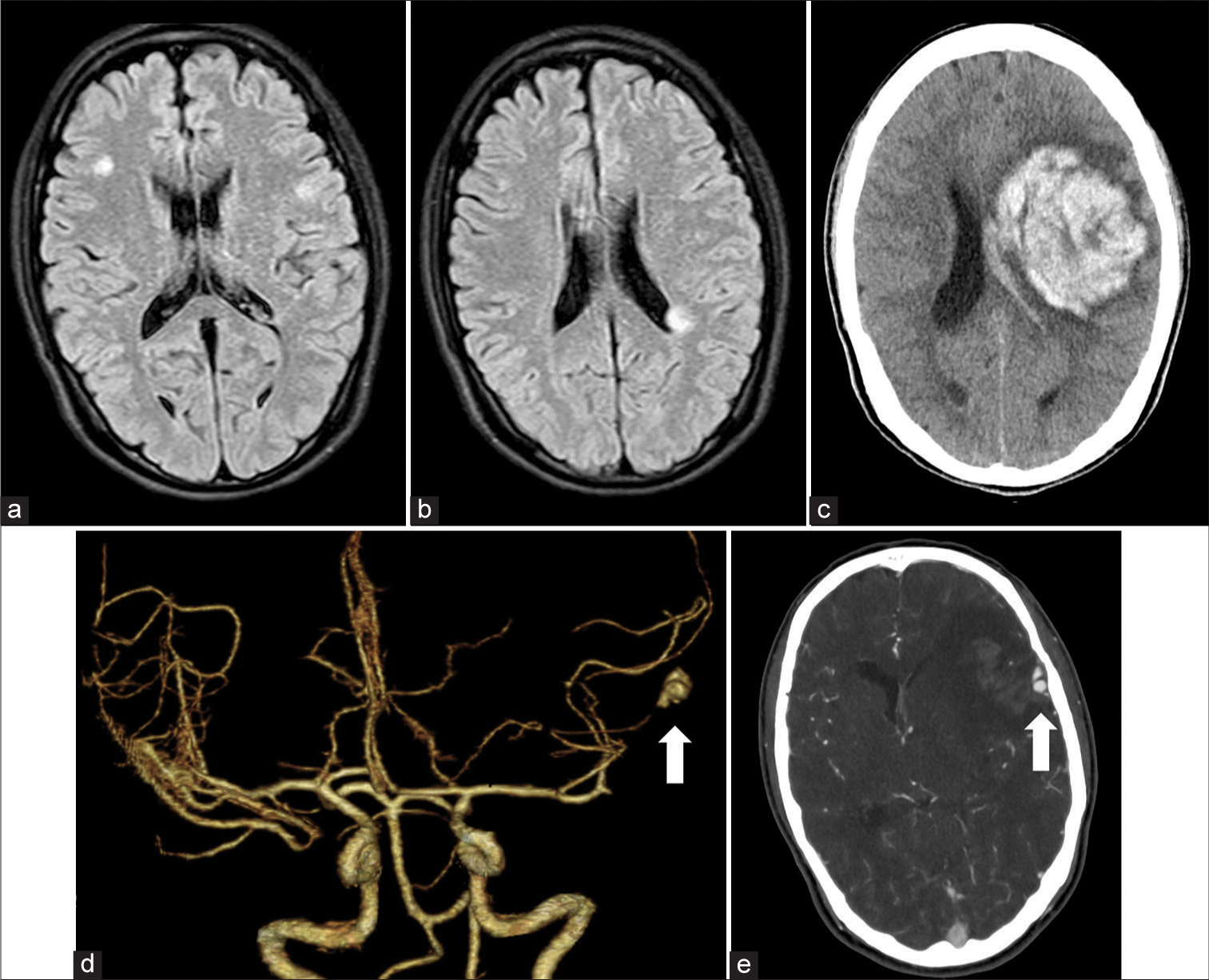
Figure 1:
(a and b) Magnetic resonance imaging revealing acute cerebral infarction in the right frontal lobe near the left lateral ventricle. (c) Computed tomography revealed an intracerebral hemorrhage in the left frontal lobe. (d) A three-dimensional computed tomography angiography image showing an aneurysm in the distal middle cerebral artery (white arrow). (e) Axial computed tomography angiography reveals bleeding from the aneurysm (white arrow).
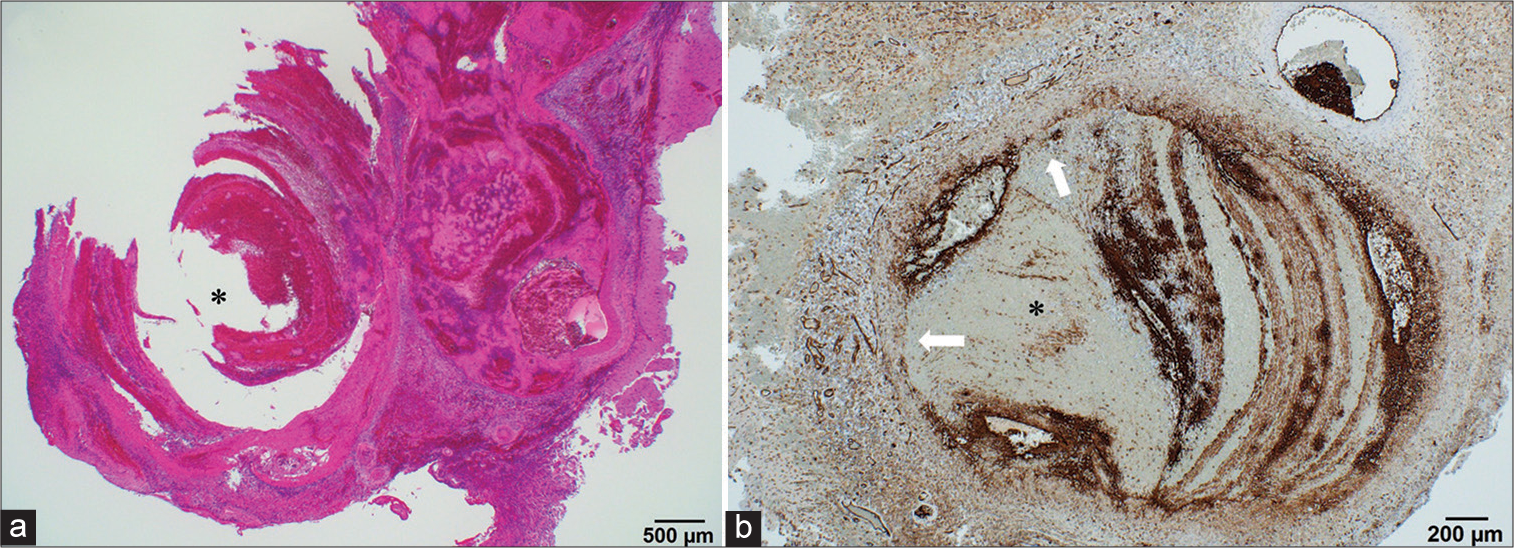
Figure 2:
(a) Hematoxylin and eosin staining revealed inflammatory cell infiltration, with partial disruption of the aneurysm wall. The endothelium is obscured, and there is neutrophilic infiltration with a hemorrhage. The asterisk indicates the intra-aneurysmal lumen. (b) Elastica van Gieson staining shows a loss of the internal elastic lamina (white arrows). The asterisk indicates the intraaneurysmal lumen.
DISCUSSION
No previous reports have described cupping therapy-induced ruptured ICMA. Given the experience of this patient, we strongly suggest raising public awareness of the infection risks of traditional therapies, such as cupping therapy, and ensuring hygiene standards are enforced at all facilities.
Cupping therapy can be classified into two main types: Dry and wet (Hijama). Dry cupping therapy uses cups to create negative pressure on the skin through suction, whereas wet cupping therapy is relatively invasive and involves scarification with needles or surgical blades before cupping therapy, such that blood is drawn into the cup. In this case, the patient had been suffering from atopic dermatitis for many years, and wet cupping was performed in unhygienic conditions. Although cupping therapy is sometimes used in patients with atopic dermatitis, its efficacy has not been confirmed.[
Cupping therapy has been reported to cause cerebrovascular diseases, including intracerebral hemorrhage, extracranial vertebral artery dissection, and cervical artery dissection.[
IE is a systemic septic disease with various clinical sequelae caused by vegetation in the valves and endocardium. Neurological complications are the most severe extracardiac complications and occur in 15–20% of patients with IE, with ICMA being relatively rare, accounting for <10% of IE neurological complications.[
In patients with atopic dermatitis, more than 90% of skin lesions show colony formation by S. aureus due to an inadequate expression of antibacterial, antifungal, and antiviral peptides that are otherwise induced by inflammation.[
CONCLUSION
We report a case of a patient with an intracranial hemorrhage due to the rupture of an ICMA after cupping therapy. Cupping therapy should be performed at facilities that follow hospital-grade disinfection protocols. Patients should be followed up post-treatment to ensure good outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alajmi T, Aljulaihim A, Alzahrani M, Aljuhayyiam S. Necrotizing fasciitis following wet cupping: A case report. Cureus. 2021. 13: e14039
2. Aoyagi S, Oda T, Wada K, Nakamura E, Kosuga T, Yasunaga H. Infective endocarditis associated with atopic dermatitis. Int Heart J. 2018. 59: 420-3
3. Blunt SB, Lee HP. Can traditional “cupping” treatment cause a stroke?. Med Hypotheses. 2010. 74: 945-9
4. Cao H, Li X, Liu J. An updated review of the efficacy of cupping therapy. PLoS One. 2012. 7: e31793
5. Chen J, Lu S, Hu K, Yang Z, Pan S, Hong T. Clinical characteristics and surgical treatment of infective endocarditis with bicuspid aortic valve. Int Heart J. 2017. 58: 220-4
6. Choi JY, Huh CW, Choi CH, Lee JI. Extracranial vertebral artery rupture likely secondary to “cupping therapy” superimposed on spontaneous dissection. Interv Neuroradiol. 2016. 22: 728-31
7. Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M. Trends in alternative medicine use in the United States, 1990-1997: Results of a follow-up national survey. JAMA. 1998. 280: 1569-75
8. El Hasbani G, Jawad A, Uthman I. Septic arthritis of the knee caused by cupping (Hijama). J R Coll Physicians Edinb. 2020. 50: 58-9
9. Hon KL, Luk DC, Leong KF, Leung AK. Cupping therapy may be harmful for eczema: A PubMed search. Case Rep Pediatr. 2013. 2013: 605829
10. Kannoth S, Thomas SV. Intracranial microbial aneurysm (infectious aneurysm): Current options for diagnosis and management. Neurocrit Care. 2009. 11: 120-9
11. Novy E, Sonneville R, Mazighi M, Klein IF, Mariotte E, Mourvillier B. Neurological complications of infective endocarditis: New breakthroughs in diagnosis and management. Med Mal Infect. 2013. 43: 443-50
12. Wang YY, Fan HW, Huang XM, Jiao Y. Disseminated Staphylococcus aureus infection after scarification wet cupping therapy: A case report and literature review. BMC Complement Med Ther. 2023. 23: 94
13. Zuhorn F, Schabitz WR, Oelschlager C, Klingebiel R, Rogalewski A. Cervical artery dissection caused by electrical cupping therapy with high-negative pressure-case report. J Stroke Cerebrovasc Dis. 2020. 29: 105207