- Department of Orthopaedics, Kawasaki Medical School, Kurashiki, Japan.
Correspondence Address:
Seiya Watanabe, Department of Orthopaedics, Kawasaki Medical School, Kurashiki, Japan.
DOI:10.25259/SNI_147_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seiya Watanabe, Kazuo Nakanishi, Yoshihisa Sugimoto, Kazuya Uchino, Hideaki Iba. Investigation of long lateral mass screw insertion torque. 29-Mar-2024;15:111
How to cite this URL: Seiya Watanabe, Kazuo Nakanishi, Yoshihisa Sugimoto, Kazuya Uchino, Hideaki Iba. Investigation of long lateral mass screw insertion torque. 29-Mar-2024;15:111. Available from: https://surgicalneurologyint.com/surgicalint-articles/12828/
Abstract
Background: Here, we assessed a new trajectory and insertion torque for the placement of a long lateral mass screw (LLMS) that offers stronger posterior fixation versus a shorter lateral mass screw (LMS) in the posterior cervical spine. We report a short technical note of the insertion torque of LLMS.
Methods: The insertion trajectory/torque was evaluated in 30 patients (10 males and 20 females) undergoing posterior cervical LLMS fusions (2021–2023). Patients averaged 65 years of age. Pathology included eight cervical spine injuries, ten cord injuries, four dislocations/fractures, and eight other entities. Variables studied included the length of the LLMS inserted from C3–7, screw deviation rates, insertion torque, and adverse events.
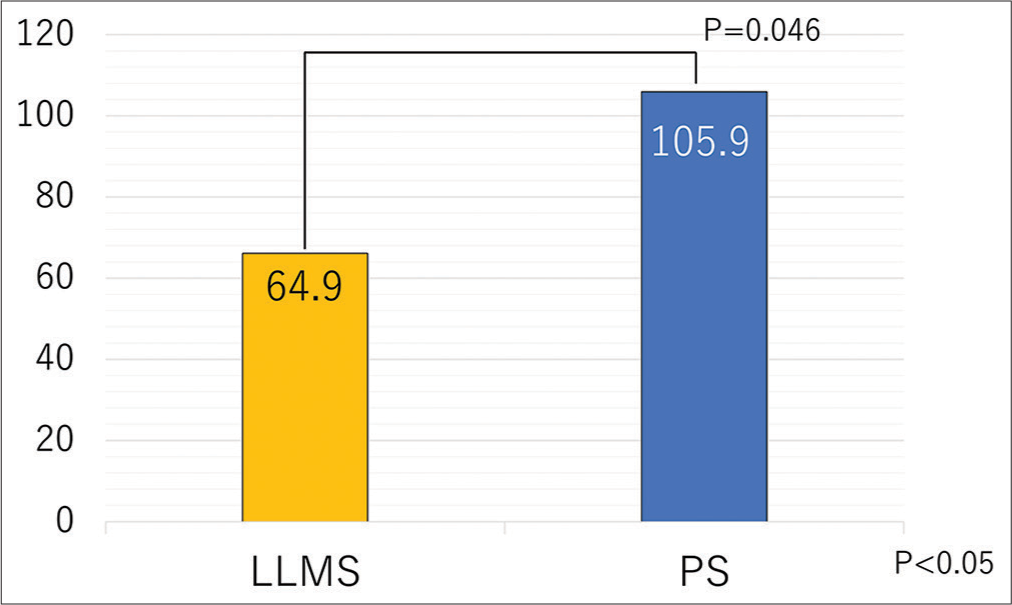
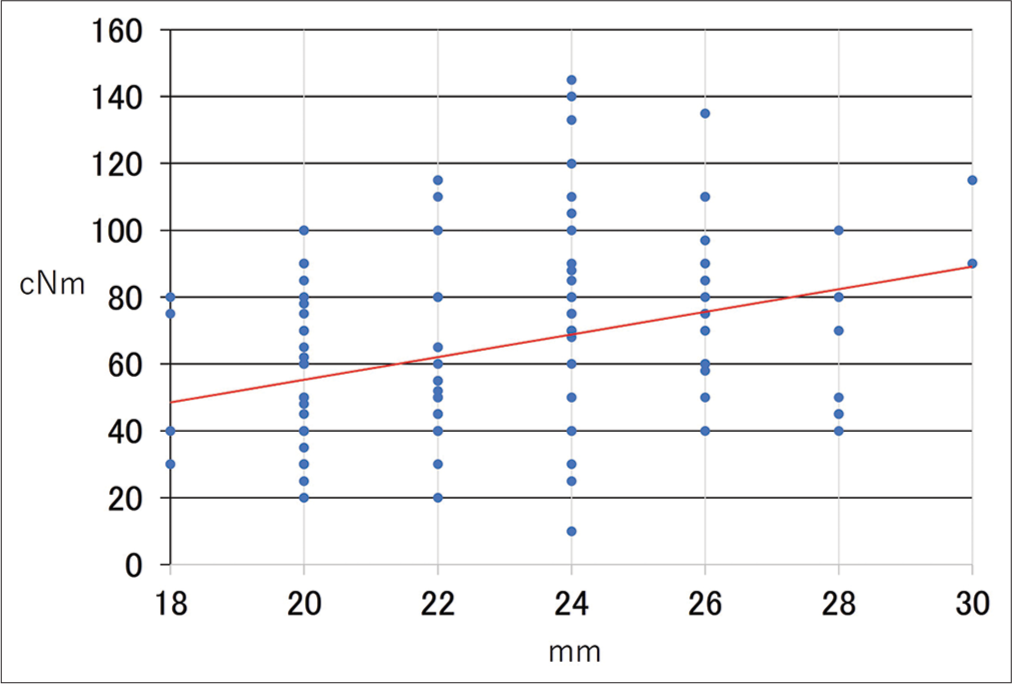
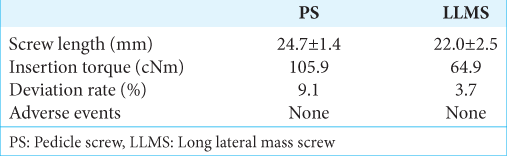
Results: A total of 146 screws were inserted: 11 pedicle screws (PSs) and 135 LLMS. The average insertion torque was 105.9 cNm for PS and 64.9 cNm for LLMS. As the screw lengthened by 1 mm, the insertion torque increased by approximately 4.4 cNm.
Conclusion: Here, we documented that the insertion torque of LLMS was 66.1 cNm, greater than the 51.0 cNm for LMS, which should provide stronger posterior cervical fixation.
Keywords: Cervical, Insertion torque, Lateral mass screw
INTRODUCTION
Here, we report a new trajectory and technique for the placement of a long lateral mass screw (LLMS) versus a Lateral mass screw (LMS) that should facilitate stronger posterior cervical spine fusion.[
MATERIALS AND METHODS
We evaluate the trajectory and insertion torque for placing LLMS in 30 patients (10 males and 20 females) undergoing posterior cervical spine fusion (2021–2023); patients averaged 65 years old. Pathologies addressed included eight cases of cervical spine injuries, ten cord injuries, four dislocations/fractures, and eight other cases. Variables studied included screw length, insertion torque, screw deviation rate, and adverse events.
RESULTS
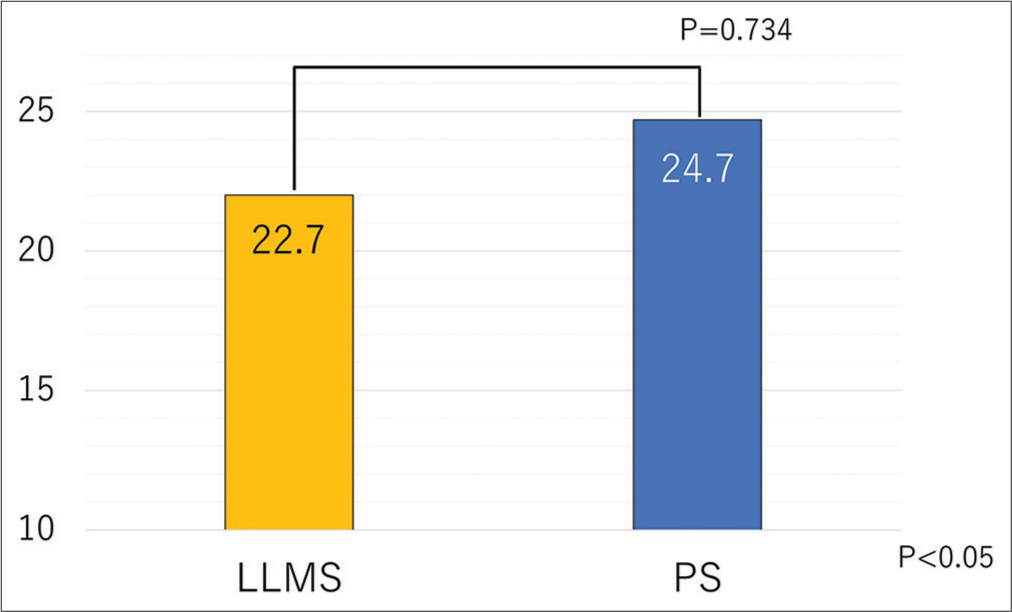
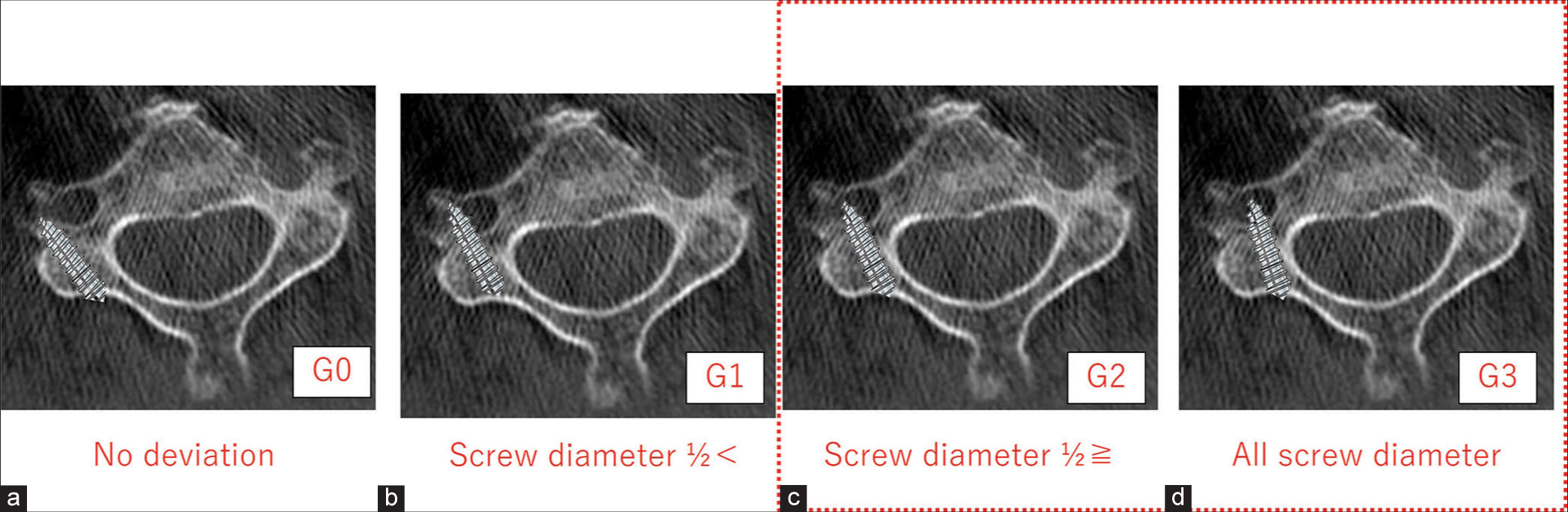
A total of 146 screws were inserted’ 11 pedicle screws (PS) and 135 LLMS. The average screw length was 24.7 ± 1.4 mm (22–26 mm) for PS and 22.0 ± 2.5 mm (18– 30 mm) for LLMS (P = 0.74) [
DISCUSSION
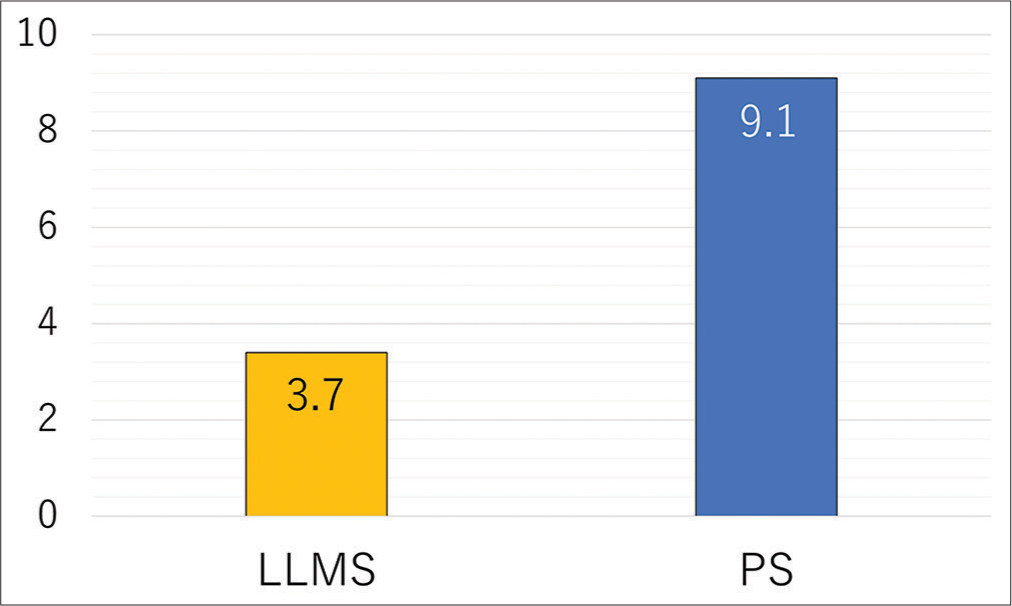
PS has a good posterior cervical fixation, but if it deviates, there is a risk of major complications (i.e., range 1.2–18.2%) even with navigation.[
CONCLUSION
We concluded that the insertion torque of LLMS was higher than that of LMS and that LLMS provides stronger posterior cervical fixation.
Ethical approval
The research/study approved by the Institutional Review Board at Kawasaki medical school, number 3782, dated 2019/12/19.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Magerl F, Seeman PF, Grob D, editors. Stable dorsal fusion of cervical spine (C2-T1) using hook plates. The cervical spine 1. New York: Springer Verlag; 1987. p.
2. Roy-Camille R, Saillant G, Laville C, Benazet JP. Treatment of lower cervical spinal injuries-C3 to C7. Spine (Phila Pa 1976). 1992. 17: S442-6
3. Shimokawa N, Sato H, Shirosaka K, Nakagawa C, Takami T. Accuracy of cervical pedicle screw placement with a navigation system. Spinal Surg. 2017. 31: 59-66
4. Watanabe S, Nakanishi K, Uchino K. Usefulness of the long lateral mass screw. J Spine Res. 2021. 12: 16-22