- Department of Neurosurgery, São José do Rio Preto Medical Faculty, São José do Rio Preto, São Paulo, Brazil.
DOI:10.25259/SNI_452_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Raysa Moreira Aprígio, Ricardo Lourenço Caramanti, Felipe Oliveira Rodrigues Santos, Isabela Pinho Tigre Maia, Fernando Manuel Rana Filipe, Dionei Freitas de Moraes, Eduardo Carlos da Silva, Fabiano Morais Nogueira. Intradural disc herniation at the L1–L2 level: A case report and literature review. 11-Oct-2019;10:196
How to cite this URL: Raysa Moreira Aprígio, Ricardo Lourenço Caramanti, Felipe Oliveira Rodrigues Santos, Isabela Pinho Tigre Maia, Fernando Manuel Rana Filipe, Dionei Freitas de Moraes, Eduardo Carlos da Silva, Fabiano Morais Nogueira. Intradural disc herniation at the L1–L2 level: A case report and literature review. 11-Oct-2019;10:196. Available from: http://surgicalneurologyint.com/surgicalint-articles/9700/
Abstract
Background: Why are intradural disc herniations (IDHs) (0.3% of all discs) so infrequent? One explanation has been the marked adherence of the posterior longitudinal ligament (PLL) to the ventral wall of the dura. Variability in symptoms and difficulty in interpreting magnetic resonance (MR) images with/without contrast make the diagnosis of an IDH difficult. Here, we reported a patient with an L1–L2 IDH and appropriately reviewed the relevant literature.
Case Description: A 57-year-old male presented with chronic low back and 1 month’s duration of the left thigh pain. The lumbar MR with/without contrast demonstrated an IDH at the L1–L2 level, resulting in spinal cord compression. At surgery, the disc herniation was appropriately resected, the dura was closed, and an interbody fusion with pedicle screw fixation was performed. Postoperatively, the patient clinically improved.
Conclusion: IDHs are rare, being seen in only 0.3% of all cases. MR findings, performed with/without contrast, may help signal the presence of an IDH. MR findings include a hypointense structure inside the dura; the “hawk beak” sign (e.g., beak-like mass with ring enhancement at the intervertebral disc space); the Y sign (e.g., ventral dura split into ventral dura and arachnoid by disc material); an abrupt loss of continuity of the PLL; a diffuse annular bulge with a large posterocentral extrusion; and an typical crumbled appearance of disc (e.g., “crumble disc sign”). At surgery, both the extradural and intradural components of the disc must be excised.
Keywords: Intradural disc herniation, Intradural lumbar disc herniation, Lumbar discectomy
INTRODUCTION
Intradural disc herniations (IDHs) represent between 0.26% and 0.30% of all discs, and 92% occur in the lower lumbar spine, mostly at the L4–L5 level. Patients are typically males in their fifties who experience the acute exacerbation of low back pain accompanied by the rapid onset of a focal motor deficit. Although preoperative magnetic resonance (MR) studies performed with/without contrast may demonstrate the level of the disc herniation and its potential intradural location, only intraoperative findings confirm an intradural disc extrusion.[
CASE REPORT
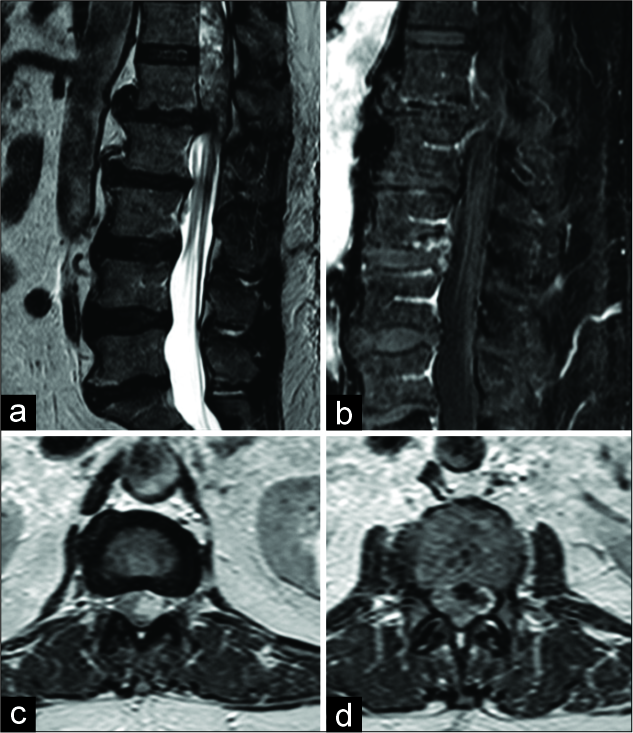
A 57-year-old male presented with chronic low back pain, and 1-month’s duration of the acute onset of the left thigh pain with weakness (4/5), and absent bilateral patellar, and a left-sided Achilles response. The lumbar magnetic resonance imaging (MRI) performed with/without contrast showed an extradural/intradural L1–L2 disc herniation (e.g., showing a “hawksbill” and other signs), resulting in significant spinal cord compression [
Figure 1:
(a) Magnetic resonance imaging (MRI) in the sagittal T2 sequence showing disc herniation L1–L2 associated superiorly heterogeneous irregular image. (b) MRI in the sagittal T1 gadolinium sequence showing herniated disc contrast enhancement in generating image “hawksbill.” (c) MRI axial T2 sequence with irregular hyperintense left image promoting spinal cord compression. (d) MRI axial T1 sequence with gadolinium irregular impregnation of the herniated content.
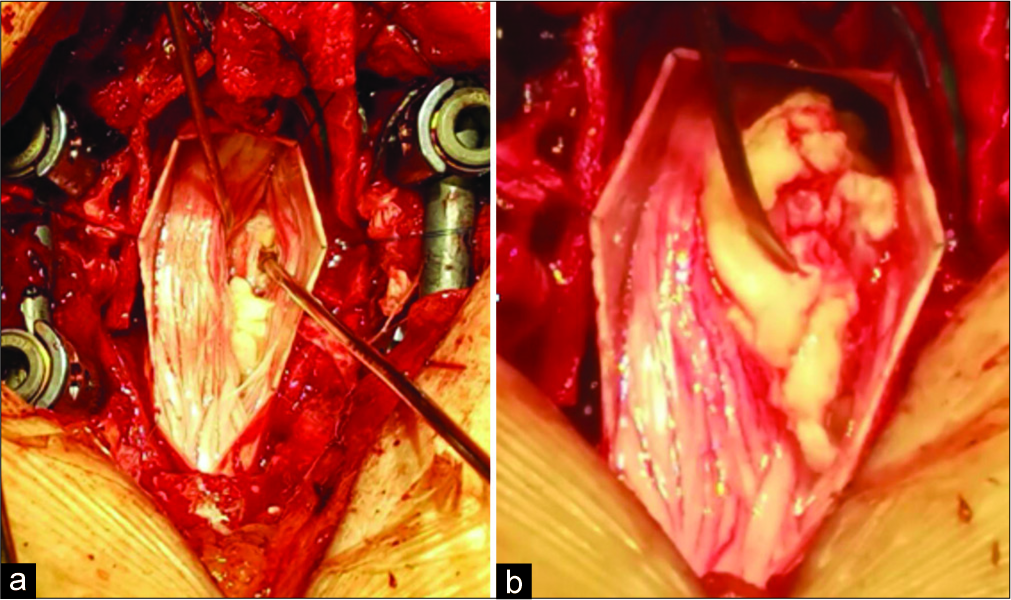
Surgery included an L1–L2 microdiscectomy. At surgery, the disc was located both extradurally and intradurally. After disc resection, the dura was sutured closed, an interbody cage was placed, and segmental pedicle screws fixation/fusion was performed. Postoperatively, the patient uneventfully recovered [
DISCUSSION
In 1942, Dandy published the first case of an intradural herniated disc. Since then, less than 124 cases have been reported in literature. Approximately 0.26–0.30% of all disc herniations are intradural and are, respectively, located in the cervical (3% of cases), thoracic (5%), and lumbar (92%) regions (i.e., L4–L5 (55%), L3–L4 (16%), L5–S1 (10%), and rare cases L1–L2 and L2–L3).[
Symptoms of intradural discs
Symptoms of intradural discs typically include chronic low back followed by acute exacerbation of leg pain and/or motor deficits/cauda equina syndromes. Arnold and Wakwaya, in 2011, reported two cases of IDHs at the L1–L2 level, where patients experienced the abrupt worsening of back/leg pain and paresthesias.[
Pathophysiology
There are two pathophysiological mechanisms for the formation of IDHs. First, they are most likely attributable to adhesions between the posterior longitudinal ligament (PLL), fibrous annulus, and the dural sac; a hole generated through the dura then allows for intradural disc migration.[
MR findings of IDHs
MRI with/without contrast is a method of choice for documenting IDH. Findings include discontinuity of the PLL at the disc entry site/dural sac, variable contrast enhancement of the herniated disc, and the Hawk nozzle signal (e.g., annulus enhancement in the intervertebral space).[
Treatment of IDHs
The treatment of IDHs is based on the removal of the extradural and intradural disc components, followed by suturing the dura mater (e.g., often ventral), without fusion as needed.[
CONCLUSION
IDHs are rare and are typically associated with the sudden onset of acute exacerbation of low back pain and new motor deficits. Utilizing MR with/without contrast, they may be appropriate diagnosed and treated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Andrea GD, Trillo G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural disc herniations: The role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev. 2004. 27: 75-80
2. Arnold PM, Wakwaya YT. Intradural disk herniation at L1-L2 Report of two cases. J Spinal Cord Med. 2011. 34: 312-4
3. Dandy WE. Serious complications of ruptured intervertebral discs. J Am Med Assoc. 1942. 119: 474-5
4. Görgülü A, Karaaslan T, Tural O. Intradural and intraradicular lumbar disk herniations: Case report and review of the literature. J Neurol Sci. 2004. 21: 4-
5. Klopfenstein J, Han PP, Kim L, Spetzler RF. Herniated lumbar disc sequestered between the internal and external dural sleeves: Case report. Barrow Q. 2003. 19: 25-7
6. Lesoin F, Duquennoy B, Rousseaux M, Servato R, Jomin M. Intradural rupture of lumbar intervertebral disc: Report of three cases with review of the literature. Neurosurgery. 1984. 14: 728-31
7. Mut M, Berker M, Palaoğlu S. Intraradicular disc herniations in the lumbar spine and a new classification of intradural disc herniations. Spinal Cord. 2001. 39: 545-8
8. Negovetić L, Cerina V, Sajko T, Glavić Z. Intradural disc herniation at the T1-T2 level. Croat Med J. 2001. 42: 193-5
9. Oztürk A, Avci E, Yazgan P, Torun F, Yücetaş S, Karabağ H. Intradural herniation of intervertebral disc at the level of lumbar 1-lumbar 2. Turk Neurosurg. 2007. 17: 134-7
10. Rodrigo V, Claramonte M, Martín M, Calatayud JB. Intradural disc herniation: How I do it. Acta Neurochir (Wien). 2018. 160: 945-7
11. Sharma A, Singh V, Sangondimath G, Kamble P. Intradural disc a diagnostic dilemma: Case series and review of literature. Asian J Neurosurg. 2018. 13: 1033-6
12. Wasserstrom R, Mamourian AC, Black JF, Lehman RA. Intradural lumbar disk fragment with ring enhancement on MR. AJNR Am J Neuroradiol. 1993. 14: 401-4
13. Whittaker CK, Bernhardt M. Magnetic resonance imaging shows gadolinium enhancement of intradural herniated disc. Spine (Phila Pa 1976). 1994. 19: 1505-7
14. Yang HS, Oh YM, Eun JP. Cervical intradural disc herniation causing progressive quadriparesis after spinal manipulation therapy: A Case report and literature review. Medicine (Baltimore). 2016. 95: e2797-
15. Yildizhan A, Paşaoğlu A, Okten T, Ekinci N, Aycan K, Aral O. Intradural disc herniations pathogenesis, clinical picture, diagnosis and treatment. Acta Neurochir (Wien). 1991. 110: 160-5