- School of Medicine, University of Texas Rio Grande Valley, Edinburg, Texas, United States.
- Department of Surgery, University of Texas Rio Grande Valley, Edinburg, Texas, United States.
Correspondence Address:
Fabiola Valenzuela
Department of Surgery, University of Texas Rio Grande Valley, Edinburg, Texas, United States.
DOI:10.25259/SNI_743_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fabiola Valenzuela1, Sohum Desai2. Intradural Extramedullary Primary Central Nervous System Melanoma of the Craniovertebral Junction during Pregnancy: Observations and Outcomes. 03-May-2021;12:198
How to cite this URL: Fabiola Valenzuela1, Sohum Desai2. Intradural Extramedullary Primary Central Nervous System Melanoma of the Craniovertebral Junction during Pregnancy: Observations and Outcomes. 03-May-2021;12:198. Available from: https://surgicalneurologyint.com/surgicalint-articles/10785/
Abstract
Background: Primary central nervous system (CNS) melanoma is a rare lesion derived from neural crest precursors. While its management is analogous to metastatic spinal melanoma, the literature does not describe this entity clearly in pregnant patients and the unique implications it presents. Here, we describe the case of a pregnant patient who presented with primary CNS melanoma of the cervical spine.
Case Description: A 27-year-old pregnant patient presented with a 3-month history of neck and interscapular pain. MRI of the cervical spine demonstrated a ventral intradural extramedullary mass adjacent to the C2-C3 vertebral bodies causing severe cord compression. The patient was induced at 31 weeks and shortly thereafter developed quadriparesis and became obtunded. The patient underwent emergent right-sided C1 hemilaminectomy, complete C2-C4 laminectomy, and right-sided intradural division of the dentate ligaments for removal of the ventral intradural mass. Full neurological recovery was achieved before discharge. At follow-up, the infant was found to be negative for transplacental metastasis. We performed fractionated radiotherapy 4 weeks after index surgery. Nine months following index surgery, she presented with severe axial neck pain. Radiographs of the cervical spine demonstrated postlaminectomy kyphosis. The patient later underwent a posterior cervical fusion. She was recurrence-free 9 months follow-up.
Conclusion: The differential for intradural extramedullary spinal lesions should include schwannoma, neurofibroma, meningioma, metastasis, and melanoma. Physicians caring for pregnant patients with melanoma should be aware of the potential for transplacental metastasis and perform follow-up for fetal complications.
Keywords: Management, Melanoma, Pregnancy, Spine, Tumor
INTRODUCTION
Primary central nervous system (CNS) melanocytic tumors are well-recognized in the World Health Organization (WHO) classification, consisting of diffuse leptomeningeal melanosis, melanomatosis, melanocytoma, and primary CNS melanoma.[
CASE PRESENTATION
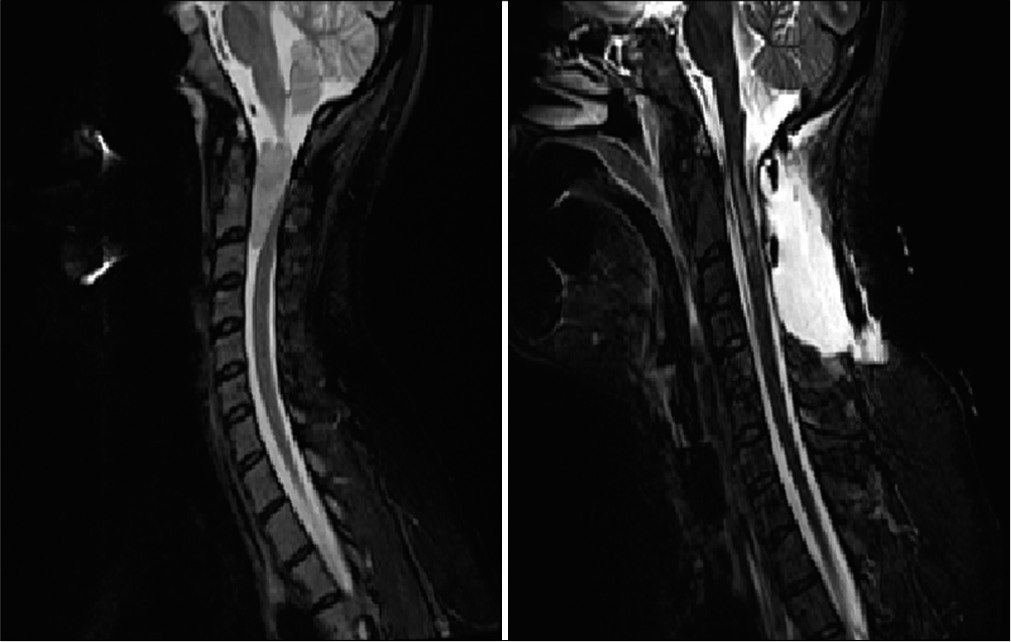
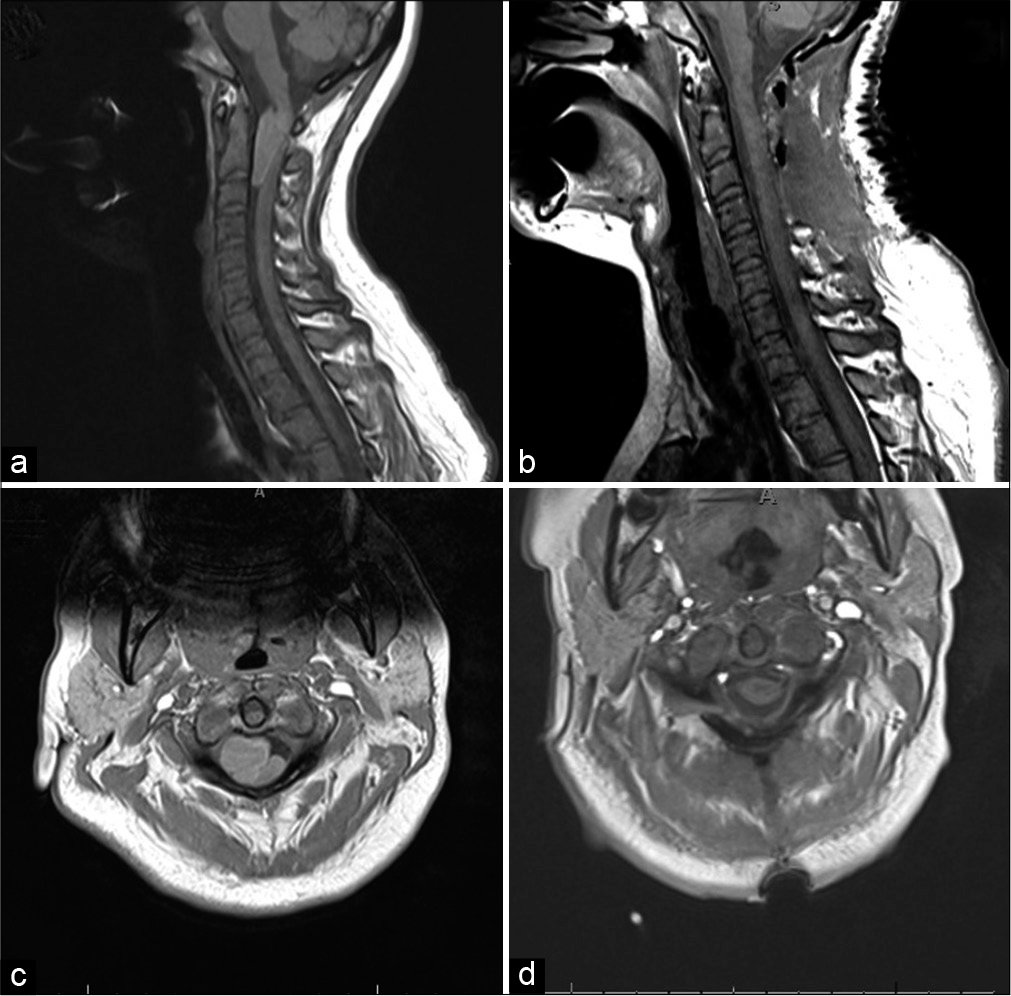
A 27-year-old pregnant patient presented with a 4-month period of neck and shoulder pain, with paresthesia radiating to the upper extremities bilaterally. Postcontrast MRI of the cervical spine revealed an enhancing intradural extramedullary lesion in the cervical spine. The lesion spanned adjacent from vertebral bodies of C1-C3 causing severe compression with kinking at the level of the C1-C2 foramen [
Figure 1:
Preoperative T2-weighted noncontrast MRI (left) of an isointense intradural extramedullary lesion extending from the level of C1-C2 measuring 1.5 × 1.6 × 3.5 cm (TV × AP × CC), causing severe mass effect and signal changes in the spinal cord. Postoperative T2-weighted noncontrast MRI (right) after C1-C3 laminectomy with revision and posterior arch of C1 resection. No evidence of residual mass or abnormal enhancement is seen. The spinal cord has significantly reexpanded with hyperintensity noted within the cord.
At 31 weeks of gestation, the patient’s condition worsened with muscle spasms of the left upper and lower extremities and generalized headache. The obstetrician decided to deliver the baby by an emergency cesarean section which proceeded without complication. The placenta was inspected grossly for abnormalities and disposed of.
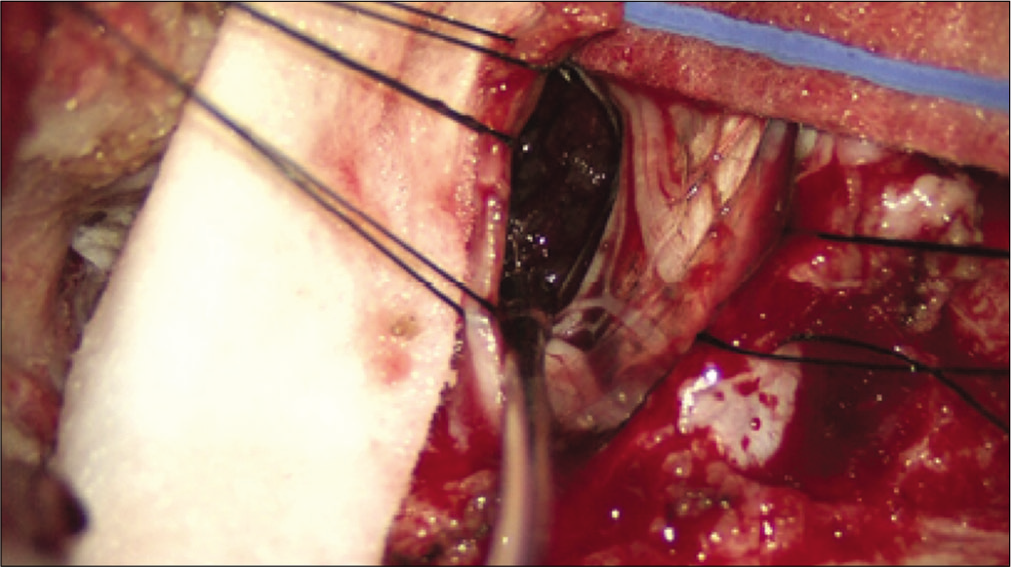
The patient developed worsening of pain hours following cesarean section, with new-onset quadriparesis. Emergent posterior decompressive laminectomy for resection of the mass was performed. A posterior midline approach was used to expose the occiput to C5. Next, the vertebral artery was mobilized off the sulcus of C1 to facilitate a wide right-sided laminectomy at that level. A C2-C4 laminectomy was performed taking care to remove the medial aspect of facet joints to facilitate exposure. Taking into consideration the tumor borders, hemorrhage, and emergent nature of the case, we felt that a C2-C4 laminectomy was necessary for safe resection of the tumor. The dura of the cervical spine was opened to the right of the midline to access the mass. The dentate ligaments were cut distal to their attachment to the cord. Gentle countertraction was applied to improve the visualization of the ventrally located mass. The mass was removed in a piecemeal fashion under the microscope [
Examination following surgery revealed intact sensation without improvement of muscle strength. She could communicate and respond to commands through blinking. By the following morning, the patient was breathing spontaneously on the ventilator and tolerated continuous positive airway pressure mode. She slowly began improving and regained strength with a return to baseline by postoperative day 4. The patient was discharged 1 week later with her child and was ambulating independently. Her only deficit was numbness in the posterior occiput consistent with occipital neuralgia.
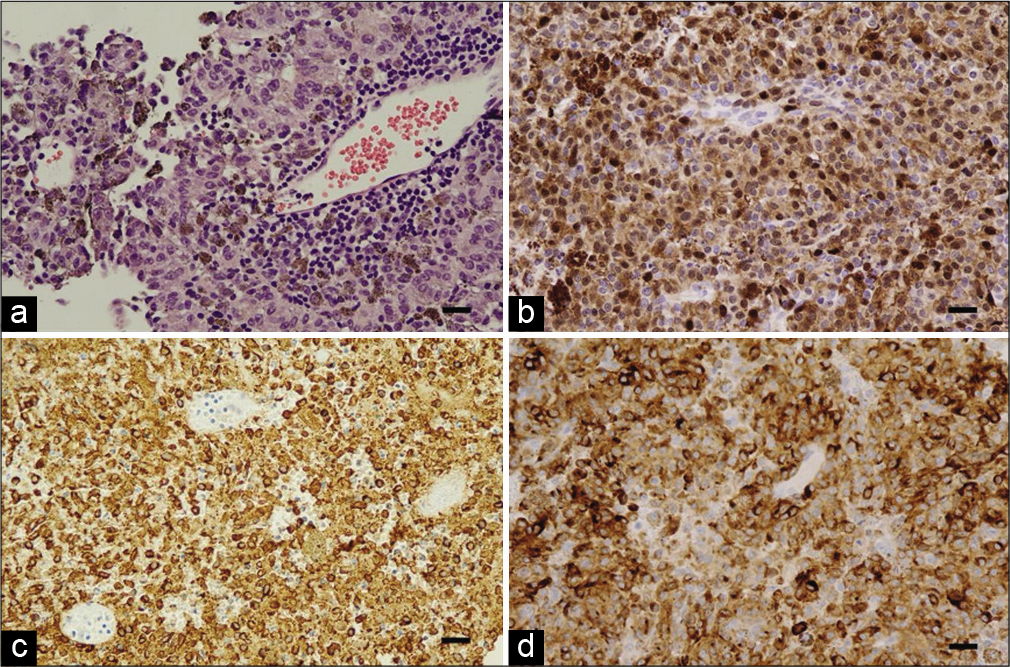
This lesion met the definition of primary melanoma of the CNS as set forth by the WHO guidelines.[
Figure 4:
Immunohistochemistry. Hematoxylin and eosin (H and E) stained section reveals a tumor whose cells have ample pale, vacuolated cytoplasm and large pleomorphic nuclei with prominent nucleoli. Some tumor cells contain melanin pigment, and lymphocytic reaction is visible around a small venule (a). Immunohistochemical stains for S-100 (b), HMB-45 (c), and MelanA/MART1 (d). Confirmation of the melanocytic origin of the neoplasm. Scale bars in all panels represent 25 micrometers.
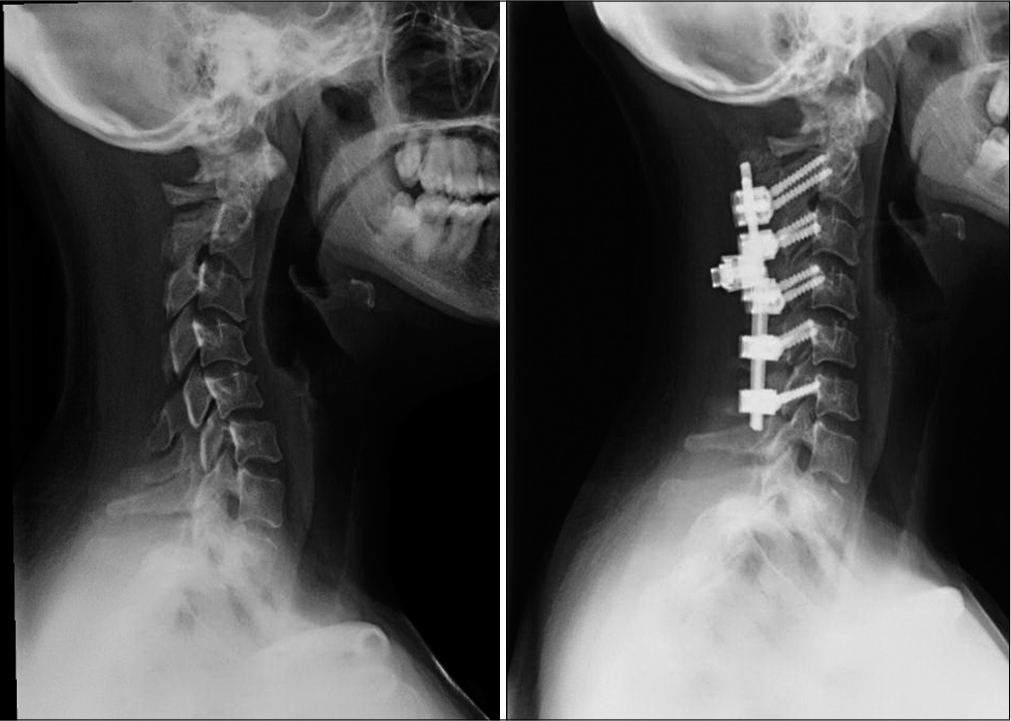
The patient was recurrence free on MRI at 6 months follow-up. At 9-month postoperatively, she complained of severe neck pain without any radicular pain or weakness. The X-ray revealed postlaminectomy kyphosis [
DISCUSSION
We have presented the rare case of a pregnant patient that presented with acute cervical myelopathy secondary to a craniocervical junction meningeal melanoma. We have also highlighted the implications related to pregnancy and delivery. One unique aspect of this case is that it presents excellent recapitulation of the neural crest origin of melanocytes. The melanoma in this case most likely arose from the dura, later becoming intradural and impinged on surrounding structures causing nonspecific symptoms seen early in the case.
Another observation we have made in retrospection is that the placenta should be retained for pathological examination. This is especially relevant in cases where a concurrent cancer diagnosis, such as melanoma, is present or on the differential for a pregnant patient. The case was followed well after the birth of the neonate and the authors are relieved the neonate did not suffer any complications from metastasis of the melanoma or due to intervention. The potential for transplacental metastasis to a fetus in pregnant patients with melanoma has been documented. This highlights the importance of pathological examination of the placenta to assess the risk of such a complication.[
It is important to weigh the risks associated with the resection of a large spinal tumor, particularly that of long-term spine destabilization. In this case, we felt that optimal resection was important. We believe that it is of great importance to obtain adequate follow-up surveillance imaging for disease recurrence. If postlaminectomy kyphosis is present, it can then be addressed at a second operative session to optimize stability.
CONCLUSION
We present a unique case of primary CNS melanoma in a pregnant patient. Physicians caring for such patients should be aware of the possibility of metastasis to the fetus through the placenta. It is important to assess for this complication through pathologic examination of the placenta.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Altman JF, Lowe L, Redman B, Esper P, Schwartz JL, Johnson TM. Placental metastasis of maternal melanoma. J Am Acad Dermatol. 2003. 49: 1150-4
2. Buckner JC, Brown PD, O’Neill BP, Meyer FB, Wetmore CJ, Uhm JH. Central nervous system tumors. Mayo Clin Proc. 2007. 82: 1271-86
3. Farrokh D, Fransen P, Faverly D. MR findings of a primary intramedullary malignant melanoma: Case report and literature review. AJNR Am J Neuroradiol. 2001. 22: 1864-6
4. Hayward RD. Malignant melanoma and the central nervous system. A guide for classification based on the clinical findings. J Neurol Neurosurg Psychiatry. 1976. 39: 526-30
5. Holland E. A case of transplacental metastasis of malignant melanoma from mother to foetus. J Obstet Gynaecol Br Emp. 1949. 56: 529-36
6. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007. 114: 97-109
7. Wadasadawala T, Trivedi S, Gupta T, Epari S, Jalali R. The diagnostic dilemma of primary central nervous system melanoma. J Clin Neurosci. 2010. 17: 1014-7