- Department of Neurosurgery, School Military Hospital Dr Alejandro Dávila Bolaños, Managua, Nicaragua.
Correspondence Address:
Doriam Alejandrino Perera Valdivia, Department of Neurosurgery, School Military Hospital Dr Alejandro Dávila Bolaños, Managua, Nicaragua.
DOI:10.25259/SNI_428_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Doriam Alejandrino Perera Valdivia, Luis Roberto Zapata Vega, Edgar Abraham Herrera Pérez. Intraventricular endoscopy and intraventricular antibiotics in the treatment of multiloculated hydrocephalus with ventriculitis in a neonate and an infant: Two case reports. 06-Oct-2023;14:354
How to cite this URL: Doriam Alejandrino Perera Valdivia, Luis Roberto Zapata Vega, Edgar Abraham Herrera Pérez. Intraventricular endoscopy and intraventricular antibiotics in the treatment of multiloculated hydrocephalus with ventriculitis in a neonate and an infant: Two case reports. 06-Oct-2023;14:354. Available from: https://surgicalneurologyint.com/surgicalint-articles/12584/
Abstract
Background: We present two pediatric cases, a neonate and an infant, who presented with treatment-refractory ventriculitis and multiloculated hydrocephalus treated with simultaneous intraventricular endoscopy and antibiotics. This is the first report of this combined therapy in children.
Case Description: Using intraventricular endoscopic surgery and antibiotics, hydrocephalus was treated with a minimum number of ventricular shunt systems. In addition, treatment-refractory ventriculitis was treated in both patients using intraventricular antibiotics.
Conclusion: Endoscopic surgery and intraventricular antibiotic administration are useful strategies for treating multiloculated hydrocephalus and ventriculitis in children.
Keywords: Infant, Intraventricular antibiotic, Intraventricular endoscopy, Multiloculated hydrocephalus, Neonate, Ventriculitis
INTRODUCTION
Complicated ventriculitis with multiloculated hydrocephalus is one of the most difficult diseases to cure in pediatric neurosurgery and is associated with high morbidity and mortality.[
In neurosurgery, intraventricular antibiotics are useful for adults and children with refractory ventriculitis.[
Intraventricular antibiotics are used to overcome the limitations of the blood-brain barrier to the passage of systemic antibiotics, significantly increasing local (cerebral) concentrations of antibiotics, and thereby improving their efficacy, especially in difficult-to-cure infections.[
Multiloculated hydrocephalus is usually associated with neonatal age and the presence of intraventricular hemorrhage due to premature birth or neonatal meningitis.[
CASE DESCRIPTIONS
Case one
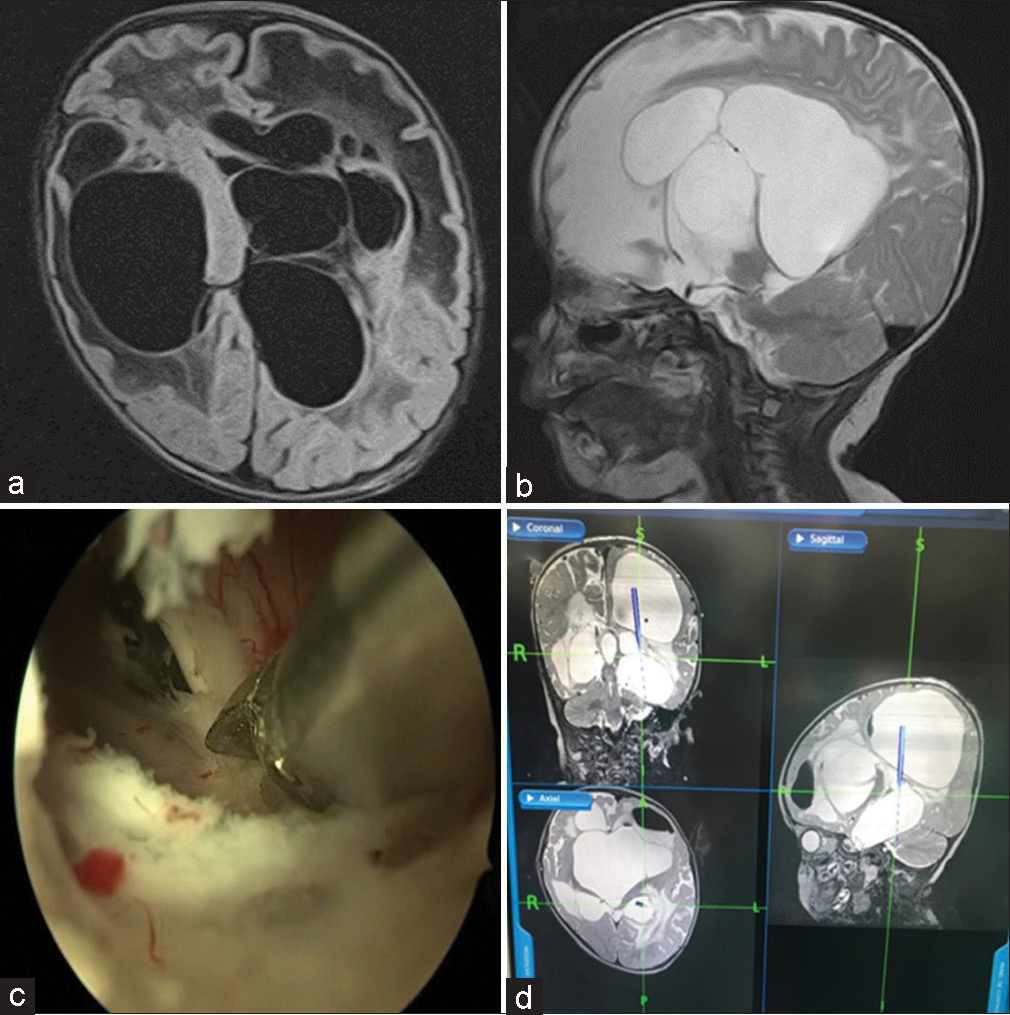
A 3-month-old male infant was referred to the pediatric department for neurosurgical consultation. The patient was treated for neonatal meningitis, which resolved. He was discharged from the hospital, and after 7 days, he presented with evidence of intracranial hypertension (accelerated increase in head circumference and bulging fontanelles). Brain computed tomography and magnetic resonance imaging revealed multiloculated hydrocephalus [
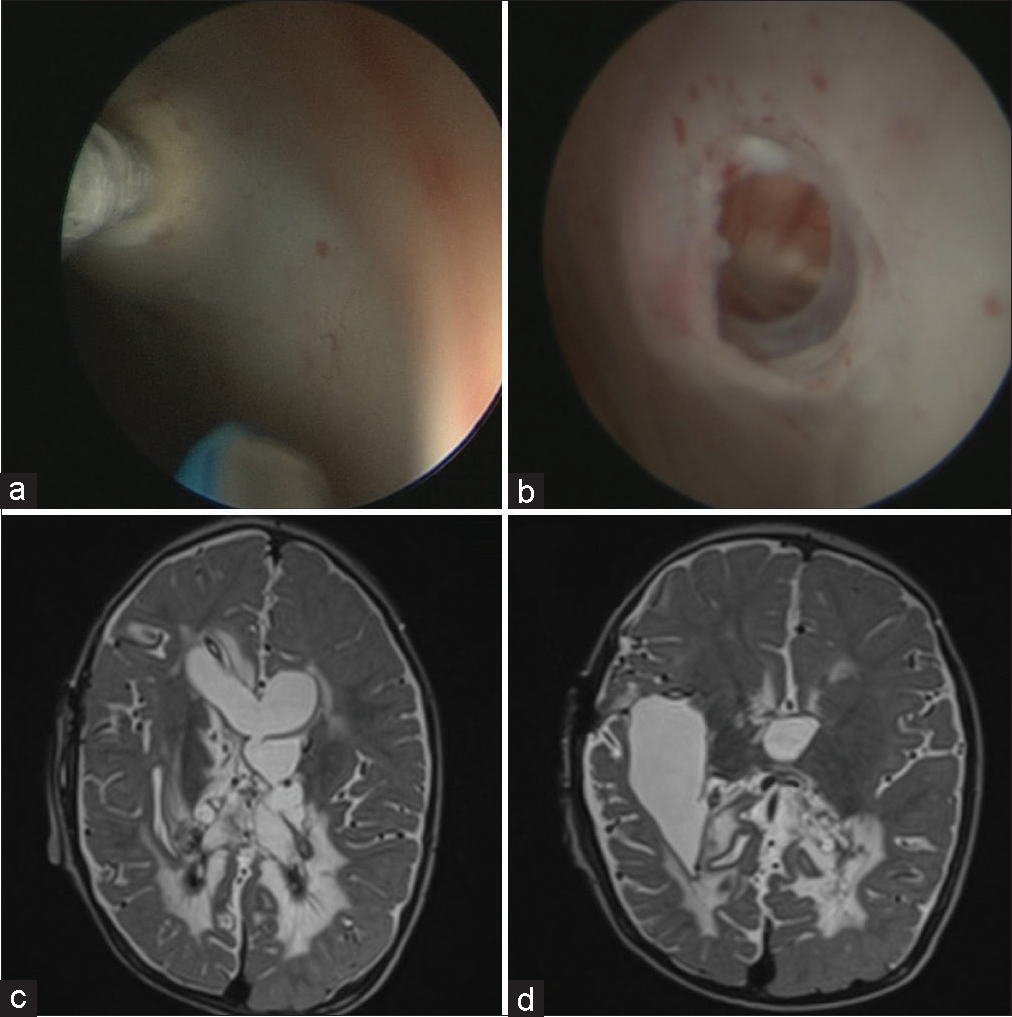
Figure 1:
(a and b) Initial brain magnetic resonance imaging in case one; multiloculated hydrocephalus is evident. (c) Second septostomy surgery to allow communication in the entire left ventricular system connecting the superior lateral ventricle with the inferior lateral ventricle (inferior temporal horn). Due to the greater thickness and fibrosis of this septum, it was not possible to perform the septostomy only with the take apart bipolar coagulator and Fogarty catheter (as in the other surgeries); however, we had to use sharp dissection with the help of microscissors. (d) Intraoperative neuronavigation images of the second septostomy surgery.
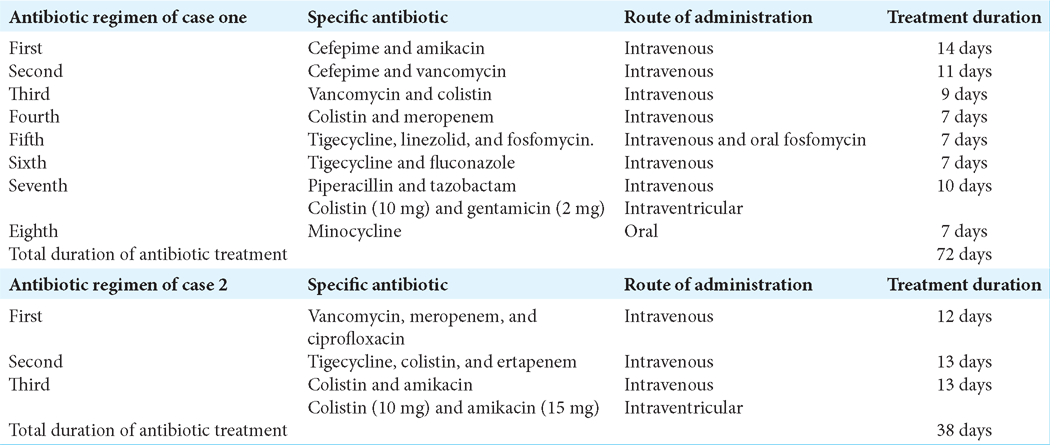
Two external ventricular drains (right and left) were placed, and cerebrospinal fluid (CSF) sampling confirmed the presence of multidrug-resistant Escherichia coli. Despite an 8-week course of various systemic antibiotics [
Based on imaging data and lack of response to prior antibiotic treatment, we planned three intraventricular endoscopic septostomy surgeries to facilitate hydrocephalus management. We consulted pediatric infectious disease specialists and decided to add intraventricular antibiotics to counteract the refractory ventriculitis.
A left posterior parietal approach was used during the first surgical procedure. For the septostomy surgeries, Karl Storz endonasal and skull base endoscopy equipment was used: a 2-mm and 0° endoscope, Fogarty French 3 catheter, Take Apart bipolar, and microscissors to cut adhesions and septa [
The objective of the first and second endoscopic septostomies was to communicate with the entire left ventricular system. In the first surgery, the entire superior lateral ventricle was connected. In the second surgery, the superior lateral ventricle was connected to the inferior lateral ventricle (left temporal horn) [
In the third endoscopic intraventricular septostomy, the septa dividing the right temporal ventricle were removed. When the right ventricular septum was incised, the right temporal horn was connected with the cisterns of the base using the transchoroidal fissure approach [
Figure 2:
(a) Third endoscopic septostomy surgery on the right side to connect the right ventricular temporal horn with the basal cisterns and left ventricular system through a transchoroidal fissure approach. (b) Intraoperative neuronavigation images. (c and d) Postsurgical magnetic resonance imaging before the patient was discharged. The entire communicating network of the ventricular system is evident, although not easily visible in a few images we can see the cerebral cortex without any tension and in fact a little separated from the skull, the most important thing is that with a single ventriculoperitoneal shunt system the clinical hydrocephalus resolved.
The patient was discharged and followed up for 1 year with no recurrence of neuroinfection or hydrocephalus and some slight psychomotor retardation. His general condition has so far been excellent.
Case two
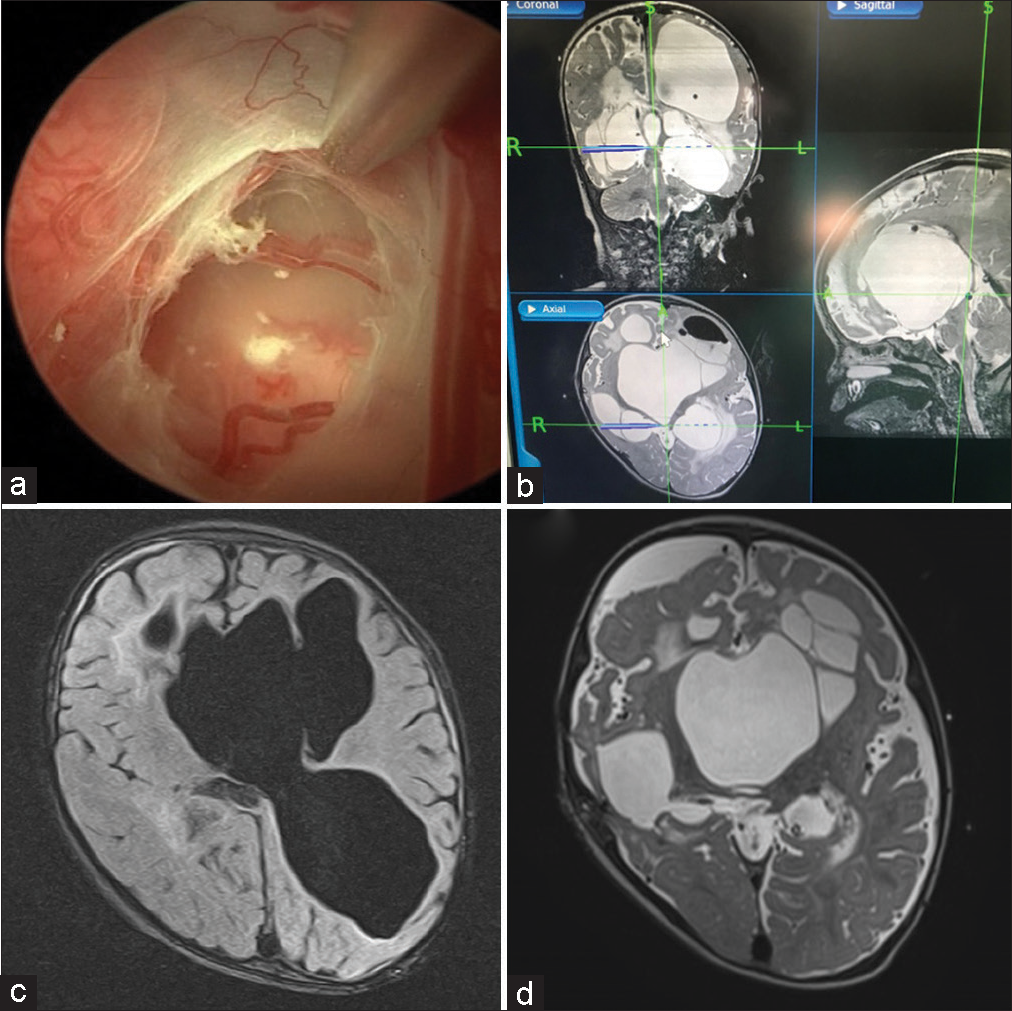
A 2-week-old male infant born with a ruptured lumbar myelomeningocele underwent surgery within 24 h of birth. The surgery was complicated by hydrocephalus and ventriculitis with ventricular empyema, which required endoscopic evacuation of the intraventricular empyema and placement of an external ventricular drain [
Figure 3:
(a) Initial magnetic resonance imaging in case two, where ventricular empyema is evident in the fluid-attenuated inversion recovery sequence (the initial stage of neuroinfection). (b-d) magnetic resonance imaging in case two, where multiloculated hydrocephalus is evident (advanced stage of neuroinfection).
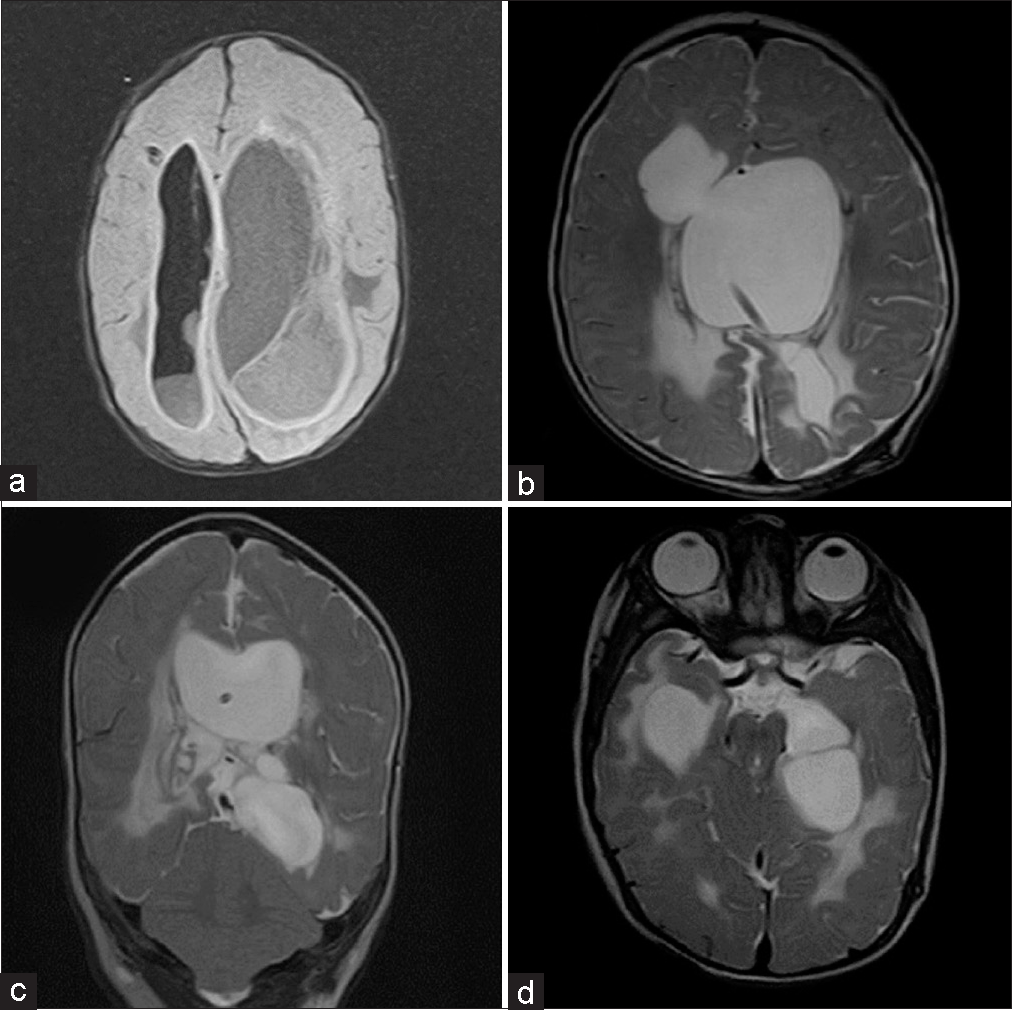
Over the following 3 weeks, the patient presented with multiple intraventricular septations [
After performing three intraventricular endoscopic septostomies, we connected two cavities of the ventricular system [
DISCUSSION
Multiloculated hydrocephalus
We described the treatment of two cases in which two diseases (multiloculated hydrocephalus and ventriculitis) with high morbidity and mortality in pediatric neurosurgery co-existed. The diseases were refractory to conventional medical treatment.
We examined the first patient with multilocular hydrocephalus to determine the optimal therapeutic approach. We considered several options, such as the traditional approach with multiple ventricular shunt systems or more recently developed therapeutic strategies, such as ventricular septostomy either by craniotomy or endoscopic ventricular septostomy. After reviewing the literature and based on our previous experience, we were convinced that the optimal option for such cases was ventricular septostomy. This approach avoids the excessive risk of morbidity and mortality from placing multiple ventricular catheters, such as an increased risk of infections and a high probability of requiring multiple re-interventions due to catheter obstructions.[
After determining that ventricular septostomy was the best treatment option, we decided whether to use a craniotomy or an intraventricular endoscopic approach. Initially, we believed that open surgery by means of a wide craniotomy was the optimal choice because of the complexity of the case and the relative ease of the microsurgical approach with greater control of hemostasis. However, we opted for an endoscopic approach to avoid the possible morbidity caused by excessive CSF drainage and other risks associated with a more invasive approach. In addition, we utilized the experience of one of our colleagues (a skull base specialist neurosurgeon) in cerebral endoscopy.[
Because the results were very effective and without associated morbidity, we used this endoscopic technique in the second pediatric case. Thus, intraventricular endoscopic septostomy is currently one of the first choices for treating septate hydrocephalus to minimize morbidity and the number of ventricular catheters required.
Treatment-refractory ventriculitis
Because our patients did not respond adequately to systemic antibiotic treatment, we explored other options to address treatment-refractory ventriculitis in neonates and infants. Drawing on past experiences, we considered the excellent results observed using intraventricular antibiotics for the treatment of refractory ventriculitis in adult patients.
Although a randomized study conducted among neonates in 1980[
CONCLUSION
In these two patients, one neonate and one infant, with multiloculated hydrocephalus and treatment-refractory ventriculitis, we performed an endoscopic septostomy and utilized intraventricular antibiotics to effectively treat these conditions without adverse effects.
To the best of our knowledge, this is the first report of the simultaneous use of intraventricular endoscopy and antibiotics to treat multiloculated hydrocephalus and treatment-refractory ventriculitis in children.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akbari SH, Holekamp TF, Murphy TM, Mercer D, Leonard JR, Smyth MD. Surgical management of complex multiloculated hydrocephalus in infants and children. Childs Nerv Syst. 2015. 31: 243-9
2. Albanese V, Tomasello F, Sampaolo S. Multiloculated hydrocephalus in infants. Neurosurgery. 1981. 8: 641-6
3. Al Menabbawy A, El Refaee E, Soliman MA, Elborady MA, Katri MA, Fleck S. Outcome improvement in cerebral ventriculitis after ventricular irrigation: A prospective controlled study. J Neurosurg Pediatr. 2020. 26: 682-90
4. Arnell K, Enblad P, Wester T, Sjölin J. Treatment of cerebrospinal fluid shunt infections in children using systemic and intraventricular antibiotic therapy in combination with externalization of the ventricular catheter: Efficacy in 34 consecutively treated infections. J Neurosurg. 2007. 107: 213-9
5. El-Ghandour NM. Endoscopic cyst fenestration in the treatment of multiloculated hydrocephalus in children. J Neurosurg Pediatr. 2008. 1: 217-22
6. Elkheshin SE, Bebars M. Endoscopic treatment of complex multiloculated hydrocephalus in children, steps that may help to decrease revision rate. Surg Neurol Int. 2021. 12: 434
7. Eller TW, Pasternak JF. Isolated ventricles following intraventricular hemorrhage. J Neurosurg. 1985. 62: 357-62
8. Eshra MA. Endoscopic management of septated, multiloculated hydrocephalus. Alex J Med. 2014. 50: 123-6
9. Hussain K, Salat M, Ambreen G, Iqbal J. Neurodevelopment outcome of neonates treated with intraventricular colistin for ventriculitis caused by multiple drug-resistant pathogens-a case series. Front Pediatr. 2020. 8: 582375
10. Jamjoom AB, Mohammed AA, Al-Boukai A, Jamjoom ZA, Rahman N, Jamjoom HT. Multiloculated hydrocephalus related to cerebrospinal fluid shunt infection. Acta Neurochir (Wien). 1996. 138: 714-9
11. Kalsbeck JE, DeSousa AL, Kleiman MB, Goodman JM, Franken EA. Compartmentalization of the cerebral ventricles as a sequela of neonatal meningitis. J Neurosurg. 1980. 52: 547-52
12. Karaiskos I, Galani L, Baziaka F, Giamarellou H. Intraventricular and intrathecal colistin as the last therapeutic resort for the treatment of multidrug-resistant and extensively drug-resistant Acinetobacter baumannii ventriculitis and meningitis: A literature review. Int J Antimicrob Agents. 2013. 41: 499-508
13. Lee YH, Kwon YS, Yang KH. Multiloculated hydrocephalus: Open craniotomy or endoscopy?. J Korean Neurosurg Soc. 2017. 60: 301-5
14. Mangi RJ, Holstein LL, Andriole VT. Treatment of gram-negative bacillary meningitis with intrathecal gentamicin. Yale J Biol Med. 1977. 50: 31-41
15. Matsunaga N, Hisata K, Shimizu T. An investigation into the vancomycin concentration in the cerebrospinal fluid due to vancomycin intraventricular administration in newborns: A study of 13 cases. Medicine (Baltimore). 2015. 94: e922
16. McCracken GH, Mize SG, Threlkeld N. Intraventricular gentamicin therapy in gram-negative bacillary meningitis of infancy. Report of the second neonatal meningitis cooperative study group. Lancet. 1980. 1: 787-91
17. Parasuraman JM, Albur M, Fellows G, Heep A. Monitoring intraventricular vancomycin for ventriculostomy access device infection in preterm infants. Childs Nerv Syst. 2018. 34: 473-9
18. Parasuraman JM, Kloprogge F, Standing JF, Albur M, Heep A. Population pharmacokinetics of intraventricular vancomycin in neonatal ventriculitis, a preterm pilot study. Eur J Pharm Sci. 2021. 158: 105643
19. Peraio S, Amen MM, Ali NM, Zaher A, Taha AN, Tamburrini G, editors. Endoscopic management of pediatric complex hydrocephalus. World Neurosurg. 2018. 119: e482-90 Erratum in: World Neurosurg 2019; 126:706
20. Sayyahfar S, Choobdar FA, Mashayekhi M, Jazi FM. Successful management of pan-resistant Acinetobacter baumannii meningitis without intrathecal or intraventricular antibiotic therapy in a neonate. Infect Chemother. 2021. 53: 146-50
21. Spennato P, Cinalli G, Ruggiero C, Aliberti F, Trischitta V, Cianciulli E. Neuroendoscopic treatment of multiloculated hydrocephalus in children. J Neurosurg. 2007. 106: 29-35
22. Spennato P, Mirone G, Cicala D, Ruggiero C, Di Martino G, De Caro ML, Cinalli G, editors. Pathophysiology and treatment of multiloculated hydrocephalus. Pediatric hydrocephalus. Milan, Italy: Springer; 2019. p. 855-905
23. Tamber MS, Klimo P, Mazzola CA, Flannery AM. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 8: Management of cerebrospinal fluid shunt infection. J Neurosurg Pediatr. 2014. 14: 60-71
24. Teo C, Kadrian D, Hayhurst C. Endoscopic management of complex hydrocephalus. World Neurosurg. 2013. 79: S21.e1-7
25. Tunkel AR, Hasbun R, Bhimraj A, Byers K, Kaplan SL, Scheld WM. 2017 Infectious diseases society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. 2017. 64: e34-65
26. Venkataramana NK. Multiloculated hydrocephalus: Evolution of treatments and outcome. J Pediatr Neurosci. 2021. 16: 232-9
27. Wen DY, Bottini AG, Hall WA, Haines SJ. Infections in neurologic surgery. The intraventricular use of antibiotics. Neurosurg Clin N Am. 1992. 3: 343-54
28. Wright PF, Kaiser AB, Bowman CM, McKee KT, Trujillo H, McGee ZA. The pharmacokinetics and efficacy of an aminoglycoside administered into the cerebral ventricles in neonates: Implications for further evaluation of this route of therapy in meningitis. J Infect Dis. 1981. 143: 141-7
29. Yeung CY. Intrathecal antibiotic therapy for neonatal meningitis. Arch Dis Child. 1976. 51: 686-90
30. Zuccaro G, Ramos JG. Multiloculated hydrocephalus. Childs Nerv Syst. 2011. 27: 1609-19