- Departments of Neurosurgery, University, Via Conca, Ancona, Marche, Italy.
- Departments of Neurology, University, Via Conca, Ancona, Marche, Italy.
DOI:10.25259/SNI_85_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mauro Dobran, Fabrizio Mancini, Riccardo Paracino, Simona Lattanzi, Lucia di Somma, Davide Nasi, Gianluca Bizzocchi, Denis Aiudi, Maurizio Iacoangeli. Laminectomy versus open-door laminoplasty for cervical spondylotic myelopathy: A clinical outcome analysis. 18-Apr-2020;11:73
How to cite this URL: Mauro Dobran, Fabrizio Mancini, Riccardo Paracino, Simona Lattanzi, Lucia di Somma, Davide Nasi, Gianluca Bizzocchi, Denis Aiudi, Maurizio Iacoangeli. Laminectomy versus open-door laminoplasty for cervical spondylotic myelopathy: A clinical outcome analysis. 18-Apr-2020;11:73. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9964
Abstract
Background: Cervical spondylotic myelopathy (CSM) is one of the most common diseases in the geriatric population. Decompressive laminectomy or laminoplasty is the predominant surgical procedure of choice, but there remains debate as to which procedure is optimal for managing CSM.
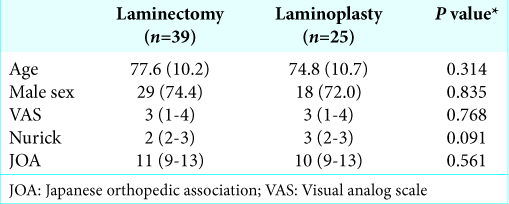
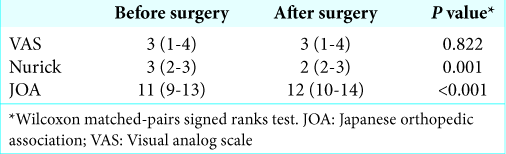
Methods: Here, we retrospectively analyzed 64 patients with CSM undergoing laminectomy (39 patients) versus laminoplasty (25 patients). The data were collected included respective Japanese orthopedic association (JOA) scores, Nurick grades, and Visual analog scale (VAS) values preoperatively versus 12 months postoperatively.
Results: The JOA score after 1 month improved in both groups utilizing laminectomy or laminoplasty. However, at 12 postoperative months, the JOA scores and Nurick grades showed greater improvement following laminoplasty, despite no differences in postoperative pain and complication rates.
Conclusion: Patients with cervical spondylotic myelopathy undergoing laminoplasty (25 patients) showed better 12-month postoperative outcomes (JOA scores and Nurick grades) versus those having laminectomies (39 patients).
Keywords: Cervical laminectomy, Cervical myelopathy, Cervical spondylotic myelopathy, Laminoplasty, Open- door technique, Spinal cord decompression
INTRODUCTION
Cervical spondylotic myelopathy (CSM) is the most common cause of nontraumatic spinal cord lesions in adults and geriatric patients.[
MATERIALS AND METHODS
We retrospectively reviewed the postoperative outcomes (Japanese orthopedic association [JOA] scores, Nurick grades, and Visual analog scale [VAS] scales) for 64 patients with CSM from 2015 to 2018 and MR/CT-documented cord compression. Patients averaged 74.8 years of age (range 57–87 years old) [
Clinical data
For these patients with CSM, 39 (60.9%) underwent cervical laminectomy without fusion, and 25 (39.1%) had open-door laminoplasty. The mean age of the study cohort was 76.4 and 47 (73.4%) of the patients were male [
Surgical techniques
Open-door laminoplasty versus laminectomy
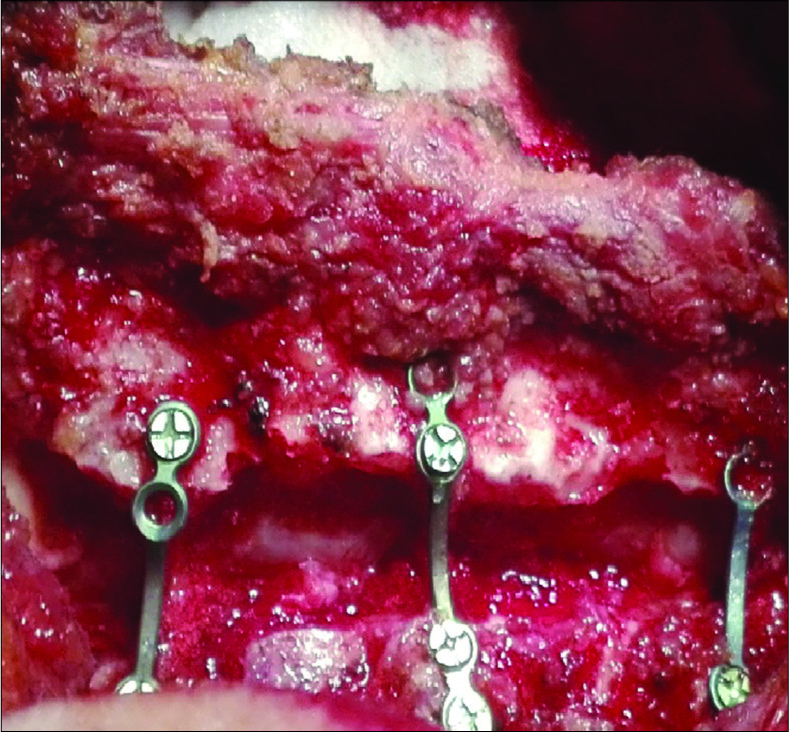
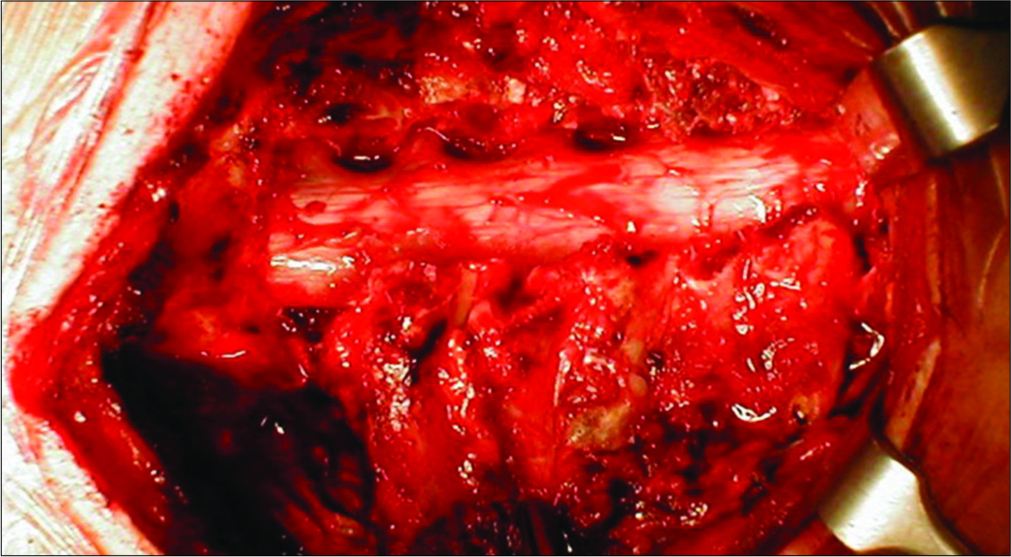
Twenty-five patients underwent the classic Hirabayashi open-door laminoplasty.[
Statistics
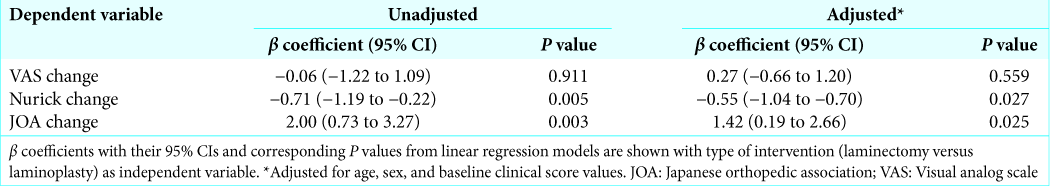
Values are presented as mean ± SD or median. Univariate comparisons were made through the Student’s t-test, Wilcoxon rank-sum test, or Chi-squared test. Changes in the scores obtained at 12 months after surgery were estimated using linear regression analysis. Data analysis was performed using STATA/IC 13.1 statistical package (StataCorp LP, Texas, USA).
RESULTS
Twelve-month postoperative scores JOA scores and Nurick grades were significantly improved for the 25 having open- door laminoplasty and 39 undergoing cervical laminectomy without fusion [
Complications
Postoperative complications occurred in 10 (15.6%) patients; five wound infections three new neurological deficits, one pulmonary embolism, and one case of pneumonia. There were no significant differences in the rates of other complications in the cervical laminectomy versus open-door laminoplasty groups (e.g., 18.0% versus 12%, respectively, P = 0.523).
DISCUSSION
Postoperative kyphosis and segmental instability after laminectomy are reported in from 6 to 47% of adults but in 100% of children.[
Literature
The literature demonstrates different pros and cons for laminoplasty versus laminectomy. The prospective AOSpine CSM – North America study involving 757 patients with CSM showed no difference in 1-year clinical outcomes between laminectomy with fusion versus laminoplasty (JOA scores of 2.45 and 2.51, respectively).[
The better clinical improvement seen in our series of 25 patients undergoing laminoplasty was based on the JOA score (not the Nurick grades), but there were no significant differences in the rates of pain improvement or complication.[
CONCLUSION
Our 25 patients with multilevel CSM undergoing laminoplasty showed better 12-month postoperative neurological outcomes based on significant improvement in JOA scores versus the 39 patients undergoing laminectomy without fusion.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Butler JC, Whitecloud TS. Postlaminectomy kyphosis. Causes and surgical management. Orthop Clin North Am. 1992. 23: 505-11
2. Casha S, Engelbrecht HA, DuPlessis SJ, Hurlbert RJ. Suspended laminoplasty for wide posterior cervical decompression and intradural access: Results, advantages, and complications. J Neurosurg Spine. 2004. 1: 80-6
3. Dobran M, Mancini F, Nasi D, Scerrati M. A case of deep infection after instrumentation in dorsal spinal surgery: The management with antibiotics and negative wound pressure without removal of fixation. BMJ Case Rep. 2017. 2017: 220792-
4. Fehlings MG, Barry S, Kopjar B, Yoon ST, Arnold P, Massicotte EM. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: Outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine (Phila Pa 1976). 2013. 38: 2247-52
5. Fehlings MG, Santaguida C, Tetreault L, Arnold P, Barbagallo G, Defino H. Laminectomy and fusion versus laminoplasty for the treatment of degenerative cervical myelopathy: results from the AOSpine North America and international prospective multicenter studies. Spine J. 2017. 17: 102-8
6. Heller JG, Edwards CC, Murakami H, Rodts GE. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: An independent matched cohort analysis. Spine (Phila Pa 1976). 2001. 26: 1330-6
7. Herkowitz HN. A comparison of anterior cervical fusion, cervical laminectomy, and cervical laminoplasty for the surgical management of multiple level spondylotic radiculopathy. Spine (Phila Pa 1976). 1988. 13: 774-80
8. Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981. 6: 354-64
9. Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. 2000. 93: 199-204
10. Lau D, Winkler EA, Than KD, Chou D, Mummaneni PV. Laminoplasty versus laminectomy with posterior spinal fusion for multilevel cervical spondylotic myelopathy: Influence of cervical alignment on outcomes. J Neurosurg Spine. 2017. 27: 508-17
11. Manzano GR, Casella G, Wang MY, Vanni S, Levi AD. A prospective, randomized trial comparing expansile cervical laminoplasty and cervical laminectomy and fusion for multilevel cervical myelopathy. Neurosurgery. 2012. 70: 264-77
12. Matsunaga S, Sakou T, Nakanisi K. Analysis of the cervical spine alignment following laminoplasty and laminectomy. Spinal Cord. 1999. 37: 20-4
13. Nurboja B, Kachramanoglou C, Choi D. Cervical laminectomy vs laminoplasty: Is there a difference in outcome and postoperative pain?. Neurosurgery. 2012. 70: 965-70
14. Petraglia AL, Srinivasan V, Coriddi M, Whitbeck MG, Maxwell JT, Silberstein HJ. Cervical laminoplasty as a management option for patients with cervical spondylotic myelopathy: A series of 40 patients. Neurosurgery. 2010. 67: 272-7
15. Revanappa KK, Rajshekhar V. Comparison of nurick grading system and modified Japanese orthopaedic association scoring system in evaluation of patients with cervical spondylotic myelopathy. Eur Spine J. 2011. 20: 1545-51
16. Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2003. 28: 1258-62
17. Yang L, Gu Y, Shi J, Gao R, Liu Y, Li J. Modified plate-only open-door laminoplasty versus laminectomy and fusion for the treatment of cervical stenotic myelopathy. Orthopedics. 2013. 36: e79-87
18. Yoon ST, Hashimoto RE, Raich A, Shaffrey CI, Rhee JM, Riew KD. Outcomes after laminoplasty compared with laminectomy and fusion in patients with cervical myelopathy: A systematic review. Spine (Phila Pa 1976). 2013. 38: S183-94