- Department of Neurosurgery, Specialties Hospital, La Raza National Medical Center, Mexican Social Security Institute, Mexico City, Mexico.
- Department of Spine Surgery, Angeles del Pedregal Hospital, Mexico City, Mexico.
Correspondence Address:
Héctor Alonso Tirado-Ornelas, Department of Neurosurgery, Specialties Hospital, La Raza National Medical Center, Mexican Social Security Institute, Mexico City, Mexico.
DOI:10.25259/SNI_525_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Héctor Alonso Tirado-Ornelas1, Jorge Luis Olivares-Peña1, Jorge Luis Olivares-Camacho2, Jorge Arturo Santos-Franco1, Maurilio Vicente Ochoa-González1. Intramedullary cervical spinal cord and cerebellar hemangioblastoma: A case report. 08-Jul-2022;13:294
How to cite this URL: Héctor Alonso Tirado-Ornelas1, Jorge Luis Olivares-Peña1, Jorge Luis Olivares-Camacho2, Jorge Arturo Santos-Franco1, Maurilio Vicente Ochoa-González1. Intramedullary cervical spinal cord and cerebellar hemangioblastoma: A case report. 08-Jul-2022;13:294. Available from: https://surgicalneurologyint.com/surgicalint-articles/11705/
Abstract
Background: Hemangioblastomas are benign tumors that develop in the central nervous system. They represent 1.5–2.5% of all intracranial tumors, and about 2–15% of all spinal cord tumors. They are highly associated with von Hippel–Lindau disease.
Case Description: A 36-year-old female presented with a 4-year history of progressive right upper extremity distal weakness and cervical pain. The magnetic resonance imaging demonstrated a homogeneously, contrast enhancing intradural/intramedullary tumor at C6–C7 with perilesional edema and a syrinx accompanied by a cerebellar cyst with a mural nodule. Surgery included excision of the spinal lesion and decompression and excision of the cerebellar cyst and mural nodule (i.e., median suboccipital craniectomy and cervical C5–C7 laminectomy).
Conclusion: Surgery is the gold standard treatment for symptomatic hemangioblastomas, and surgical approaches should minimize risk.
Keywords: Hemangioblastoma, Neurosurgery, Spine surgery, Spine, von Hippel-Lindau
INTRODUCTION
Hemangioblastomas are histologically benign tumors that develop in the central nervous system. They represent 1.5–2.5% of all intracranial tumors, where they are most often found is the posterior fossa (7–12%).[
CASE REPORT
Clinical presentation
A 36-year-old female presented with a 4-year history of progressive right upper extremity distal weakness and cervical pain. On examination, she exhibited hypoesthesia in both upper extremities accompanied by a hemispheric cerebellar syndrome and hyperreflexia. A family history of von Hippel–Lindau disease was ruled out.
Magnetic resonance imaging (MRI)
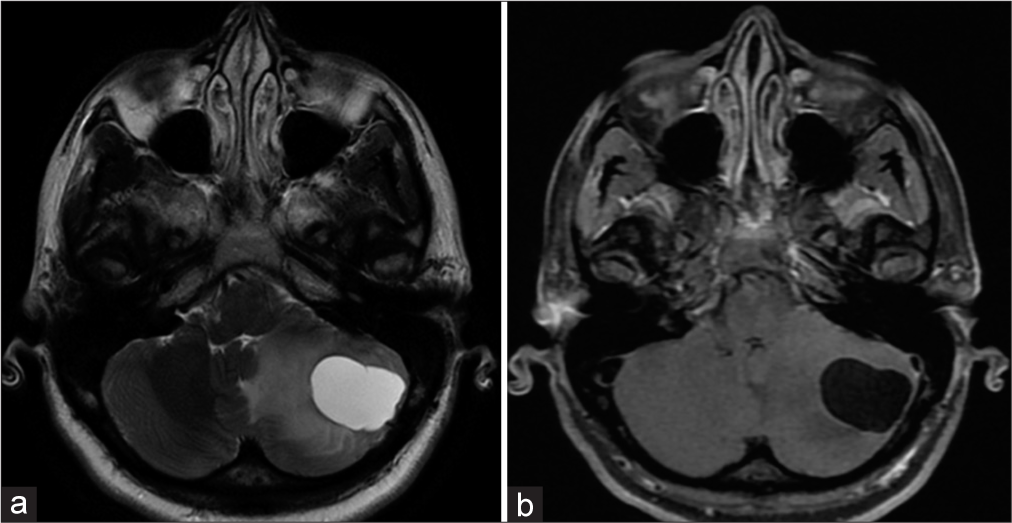
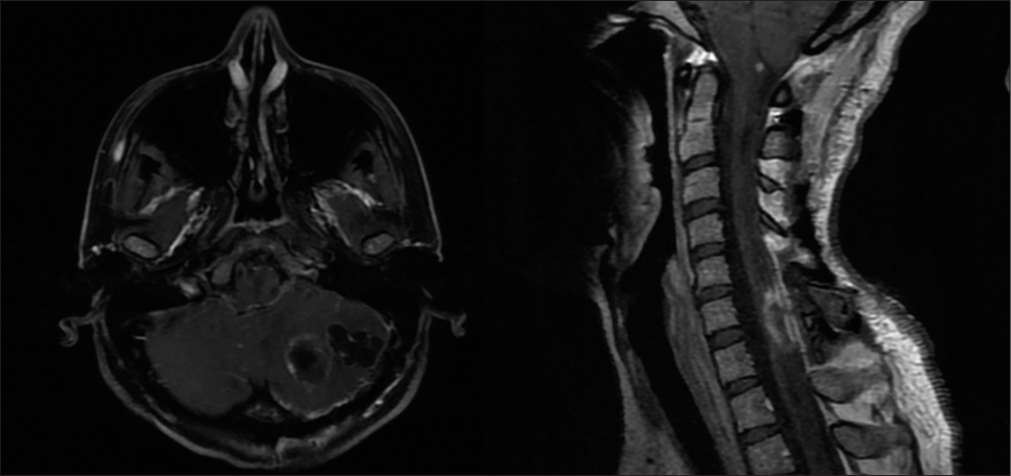
The MRI demonstrated a cerebellar cyst with a mural nodule [
Surgery
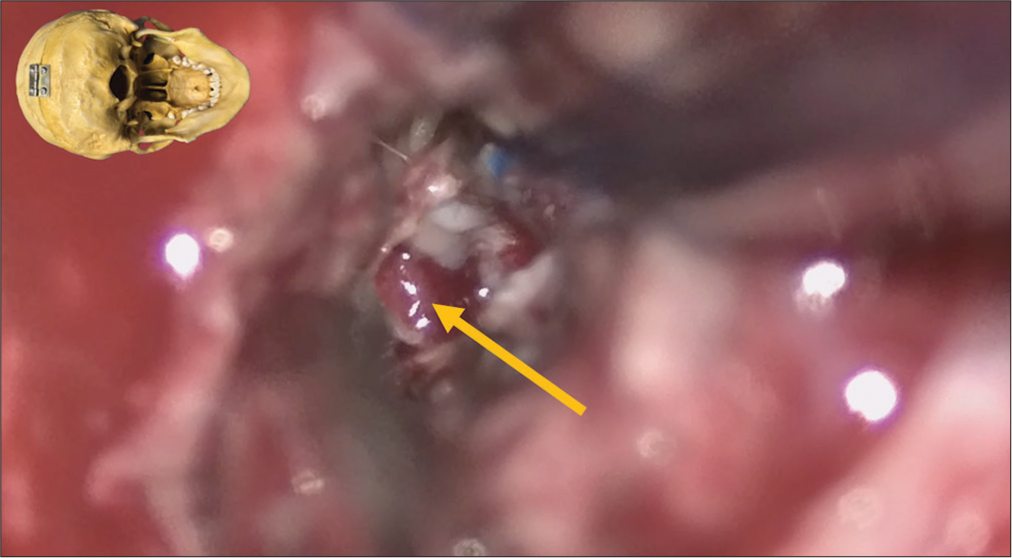
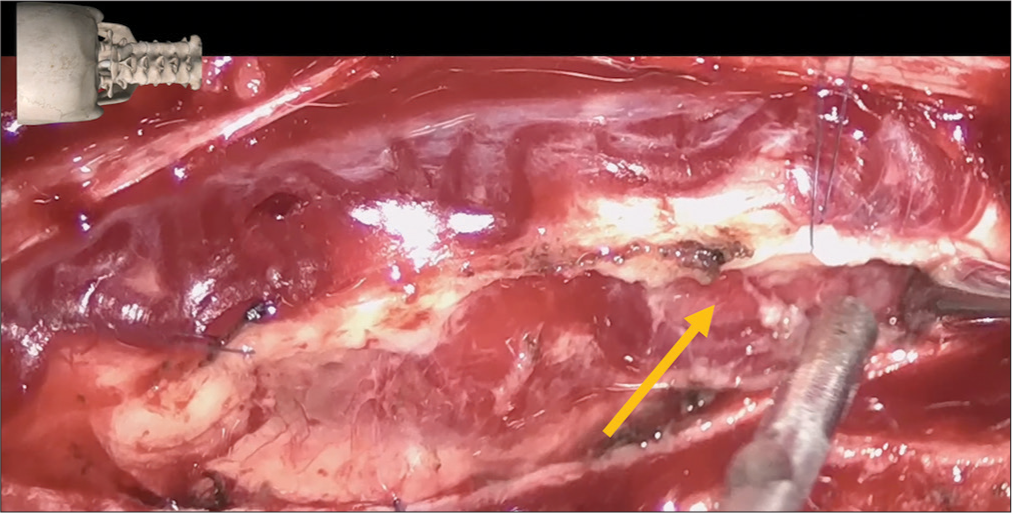
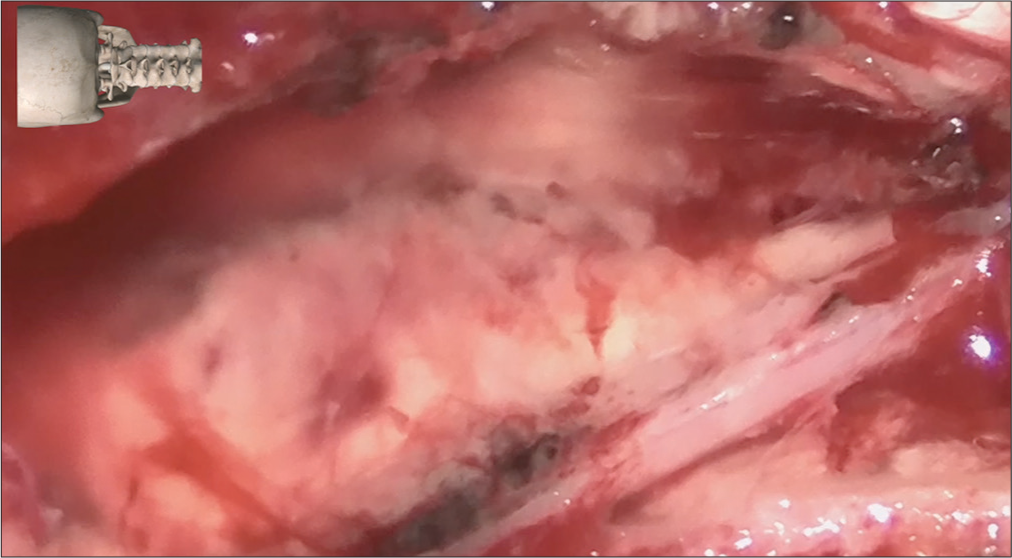
The patient underwent tumor resection through a median suboccipital craniectomy for the cerebellar lesion [
DISCUSSION
Surgical resection offers definitive therapy for sporadic, isolated hemangioblastomas, particularly those arising in the cerebellum. The role of surgery in patients with von Hippel–Lindau disease is less well-defined due to the frequent occurrence of multiple lesions. The optimal timing of surgery for patients these patients is uncertain. Most neurosurgeons do not operate these patients until they demonstrate progressive neurological deficits, tumor or cyst growth, or renewed hemorrhage. The preoperative neurologic deficit noted in this patient warranted surgical intervention that resulted in symptomatic improvement.
CONCLUSION
We reported a case of symptomatic multiple hemangioblastomas, in cerebellum and spinal cord. Complete resection of hemangioblastomas is very important to reduce the risks of lesion recurrence. This patient underwent complete resection of two symptomatic hemangioblastomas involving the cerebellum and spinal cord. In this case, the diagnosis of von Hippel–Lindau disease was confirmed by the presence of two or more central nervous system hemangioblastomas even without a positive genetic test.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Amano T, Tokunaga S, Shono T, Mizoguchi M, Matsumoto K, Yoshida F. Cerebellar haemangioblastoma manifesting as hearing disturbance. Neurol Med Chir (Tokyo). 2009. 49: 418-20
2. Kanno H, Yamamoto I, Nishikawa R, Matsutani M, Wakabayashi T, Yoshida J. Spinal cord hemangioblastomas in von Hippel-Lindau disease. Spinal Cord. 2009. 47: 447-52
3. Kuharic M, Jankovic D, Splavski B, Boop FA, Arnautovic KI. Hemangioblastomas of the posterior cranial fossa in adults: Demographics, clinical, morphologic, pathologic, surgical features, and outcomes. A systematic review. World Neurosurg. 2018. 110: e1049-62
4. Mandigo CE, Ogden AT, Angevine PD, McCormick PC. Operative management of spinal hemangioblastoma. Neurosurgery. 2009. 65: 1166-77
5. Migliorini D, Haller S, Merkler D, Pugliesi-Rinaldi A, Koka A, Schaller K. Recurrent multiple CNS hemangioblastomas with VHL disease treated with pazopanib: A case report and literature review. CNS Oncol. 2015. 4: 387-92
6. Rachinger J, Buslei R, Prell J, Strauss C. Solid haemangioblastomas of the CNS: A review of 17 consecutive cases. Neurosurg Rev. 2009. 32: 37-47