- Department of Surgery, Aga Khan University Hospital, Karachi, Pakistan.
Correspondence Address:
Shahzad M. Shamim, Department of Surgery, Aga Khan University Hospital, Karachi, Pakistan.
DOI:10.25259/SNI_127_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ayesha Sohail, Mohammad Hamza Bajwa, Qurat-Ul-Ain Virani, Anam Tariq, Nasr Hussain, Shahzad M. Shamim. Is endoscopic third ventriculostomy a viable treatment option for normal pressure hydrocephalus? A systematic review. 10-May-2024;15:154
How to cite this URL: Ayesha Sohail, Mohammad Hamza Bajwa, Qurat-Ul-Ain Virani, Anam Tariq, Nasr Hussain, Shahzad M. Shamim. Is endoscopic third ventriculostomy a viable treatment option for normal pressure hydrocephalus? A systematic review. 10-May-2024;15:154. Available from: https://surgicalneurologyint.com/surgicalint-articles/12892/
Abstract
Background: Endoscopic third ventriculostomy (ETV) is considered an alternative treatment for hydrocephalus and has become a standard of care for obstructive hydrocephalus. Recent studies have also explored its role in normal pressure hydrocephalus (NPH). We conducted a systematic review aiming to assess the outcomes of this minimally invasive endoscopic technique as a viable treatment option for NPH.
Methods: A systematic literature search was performed using PubMed and Scopus databases, using iterations of search terms “Endoscopic third ventriculostomy,” “Idiopathic normal pressure hydrocephalus,” and “Normal pressure hydrocephalus.” To be eligible for inclusion in the review, articles had to report the usage of ETV as a primary treatment modality for NPH, report its outcomes, and be published in the English language.
Results: Out of the 13 studies selected for qualitative synthesis, nine supported the use of ETV for NPH as an effective treatment option with improvement in the preoperative symptoms. Two studies favored shunt over ETV, stating that quality of life is better with VP shunt insertion. One study reported that ETV has higher perioperative mortality rates that outweigh its benefits. One study reported it to be an ineffective surgical option.
Conclusion: The current review of evidence does not support the use of ETV for the treatment of NPH, except perhaps in a small subset of patients. These patients have a shorter duration of symptoms and a better preoperative neurological status. The lumbar infusion test and ventricular infusion test are modalities useful for selecting these candidates.
Keywords: Endoscopic third ventriculostomy, Idiopathic normal pressure hydrocephalus, Normal pressure hydrocephalus, Systematic review
INTRODUCTION
Endoscopic third ventriculostomy (ETV) is a technique that uses a rigid or flexible endoscope to perforate the floor of the third ventricle to create communication between the third ventricle, interpeduncular, and prepontine subarachnoid spaces. It is a minimally invasive procedure that is used mainly to treat obstructive hydrocephalus.[
NPH is clinically characterized by the Hakim-Adams triad, which includes gait ataxia, cognitive dysfunction, and urinary incontinence.[
In this review, we aim to evaluate the utility of ETV for the management of patients with NPH to determine whether it might be a suitable option in comparison to other modalities.
MATERIALS AND METHODS
This systematic review has been reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
Search strategy
An electronic search of literature was conducted using PubMed and Scopus on February 02, 2023, and the following search strategies were used: (((ETV) OR (Endoscopic third ventriculostomy) OR (Third ventriculostomy) OR (Microscopic third ventriculostomy) OR (Endoscopic 3rd ventriculostomy)) AND (iNPH) OR (Idiopathic normal pressure hydrocephalus) OR (NPH) OR (Normal pressure hydrocephalus))).
Inclusion and exclusion criteria
All observational studies comprising cross-sectional, cohorts, as well as randomized control trials in which ETV was used for treating iNPH or NPH were included in the study. Case reports, conference papers, commentaries, articles other than English language, and review articles were excluded from the study. All the articles in which ETV was not used as the primary modality of treatment were excluded from the study. Articles in which ETV was used in obstructive/noncommunicating hydrocephalus or had mixed cohorts where individual data for NPH could not be determined were also excluded from the study.
Study selection
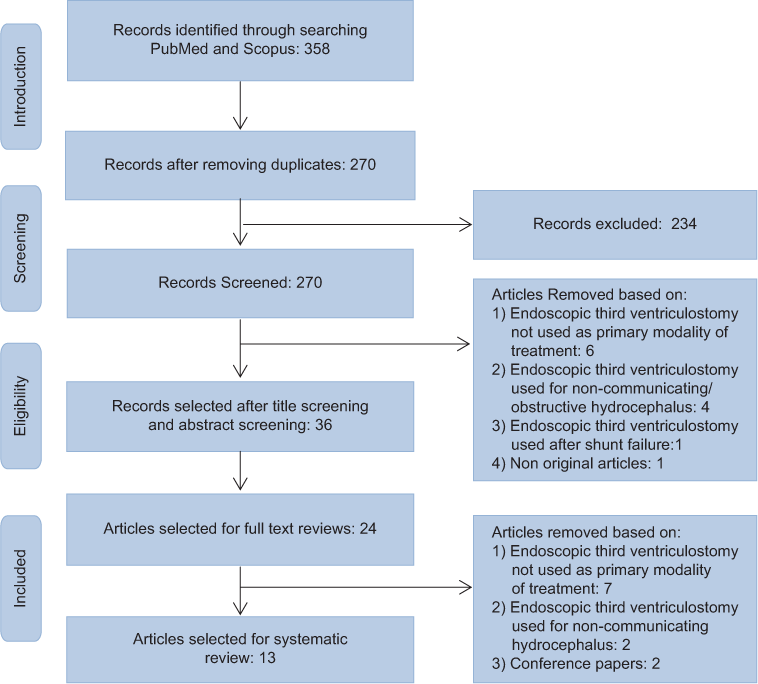
The initial results of our database search were reviewed, and duplicates were removed [
Data extraction
The selected articles were reviewed, and data describing the authors of the study, year of publication, type of study, total number of patients, demographics of patients, presented pathology (type of hydrocephalus), number of patients who underwent ETV, presenting symptoms, outcomes of the procedure, factors defining ETV success, postoperative complications, number of patients who had to undergo re-intervention, and factors contributing in better ETV outcome were extracted. Due to heterogeneous data present between cohorts, meta-analysis was not possible. A qualitative assessment of all the articles was conducted using the National Institutes of Health (NIH) Quality Assessment Tool for Cohorts, Cross-Sectional Studies, and Randomized Controlled Trials.
RESULTS
A total of 358 articles were identified (176 on Scopus and 182 on PubMed) from the search algorithm from which duplicates were removed, titles and abstracts were screened, and 13 articles were selected that met all inclusion criteria for subjective analysis.
Risk of bias within studies
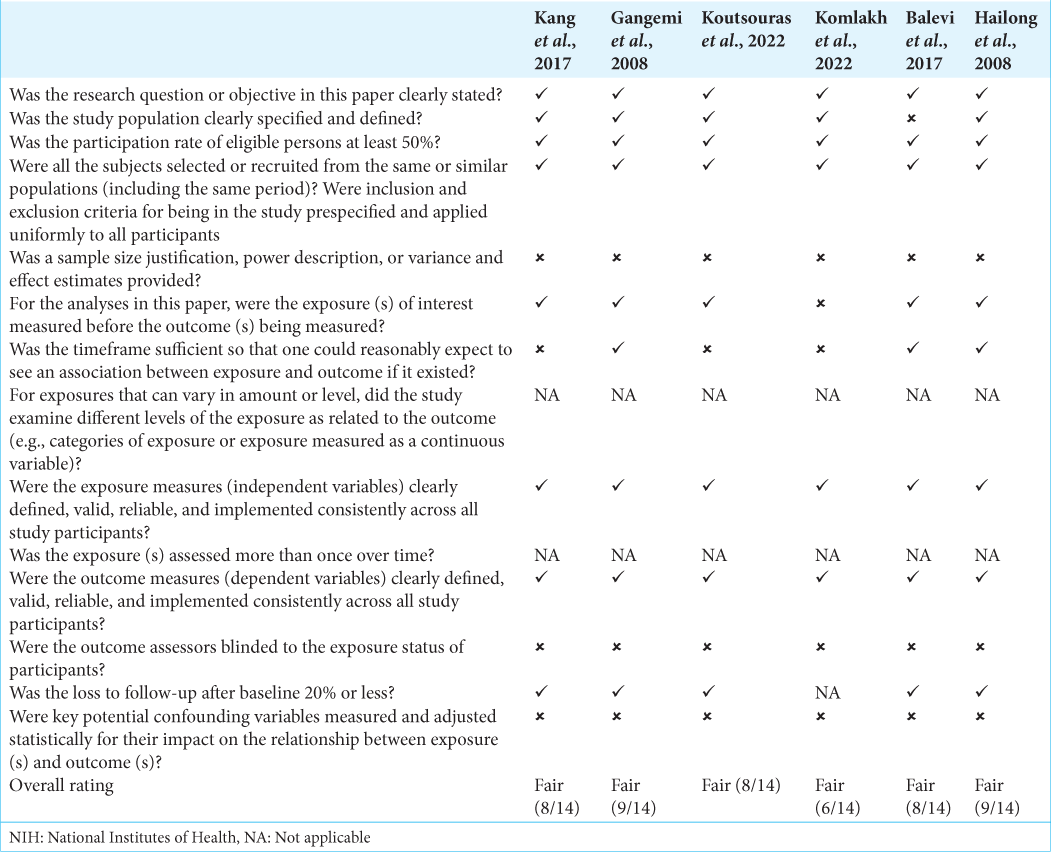
The NIH Quality Assessment Tool for Cohorts, Cross-Sectional Studies, and Randomized Controlled Trials was used by two authors, A.S. and Q.V., independently and the results were then compared. All of the 13 studies were reported as fair-quality studies, as shown in
ETV as a primary treatment modality in NPH
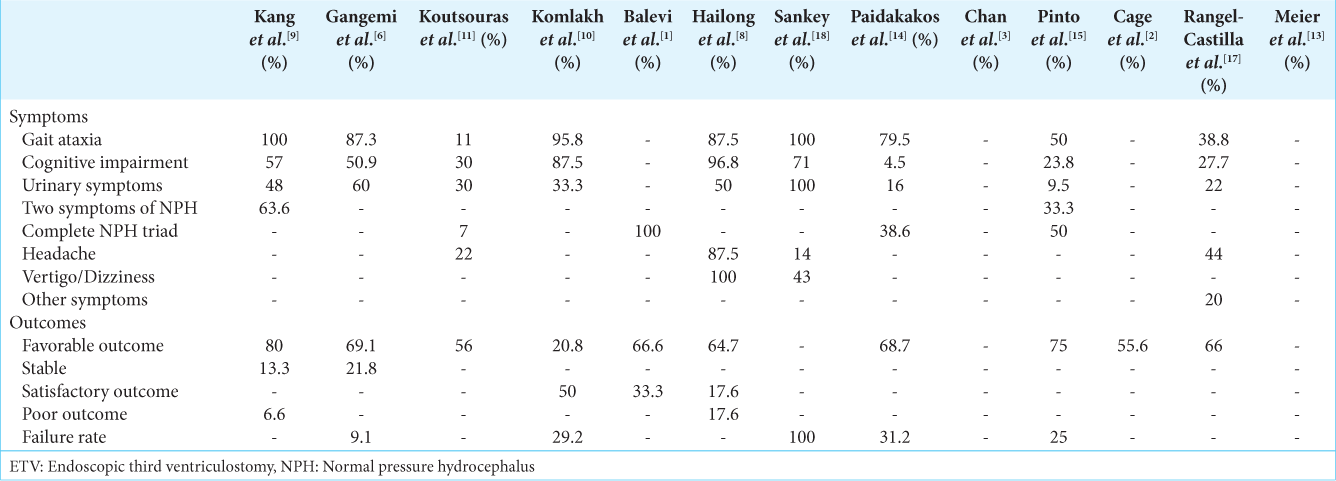
ETV success in NPH patients is defined by the improvement in the patient’s neurological status and preoperative symptoms, that is, gait, urinary incontinence, and dementia post-procedure, whereas ETV failure is defined by the worsening of preoperative symptoms and deterioration of the neurological status necessitating the need for another endoscopic procedure or shunt insertion later on.
Kang et al., in 2017, reported the use of ETV among 15 out of 21 patients diagnosed with NPH.[
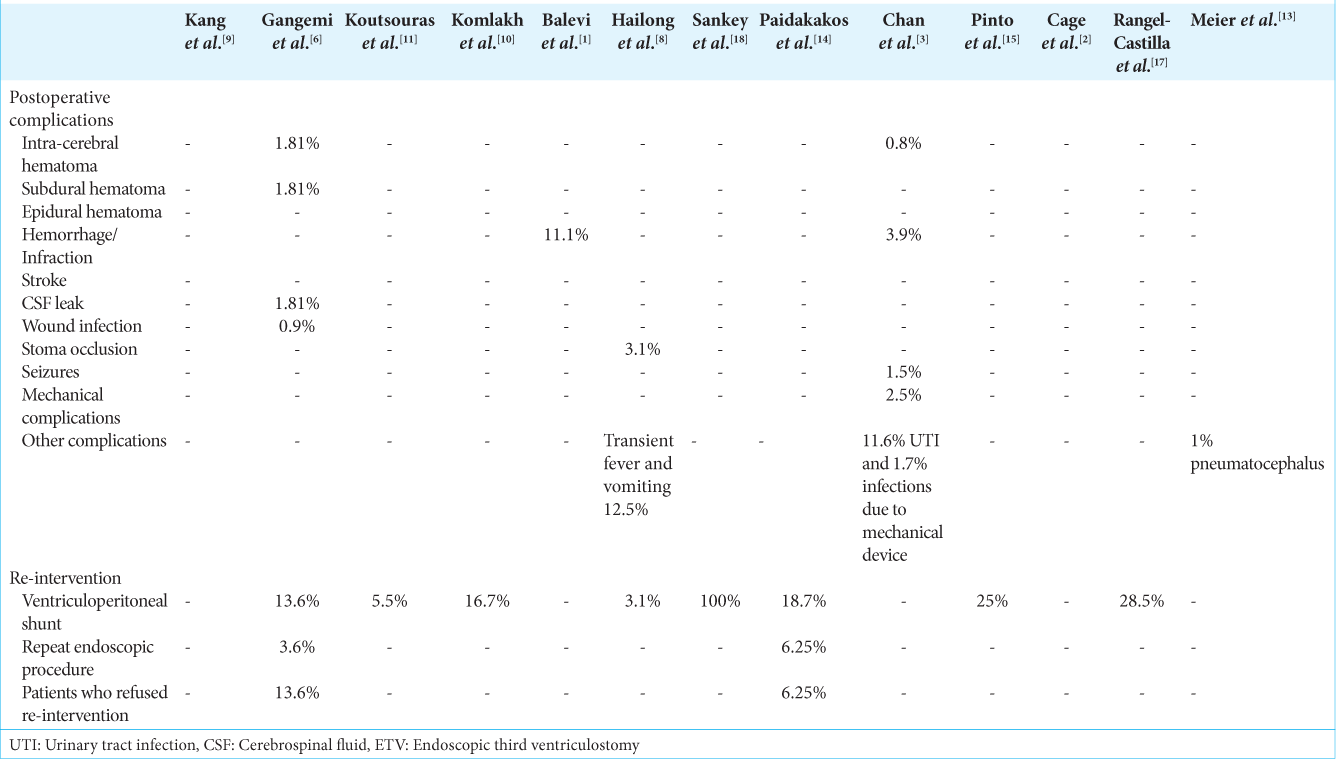
Postoperative complications and the need for re-intervention after ETV
Gangemi et al., reported 1.81% intracerebral hematomas, 1.81% subdural hematomas, 1.81% CSF leak, and 0.9% wound infections postoperatively.[
Factors favoring the use of ETV in NPH
Kang et al., in their study, stated that adult NPH patients with positive aqueductal flow void on T2 sagittal magnetic resonance imaging (MRI) and aqueductal peak velocity >5 cm/s on cine MRI have better outcomes when being treated with ETV.[
DISCUSSION
Mechanism of ETV
Cerebral parenchyma, in normal conditions, acts as a viscoelastic tissue that adequately disperses CSF pressure. In patients with NPH, this brain elasticity is lost due to multiple factors, such as insufficient transcortical subarachnoid space, fibrosis, meningitis, and small periventricular ischemic lesions that weaken the cerebral ventricles and decrease the absorption of CSF. Fenestration of the floor of the third ventricle by an ETV is purported to decrease the intraventricular pressure and increase the cerebral blood flow and perfusion pressure.[
ETV success in NPH
Rangel-Castilla et al., in their study of 36 patients with communicating hydrocephalus, reported the use of ETV as a good surgical option in replacing malfunctioning shunts and in the treatment of NPH, allowing patients to be shunt independent.[
Factors contributing to ETV’s success
Kang et al. conducted a study to determine the efficacy of ETV in older age patients with NPH. About 80% of the patients who underwent ETV for NPH showed improvement in preoperative symptoms. The group concluded that ETV is effective in carefully selected elderly patients with NPH, given that they have a positive aqueductal flow void on T2 sagittal MRI and their aqueductal peak velocity is >5 cm/s on cine MRI.[
ETV failure in NPH patients
While some studies suggest ETV to be a reasonable option for treating NPH, several studies report that ETV has higher perioperative mortality and complication rates as compared to VP shunt, which outweighs its potential benefits. Sankey et al. studied gait outcomes in NPH patients and reported ETV to be ineffective, with a failure rate of 100% in treating NPH. Not only did ETV fail to improve gait but also all the patients ultimately had to undergo shunt placements for a better outcome.[
The studies included in this review had heterogeneous data available, which was nonuniformly presented. Of the 13 studies included in this review, only one was a randomized controlled trial, two were cross-sectional studies, and the rest were cohorts. Eleven out of these 13 studies had a small sample size, which limits the generalizability of these results. Almost all the studies reported the need for further studies with a larger sample size and suggested further randomized controlled trials to confirm their results and to understand the effectiveness of ETV for NPH better.
CONCLUSION
There is inconclusive data to support ETV as an effective treatment option for NPH. Based on the literature available so far, ETV cannot be used as an interchangeable alternative to VP shunts other than in carefully selected patients. These include patients with a shorter clinical history, those with better preoperative neurological status, patients having pathologically increased outflow resistance on ventricular infusion tests, and physiologically increased outflow resistance on lumbar infusion tests.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Balevi M. Endoscopic third ventriculostomy in normal pressure hydrocephalus and symptomatic long-standing overt ventriculomegaly. Asian J Neurosurg. 2017. 12: 605-12
2. Cage TA, Auguste KI, Wrensch M, Wu YW, Gupta N. Self-reported functional outcome after surgical intervention in patients with idiopathic normal pressure hydrocephalus. J Clin Neurosci. 2011. 18: 649-54
3. Chan AK, McGovern RA, Zacharia BE, Mikell CB, Bruce SS, Sheehy JP. Inferior short-term safety profile of endoscopic third ventriculostomy compared with ventriculoperitoneal shunt placement for idiopathic normal-pressure hydrocephalus: A population-based study. Neurosurgery. 2013. 73: 951-60 discussion 960-1
4. Demerdash A, Rocque BG, Johnston J, Rozzelle CJ, Yalcin B, Oskouian R. Endoscopic third ventriculostomy: A historical review. Br J Neurosurg. 2017. 31: 28-32
5. Fountas KN, Kapsalaki EZ, Paterakis KN, Lee GP, Hadjigeorgiou GM. Role of endoscopic third ventriculostomy in the treatment of selected patients with normal pressure hydrocephalus. Acta Neurochir Suppl. 2012. 113: 129-33
6. Gangemi M, Maiuri F, Naddeo M, Godano U, Mascari C, Broggi G. Endoscopic third ventriculostomy in idiopathic normal pressure hydrocephalus: An Italian multicenter study. Neurosurgery. 2008. 63: 62-7 discussion 67-9
7. Giordan E, Palandri G, Lanzino G, Murad MH, Elder BD. Outcomes and complications of different surgical treatments for idiopathic normal pressure hydrocephalus: A systematic review and meta-analysis. J Neurosurg. 2018. p. 1-13
8. Hailong F, Guangfu H, Haibin T, Hong P, Yong C, Weidong L. Endoscopic third ventriculostomy in the management of communicating hydrocephalus: A preliminary study. J Neurosurg. 2008. 109: 923-30
9. Kang YS, Park EK, Kim JS, Kim DS, Thomale UW, Shim KW. Efficacy of endoscopic third ventriculostomy in old aged patients with normal pressure hydrocephalus. Neurol Neurochir Pol. 2018. 52: 29-34
10. Komlakh K, Oveisi H, Hossein Aghamiri S. Endoscopic third ventriculostomy as treatment option for normal pressure hydrocephalus. Eur J Transl Myol. 2022. 32: 10618
11. Koutsouras GW, Steinmetz E, Tichenor M, Schmidt B, Mohan YS, Krishnamurthy S. Endoscopic third ventriculostomy and cortical biopsy in patients with normal pressure hydrocephalus. Cureus. 2022. 14: e31523
12. Kulkarni AV, Shams I, Cochrane DD, McNeely PD. Quality of life after endoscopic third ventriculostomy and cerebrospinal fluid shunting: An adjusted multivariable analysis in a large cohort. J Neurosurg Pediatr. 2010. 6: 11-6
13. Meier U, Zeilinger FS, Schönherr B. Endoscopic ventriculostomy versus shunt operation in normal pressure hydrocephalus: Diagnostics and indication. Minim Invasive Neurosurg. 2000. 43: 87-90
14. Paidakakos N, Borgarello S, Naddeo M. Indications for endoscopic third ventriculostomy in normal pressure hydrocephalus. Acta Neurochir Suppl. 2012. 113: 123-7
15. Pinto FC, Saad F, Oliveira MF, Pereira RM, Miranda FL, Tornai JB. Role of endoscopic third ventriculostomy and ventriculoperitoneal shunt in idiopathic normal pressure hydrocephalus: Preliminary results of a randomized clinical trial. Neurosurgery. 2013. 72: 845-53 discussion 853-4
16. Pranata R, Yonas E, Vania R, Rachmadian CV, July J. Preoperative third ventricle floor bowing is associated with increased surgical success rate in patients undergoing endoscopic third ventriculostomy-a systematic review and meta-analysis. Neurol India. 2022. 70: 664-9
17. Rangel-Castilla L, Barber S, Zhang YJ. The role of endoscopic third ventriculostomy in the treatment of communicating hydrocephalus. World Neurosurg. 2012. 77: 555-60
18. Sankey EW, Jusué-Torres I, Elder BD, Goodwin CR, Batra S, Hoffberger J. Functional gait outcomes for idiopathic normal pressure hydrocephalus after primary endoscopic third ventriculostomy. J Clin Neurosci. 2015. 22: 1303-8
19. Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JR. Hospital care for children with hydrocephalus in the United States: Utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr. 2008. 1: 131-7
20. Tasiou A, Brotis AG, Esposito F, Paterakis KN. Endoscopic third ventriculostomy in the treatment of idiopathic normal pressure hydrocephalus: A review study. Neurosurg Rev. 2016. 39: 557-63
21. Tudor KI, Tudor M, McCleery J, Car J. Endoscopic third ventriculostomy (ETV) for idiopathic normal pressure hydrocephalus (iNPH). Cochrane Database Syst Rev. 2015. 2015: CD010033
22. Yadav YR, Bajaj J, Ratre S, Yadav N, Parihar V, Swamy N. Endoscopic third ventriculostomy-a review. Neurol India. 2021. 69: 502-13