- Department of Neurosurgery, Dubrava University Hospital, Zagreb, Croatia
- Department of Surgery and Neurosurgery, School of Medicine, J.J. Strossmayer University of Osijek, Osijek, Croatia
- Department of Pathology and Cytology, Dubrava University Hospital, Zagreb, Croatia
Correspondence Address:
Marina Raguž
Department of Neurosurgery, Dubrava University Hospital, Zagreb, Croatia
DOI:10.4103/sni.sni_147_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Jurica Maraković, Tonko Marinović, Vjekoslav Jeleč, Domagoj Dlaka, Danko Muller, Andrea Blažević, Marina Raguž. Intraspinal calcinosis mimicking intervertebral disc extrusion: A clinical and surgical case report. 14-Aug-2018;9:166
How to cite this URL: Jurica Maraković, Tonko Marinović, Vjekoslav Jeleč, Domagoj Dlaka, Danko Muller, Andrea Blažević, Marina Raguž. Intraspinal calcinosis mimicking intervertebral disc extrusion: A clinical and surgical case report. 14-Aug-2018;9:166. Available from: http://surgicalneurologyint.com/surgicalint-articles/intraspinal-calcinosis-mimicking-intervertebral-disc-extrusion-a-clinical-and-surgical-case-report/
Abstract
Background:Subcutaneous calcinosis is a well-recognized manifestation of systemic sclerosis that usually involves multiple pressure points and may also be found in the paraspinal or intraspinal regions. In this case, intraspinal calcinosis uniquely led to a severe neurological deficit.
Case Description:A patient with severe systemic sclerosis/calcinosis exhibited left greater than right lower extremity radiculopathy attributed to intraspinal left-sided L4-L5 calcinosis. On examination, the patient exhibited bilateral positive Lasegue signs, distal lower extremity weakness (left greater than right), and bilaterally decreased Achilles responses. When the magnetic resonance imaging (MRI) revealed a significant intracanalicular mass on the left side at the L4-L5 level, the patient underwent a left-sided L4-L5 decompressive laminectomy. The MRI scan 5 years later revealed no recurrence of the calcinosis, and the patient had no residual neurological deficit.
Conclusions:Spinal calcinosis rarely involves the lumbar spinal canal. Here, a patient with a large left-sided L4-L5 focus of intraspinal calcinosis, mimicking a disc herniation, required a laminectomy to resect the lesion. Lumbar calcinosis should be radiologically evaluated utilizing using X-ray, MRI, and computed tomography studies to adequately document the pathology. Patients, when symptomatic, may require surgical decompression and excision of these lesions.
Keywords: CREST syndrome, spinal calcinosis, surgical treatment, systemic sclerosis
INTRODUCTION
Systemic sclerosis is classified into two groups based on the extent of skin thickening: (1) limited and (2) diffuse scleroderma. The acronym CREST refers to its five main features: calcinosis, Raynaud's disease, esophageal dysmotility, sclerodactyly, and telangiectasia. Subcutaneous calcinosis occurs in both types of systemic sclerosis, and is more common in patients with limited scleroderma as part of the CREST syndrome.[
CASE DESCRIPTION
History
A 56-year-old female patient presented with swelling of the joints of the hands and coldness of the extremities. A skin biopsy showed reduced blood vessels in the dermis, and degenerative changes in the collagen/elastic fibers. She was diagnosed with systemic sclerosis, and methotrexate was prescribed. She then presented with 3 months of increasing left lower extremity radiculopathy accompanied by bilateral positive Lasegue signs (30°), weakness of both dorsi and plantar flexion, and diminished Achilles reflexes.
Radiographic findings
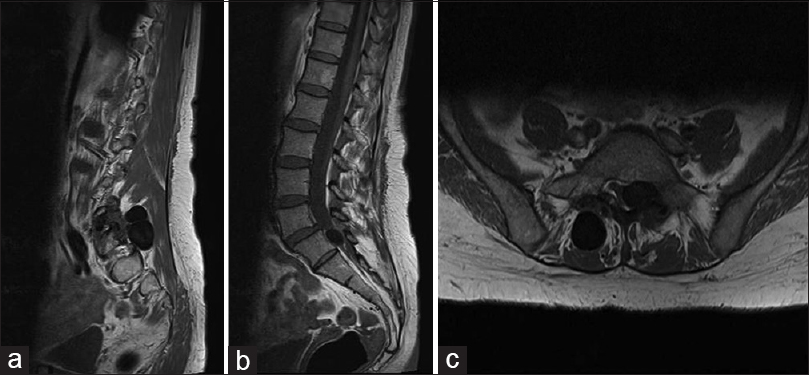
The X-rays showed stenosis at the L5 and S1 levels along with ossification involving the L3, L4, and L5 vertebral bodies. The most prominent magnetic resonance (MRI) finding was an intraspinal lesion at the L4-L5 level resulting in significant left L5 root compression. Additional MRI studies of the cervical, thoracic, and lumbar regions demonstrated additional intervertebral disc protrusions. In particular, the lumbosacral MRI revealed a perineural cyst of the sacrum, and a large calcified mass dorsal to S1 vertebral body [
Operation and postoperative course
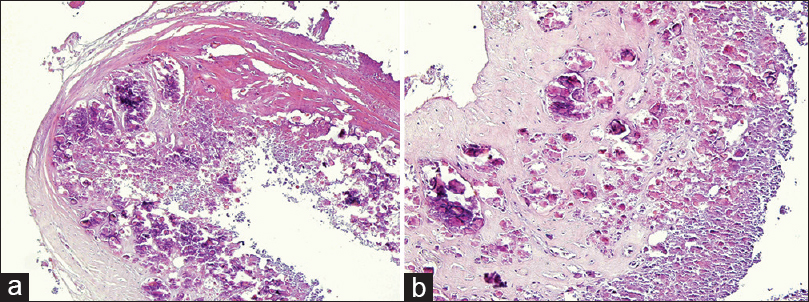
The patient underwent a laminectomy at the L4-L5 level, where a calcified mass was decompressed/excised. The pathohistological examination confirmed collagen fibers (accounting for the fibrinous external layer) covered by frank calcium deposits consistent with the diagnosis of calcinosis [
DISCUSSION
Types of calcinosis
Soft tissue calcifications are historically divided into four types: dystrophic, tumorous, metastatic, and idiopathic.[
Spinal locations of calcinosis
Spinal calcinosis rarely occurs.[
Neurological presentation of calcinosis
Neurological symptoms and signs of spinal calcinosis may include focal pain, weakness, radiculopathy, decreased range of motion, and focal neurological deficits.[
Lumbar laminectomy for calcinosis
Patients with significant neurological deficits associated with intraspinal calcinosis may require operative decompression.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arginteanu MS, Perin NI. Paraspinal calcinosis associated with progressive systemic sclerosis. Case report. J Neurosurg. 1997. 87: 761-3
2. Bluett J, Davies C, Harris J, Herrick A. Cervical spine calcinosis in systemic sclerosis. J Rheumatol. 2013. 40: 1617-8
3. Faraj K, Perez-Cruet K, Perez-Cruet M. CREST calcinosis affecting the lumbar and cervical spine and the use of minimally-invasive surgery. Cureus. 2017. 9: e1145-
4. Nagai Y, Sogabe Y, Ishikawa O. Tumoral calcinosis of the ribs and lumbar spine in systemic sclerosis. Eur J Dermatol. 2008. 18: 473-4
5. Nakamura T, Hirakawa K, Takaoka H, Iyama K. Dystrophic calcinosis with both a huge calcified mass in the cervical spine and calcification in the chest wall in a patient with rheumatoid overlap syndrome. Clin Rheumatol. 2016. 35: 1403-9
6. Ogawa T, Ogura T, Hayashi N, Hirata A. Tumoral calcinosis of thoracic spine associated with systemic sclerosis. J Rheumatol. 2009. 36: 2552-3
7. Ogawa T, Ogura T, Ogawa K, Hirata A, Hayashi N, Izumi Y. Paraspinal and intraspinal calcinosis: Frequent complications in patients with systemic sclerosis. Ann Rheum Dis. 2009. 68: 1655-6
8. Radhakrishnan K, Litchy WJ, O’Fallon WM. Epidemiology of cervical radiculopathy. A population-based study from Rochester Minnesota, 1975 through 1990. Brain. 1994. 117: 325-335
9. Schweitzer ME, Cervilla V, Manaster BJ, Gerharter J, Dalinka M, Peck WW. Cervical paraspinal calcification in collagen vascular diseases. AJR Am J Roentgenol. 1991. 157: 523-5
10. Shibuya S, Kawaguchi Y, Arima N, Yamamoto T, Dobashi H, Tokuda M. Tumoral calcinosis in bilateral facet joints of the lumbar spine in scleroderma. Case report. J Neurosurg Spine. 2006. 5: 451-4
11. Ward M, Curé J, Schabel S, Smith EA, Schumacher HR, Silver RM. Symptomatic spinal calcinosis in systemic sclerosis (scleroderma). Arthritis Rheum. 1997. 40: 1892-5