- Department of Neurological Surgery, University of Miami Miller School of Medicine, Miami, Florida, United States.
- Department of Surgery, University of Miami Miller School of Medicine, Miami, Florida, United States.
Correspondence Address:
Joseph Yunga Tigre, Department of Neurological Surgery, University of Miami Miller School of Medicine, Miami, Florida, United States.
DOI:10.25259/SNI_726_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joseph Yunga Tigre1, Aiko Puerto1, Jean-Paul Russo1, Andrew J. Kloehn1, Naaman Abdullah2, S. Shelby Burks1, Allan D. Levi1. Intraoperative embolectomy of a left illiac artery thrombus during an anterior lumbar interbody fusion. 20-Oct-2023;14:374
How to cite this URL: Joseph Yunga Tigre1, Aiko Puerto1, Jean-Paul Russo1, Andrew J. Kloehn1, Naaman Abdullah2, S. Shelby Burks1, Allan D. Levi1. Intraoperative embolectomy of a left illiac artery thrombus during an anterior lumbar interbody fusion. 20-Oct-2023;14:374. Available from: https://surgicalneurologyint.com/surgicalint-articles/12604/
Abstract
Background: Anterior lumbar interbody fusion (ALIF) offers direct midline access to the lumbar intervertebral discs utilizing an anterior retroperitoneal approach. Here, a 33-year-old female undergoing ALIF developed an acute intraoperative left iliac artery thrombus and underwent immediate successful embolectomy.
Case Description: A 33-year-old female was undergoing routine L5-S1 ALIF when an acute intraoperative left iliac vein injury occurred, requiring immediate repair by a vascular surgeon. Her left foot pulse oximeter showed a decreased reading, and her Doppler ultrasound confirmed reduced flow in the distal external iliac artery due to a thrombus. She required an immediate left iliac artery embolectomy, and flow was immediately restored. Postoperatively, she recovered well, and 3 months postoperatively, she remained neurologically intact without any further complications.
Conclusion: Using pulse oximeters in patients undergoing ALIF surgery can aid in facilitating the diagnosis and treatment of acute artery thrombi. When such vascular injuries arise, having immediate access to experienced vascular surgeons is critical to obtain expeditious treatment and optimize patient outcomes.
Keywords: Anterior lumbar interbody fusion embolectomy, Anterior lumbar interbody fusion embolus, Anterior lumbar interbody fusion vascular injury, Anterior lumbar interbody fusion vessel injury
INTRODUCTION
The anterior vasculature, subcutaneous tissue, and visceral organs are placed at risk with anterior lumbar interbody fusions (ALIFs).[
CASE PRESENTATION
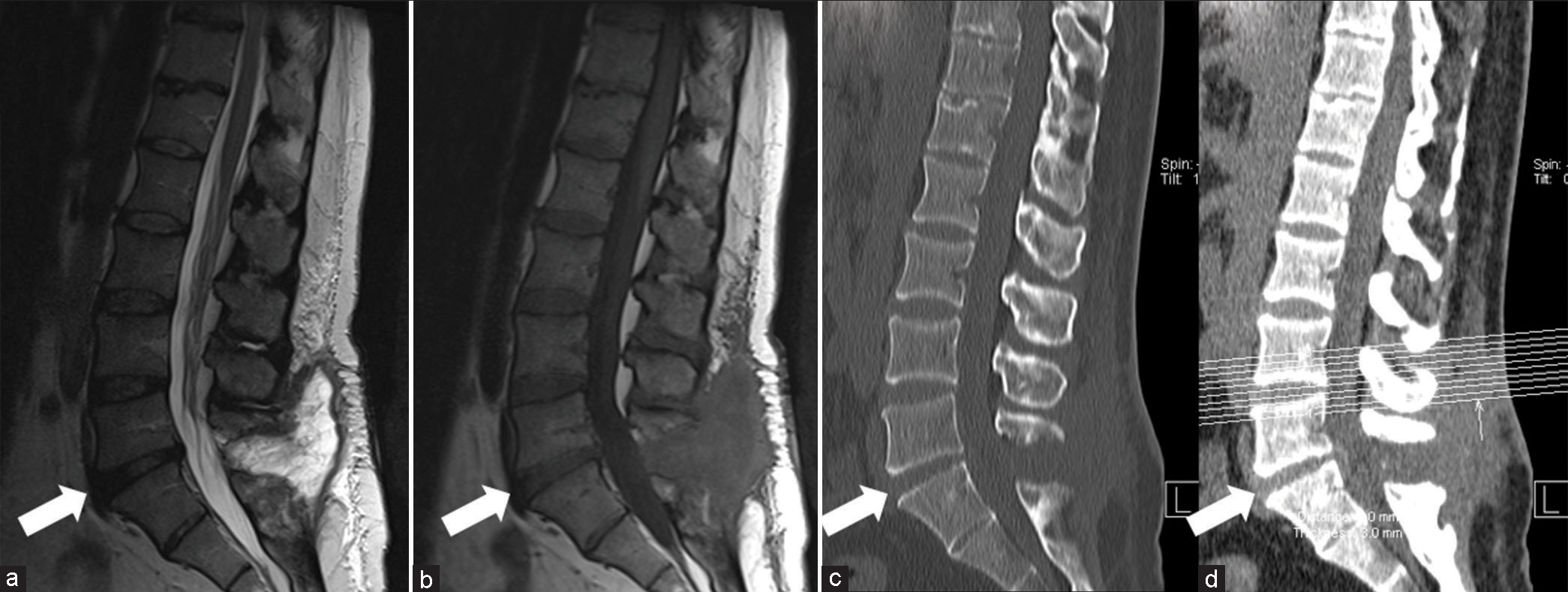
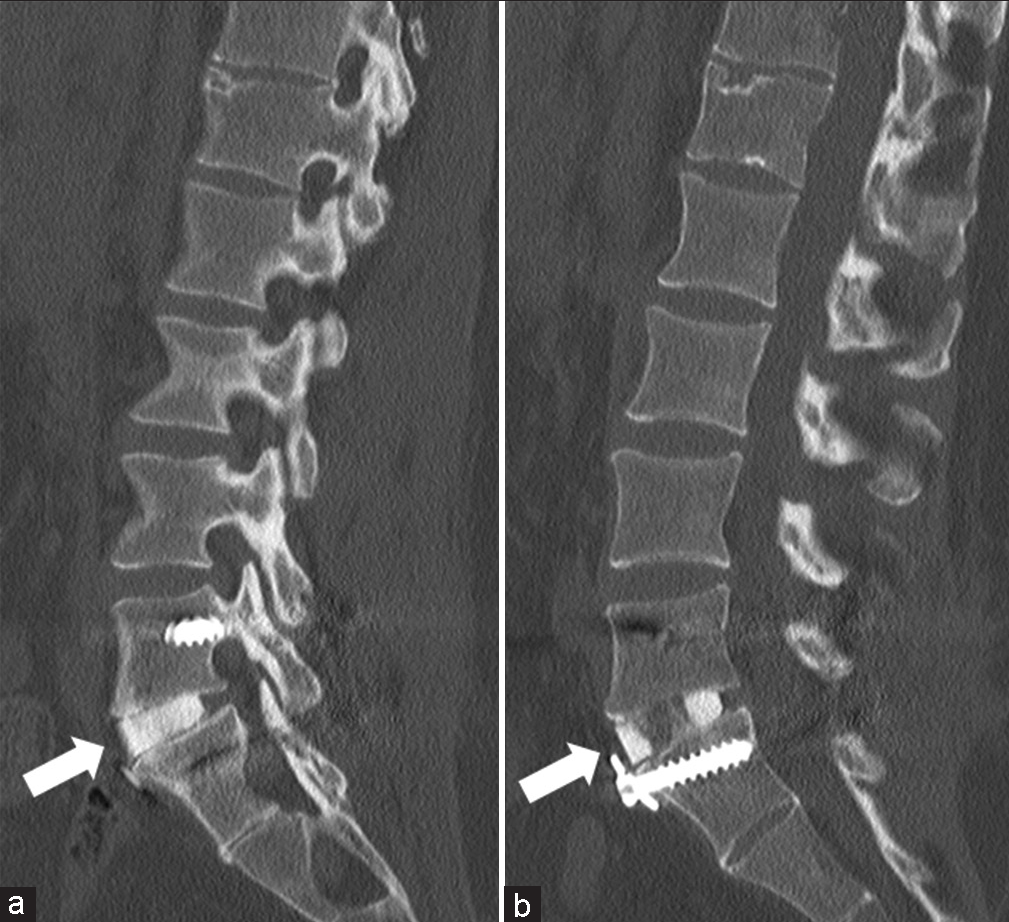
A 33-year-old, right-handed female presented for continued follow-up due to worsening low back pain despite two previous lumbar surgeries. X-rays, computed tomography (CT), and magnetic resonance imaging (MRI) showed evidence of her prior bilateral L5 laminectomy and L5-S1 disc space narrowing [
Figure 1:
Preoperative imaging. Preoperative lumbar imaging demonstrating prior bilateral L5 laminectomy and L5-S1 disc space narrowing (white arrow). (a) is a sagittal T2-weighted magnetic resonance imaging (MRI) and (b) is a sagittal T1-weighted MRI. (c and d) are sagittal lumbar computed tomography images.
Intervention
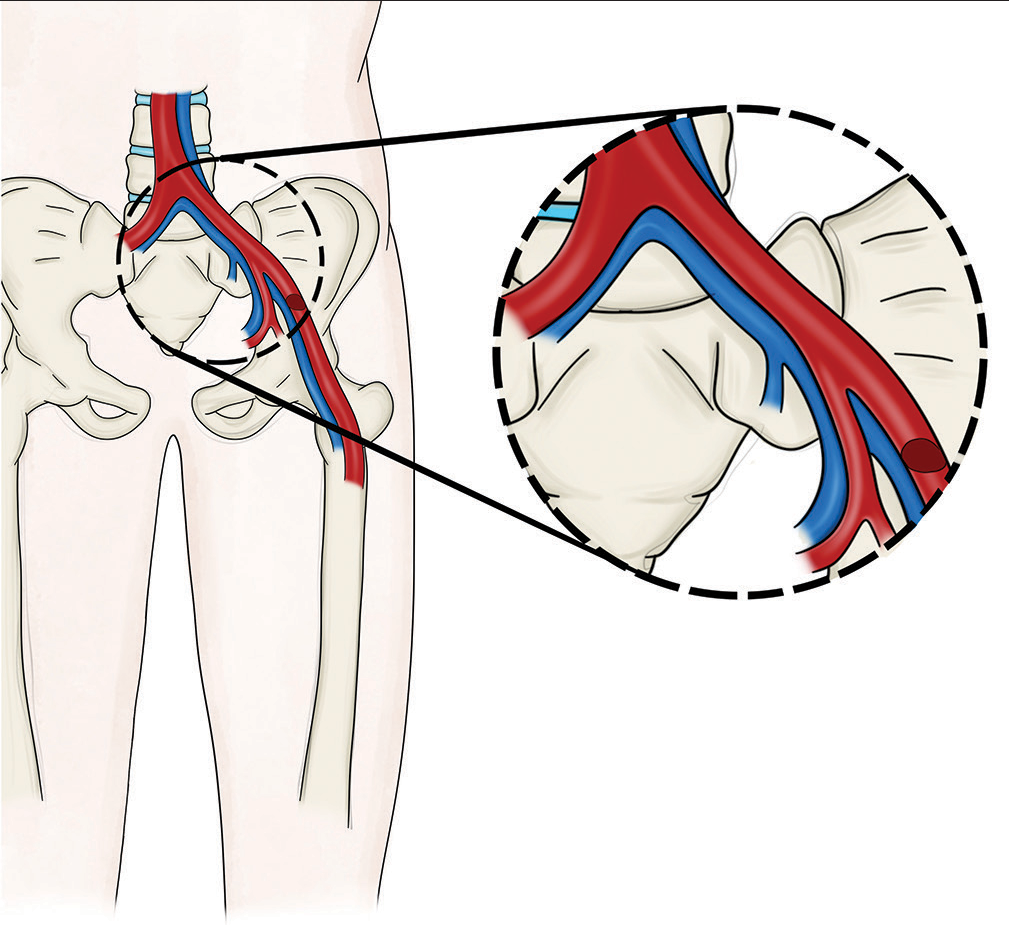
An L5-S1 discectomy and ALIF were performed. Of note, the bifurcation of the iliac vein and artery was located lower than expected, resulting in the left iliac vein lying directly over the L5-S1 disc, increasing the difficulty of the exposure. During the exposure of the L5-S1 disc space, the left iliac vein was noted to be bleeding; this was quickly stopped using Fibrillar hemostasis. This was followed by the completion of the L5-S1 discectomy/fusion that included placement of the femoral ring allograft and anterior screw-washer application in the sacrum to secure the graft.
Left iliac vein laceration and left iliac artery embolectomy by the vascular surgeon
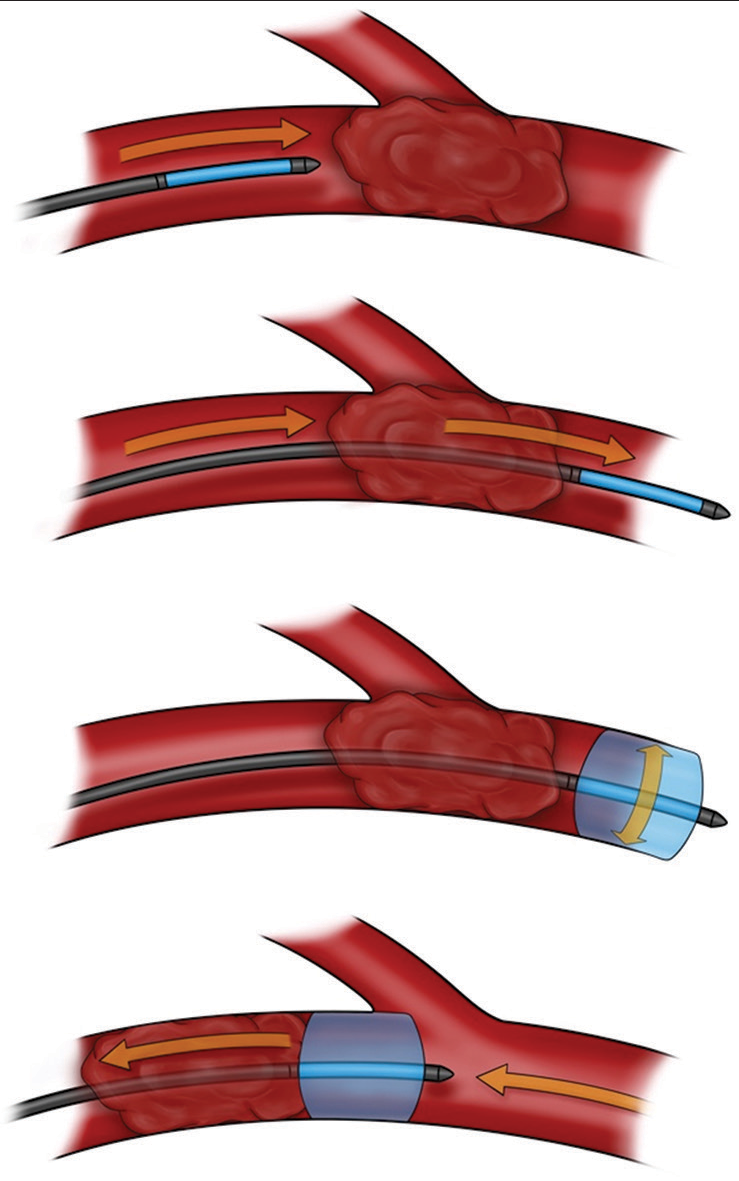
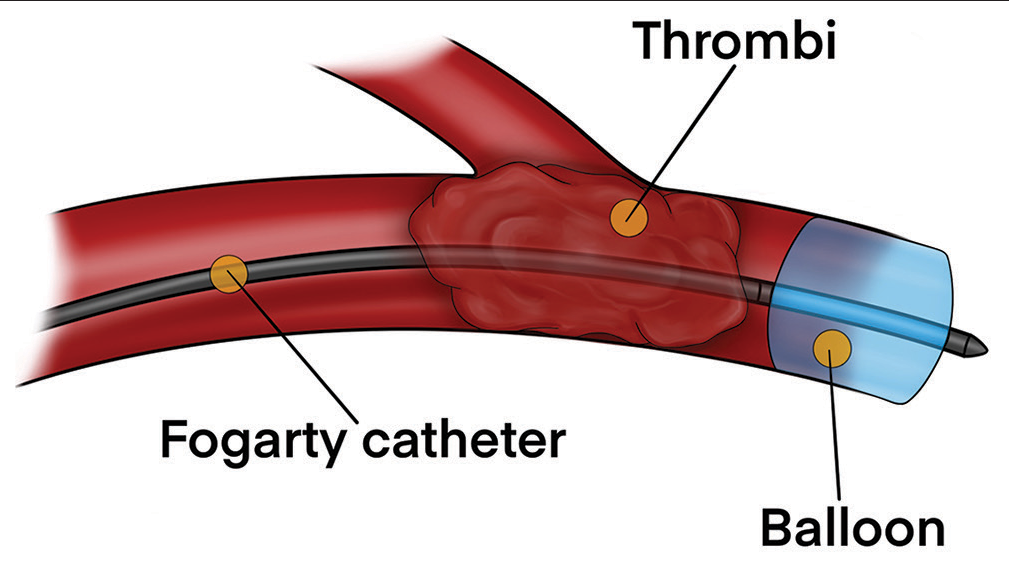
Once the retractors were removed, the iliac vein was noted to be bleeding again, and the vascular surgeon sutured the left iliac vein laceration (i.e., without any compromise). However, physical examination demonstrated a slightly cool left foot, and after the arterial Doppler and pulse oximeter both confirmed weak pulse in the left lower extremity (i.e., likely attributed to arterial retraction injury), the vascular surgeon performed a left iliac artery embolectomy [
Postoperative course
Following extubation, the patient was evaluated and demonstrated full motor function and sensation in all her toes. Close monitoring with repeated Doppler’s was performed to survey for potential recurrent/residual emboli. On postoperative day (POD) 2, the patient was taken back to the operating room for placement of percutaneous screws at the L5-S1 level. The rest of her stay was uneventful, including the absence of a left lower extremity deep venous thrombosis. Her intraoperative cultures showed no bacterial growth, and she was discharged home on POD 6. Three months later, she was asymptomatic, and imaging revealed solid fusion at the L5-S1 level [
DISCUSSION
Vascular injuries are the most frequent complication in ALIF and occur most often with exposure to the L4-L5 and L5-S1 disc spaces.[
Need for immediate access to vascular surgeons
Given the risk of vascular injuries associated with ALIF, adding a vascular surgeon to the surgical team is beneficial. When lacerations occur during exposure, the decision to continue the procedure should be a joint decision between the vascular and spine surgeon to determine if further mobilization might jeopardize the repair of the laceration.[
CONCLUSION
Using pulse oximeters in patients undergoing ALIF surgery can aid in facilitating the diagnosis and treatment of acute artery thrombi. When such vascular injuries arise, having immediate access to experienced vascular surgeons is critical to obtain expeditious treatment and optimize patient outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Asha MJ, Choksey MS, Shad A, Roberts P, Imray C. The role of the vascular surgeon in anterior lumbar spine surgery. Br J Neurosurg. 2012. 26: 499-503
2. Brau S, Delamarter RB, Schiffman ML, Williams LA, Watkins RG. Vascular injury during anterior lumbar surgery. J Spine. 2004. 4: 409-12
3. Chiriano J, Abou-Zamzam AM, Urayeneza O, Zhang WW, Cheng W. The role of the vascular surgeon in anterior retroperitoneal spine exposure: Preservation of open surgical training. J Vasc Surg. 2009. 50: 148-51
4. Choy W, Barrington N, Garcia RM, Kim RB, Rodriguez H, Lam S. Risk factors for medical and surgical complications following single-level ALIF. Global Spine J. 2017. 7: 141-7
5. Garg J, Woo K, Hirsch J, Bruffey JD, Dilley RB. Vascular complications of exposure for anterior lumbar interbody fusion. J Vasc Surg. 2010. 51: 946-50 discussion 950
6. Manunga J, Alcala C, Smith J, Mirza A, Titus J, Skeik N. Technical approach, outcomes, and exposure-related complications in patients undergoing anterior lumbar interbody fusion. J Vasc Surg. 2020. 73: 992-8
7. Mobbs RJ, Phan K, Daly D, Rao PJ, Lennox A. Approach-related complications of anterior lumbar interbody fusion: Results of a combined spine and vascular surgical team. Global Spine J. 2016. 6: 147-54