- Department of Neurosurgery, University of Caxias do Sul, Caxias do Sul, Rio Grande do Sul, Brazil.
Correspondence Address:
Asdrubal Falavigna, Department of Neurosurgery, University of Caxias do Sul, Caxias do Sul, Rio Grande do Sul, Brazil.
DOI:10.25259/SNI_220_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Matheus Machado Rech, Yan De Assunção Bicca, Miguel Bertelli Ramos, Murillo Cesar Gionedis, Arthur Aguzzoli, Asdrubal Falavigna. Knowledge, attitudes, and behaviors regarding the use of clinical practice guidelines among spine surgeons in Latin America. 15-Apr-2022;13:144
How to cite this URL: Matheus Machado Rech, Yan De Assunção Bicca, Miguel Bertelli Ramos, Murillo Cesar Gionedis, Arthur Aguzzoli, Asdrubal Falavigna. Knowledge, attitudes, and behaviors regarding the use of clinical practice guidelines among spine surgeons in Latin America. 15-Apr-2022;13:144. Available from: https://surgicalneurologyint.com/surgicalint-articles/11539/
Abstract
Background: Clinical Practice Guidelines (CPGs) are invaluable tools to assure evidence-based spine surgery care. In this study, we aimed to identify perceptions, barriers, and potential determinants for the use of CPG among Latin American spine surgeons.
Methods: A 28-item questionnaire regarding the use of CPGs was sent to the members of AO Spine Latin America. The questionnaire was subdivided into three sections: (1) demographic data; (2) perceptions and awareness of CPGs; (3) and potential barriers to CPG use. Multivariate logistic regression was performed to assess potential associations with CPG use.
Results: A total of 304 spine surgeons answered the questionnaire. Most of the participants were male (91.8%) and orthopedic spine surgeons (52.3%) who averaged 45–65 years of age. Most respondents were aware of some CPGs for spine care (68.8%) and reported using them (70.4%); lack of awareness about CPGs was the most frequent barrier to their use (65.1%).
Conclusion: Awareness of CPGs in spine surgery is of paramount importance for their use. Educational programs explaining the importance and benefits of spine care CPG surgical and clinical practice would increase the adherence of physicians to the guidelines.
Keywords: Evidence-based medicine, Guidelines, Neurosurgeon, Orthopedic surgeon, Spine
INTRODUCTION
Clinical Practice Guidelines (CPGs) provide the best available evidence for managing patients’ conditions and offer essential scientific information for the physician’s practice.[
MATERIALS AND METHODS
Type of study and questionnaire
The authors sent a cross-sectional survey to assess the adherence of Latin American spine surgeons to CPGs, as well as the facilitators and barriers to their utilization. The participation of the spine surgeons was voluntary and anonymous. The questionnaire comprised 28 questions, subdivided into three sections: (1) demographic data; (2) perceptions and awareness of CPGs; and (3) potential barriers to CPG use. The respective questions and their results are shown in [
Data analysis and statistics
We used SPSS Version 21. Continuous variables are presented as means (or medians) ± standard deviation (or quartile deviation) and their respective 95% confidence intervals (95% CI). Categorical variables are expressed as frequencies and percentages and analyzed using the Chi-square test.
Age (continuous), years of experience as spine surgeon (continuous), specialty (neurosurgery or orthopedics), and awareness of any CPG for spine care (yes or no) were the variables selected to undergo statistical analysis to assess potential associations. A significant P-value was set equal to or lower than 0.05.
RESULTS
General and demographic data
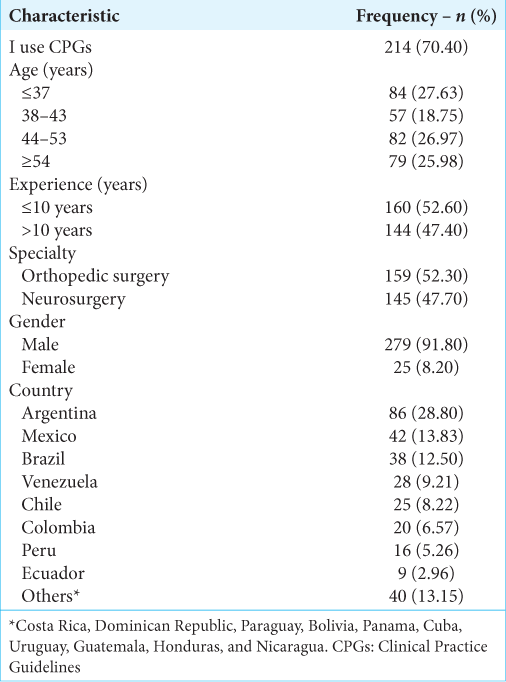
The response rate was 20.97% (n = 304/1450). Spine surgeons from 18 different countries answered the questionnaire. The countries with the highest number of respondents were Argentina (28.28%; n = 86/304), Mexico (13.81%; n = 42/304), and Brazil (12.50%; n = 38/304) [
Perceptions and awareness of CPGs
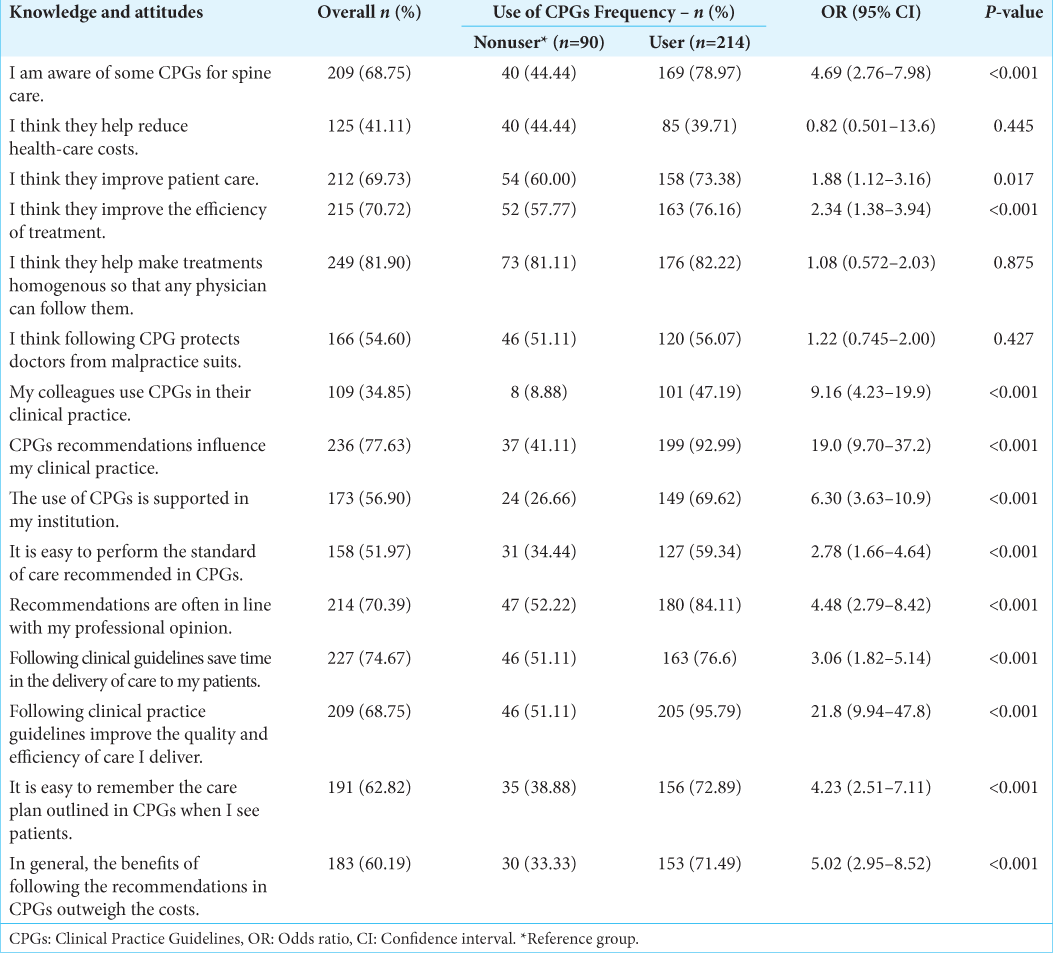
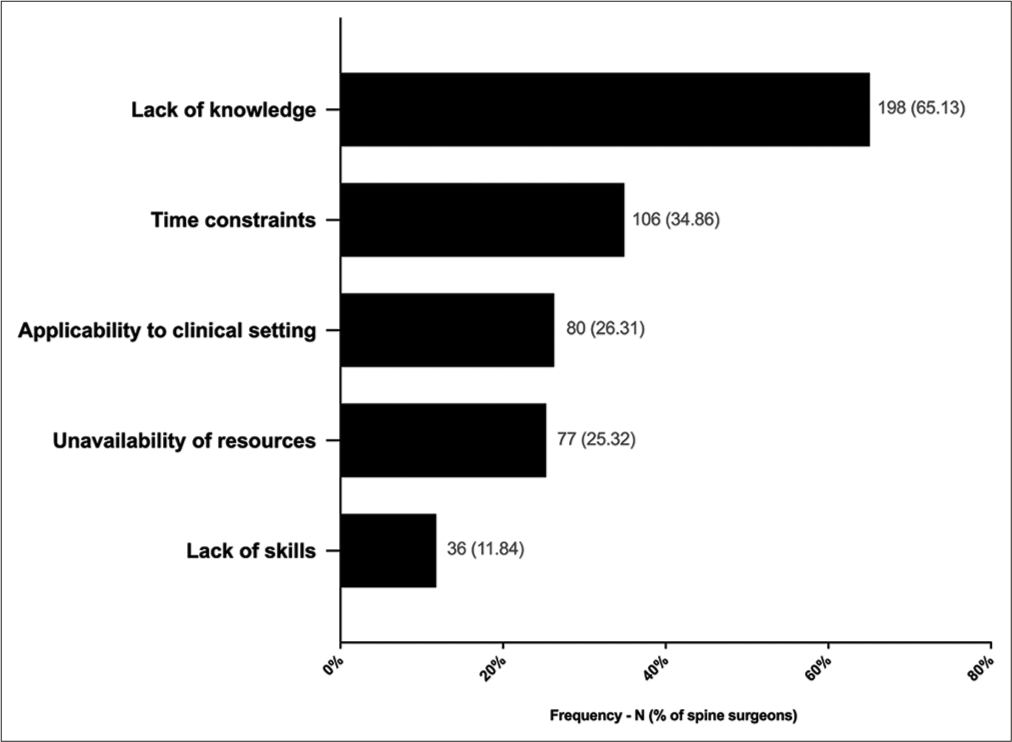
Most of the surgeons were aware of some CPGs for spine care (68.75%) and considered following CPGs as a protective measure for delivering better patient care (69.73%) and reducing health-care costs (60.19%). Lack of knowledge about CPGs was the most frequent barrier to their use (65.13%) followed by time constraints (34.86%) and applicability issues (31%). Further, data regarding perceptions and barriers are shown in [
Variables associated or not with guidelines use
The multivariate logistic regression model to forecast CPG use presented independent associations when they took it accounts for age (OR = 1.05, 95% CI = 0.99–1.10, P = 0.05), years of experience (OR = 0.93, 95% CI = 0.88–0.98; P = 0.007), specialty (OR = 2.07, 95% CI = 0.27–0.85, P = 0.013), and awareness (OR = 4.97, 95% CI = 2.87–8.58; P < 001).
DISCUSSION
We evaluated the perceptions and attitudes regarding CPGs among spine surgeons and potential barriers to their use. We found a strong association between awareness of CPGs and their use. Our findings can help future educational interventions to change the behavior of Latin America surgeons by spreading awareness of CPG use through educational programs to increase knowledge, foster critical appraisal, and alter attitudes. Although adherence to CPG-based decision-making in medicine represents an average of 67% of the decisions, it is estimated that 40% of the patients receive treatments that are not based on scientific evidence.[
CPGs do not decrease the incidence of malpractice suits or costs
Spine surgery predominates in number of malpractice suits in neurosurgery, comprising 40% of them.[
Behavioral aspects of CPGs adherence
Among the spine surgeons responding, 35.85% reported that their colleagues are CPG users and they also cited institutional support for using CPGs 56.90% of the time. Notably, there is a lack of evidence that financial incentives could improve guideline adherence.[
How to increase CPGs use among spine surgeons?
Continued education by local opinion leads only to a 6% minimal increase in the use of CPGs.[
There are specific ways to overcome the barriers of physicians’ awareness and attitudes. Spine surgeons’ attitudes can be improved by more opinion leaders’ recommendations, endorsement from specialty societies, educational meetings, outreach visits, and interactive learning.[
Furthermore, it needs to be emphasized that adherence to CPGs has clear benefits for the management of spine-related disease including also cost savings and improved quality of care.[
CONCLUSION
The awareness of CPGs is a key factor for guidelines use by Latin American spine surgeons to ensure up-to-date conducts and improved care of future patients.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Casey DE. Why don’t physicians (and patients) consistently follow clinical practice guidelines?. JAMA Intern Med. 2013. 173: 1581-3
2. de Macêdo Filho LJ, Aragão AC, Moura IA, Olivier LB, Albuquerque LA. Malpractice and socioeconomic aspects in neurosurgery: A developing-country reality. Neurosurg Focus. 2020. 49: E13
3. Falavigna A, Botelho RV, Teles AR, da Silva PG, Martins D, Guyot JP. Twelve years of scientific production on Medline by Latin American spine surgeons. PLoS One. 2014. 9: e87945
4. Fehlings MG, Nater A. Development and implementation of guidelines in neurosurgery. Neurosurg Clin N Am. 2015. 26: 271-82, x
5. Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation a scoping review. Healthcare (Basel). 2016. 4: E36
6. Grol R, Grimshaw J. From best evidence to best practice: Effective implementation of change in patients’ care. Lancet Lond Engl. 2003. 362: 1225-30
7. Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: Understanding time lags in translational research. J R Soc Med. 2011. 104: 510-20
8. Petersen LA, Simpson K, Pietz K, Urech TH, Hysong SJ, Profit J. Effects of individual physician-level and practice-level financial incentives on hypertension care: A randomized trial. JAMA. 2013. 310: 1042-50
9. Traeger AC, Buchbinder R, Elshaug AG, Croft PR, Maher CG. Care for low back pain: Can health systems deliver?. Bull World Health Organ. 2019. 97: 423-33
10. Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ trends and regional variations in lumbar spine surgery: 1992-2003. Spine. 2006. 31: 2707-14