- Department of Neurosurgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, USA
- Department of Neurosurgery, Kaleida Health, Buffalo, New York, USA
Correspondence Address:
Vassilios G. Dimopoulos
Department of Neurosurgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, USA
Department of Neurosurgery, Kaleida Health, Buffalo, New York, USA
DOI:10.4103/2152-7806.191073
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Siasios ID, Vakharia K, Gibbons KJ, Dimopoulos VG. Large, spontaneous spinal subdural–epidural hematoma after epidural anesthesia for caesarean section: Conservative management with excellent outcome. Surg Neurol Int 22-Sep-2016;7:
How to cite this URL: Siasios ID, Vakharia K, Gibbons KJ, Dimopoulos VG. Large, spontaneous spinal subdural–epidural hematoma after epidural anesthesia for caesarean section: Conservative management with excellent outcome. Surg Neurol Int 22-Sep-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/large-spontaneous-spinal-subdural-epidural-hematoma-epidural-anesthesia-caesarean-section-conservative-management-excellent-outcome/
Abstract
Background:Iatrogenic or spontaneous spinal hematomas are rarely seen and present with multiple symptoms that can be difficult to localize. Most spontaneous spinal hematomas are multifactorial, and the pathophysiology is varied. Here, we present a case of a scattered, multicomponent, combined subdural and epidural spinal hematoma that was managed conservatively.
Case Description:A 38-year-old woman came to the emergency department (ED) complaining of severe neck and back pain. She had undergone a caesarean section under epidural anesthesia 4 days prior to her arrival in the ED. She was placed on heparin and then warfarin to treat a pulmonary embolism that was diagnosed immediately postpartum. Her neurological examination at presentation demonstrated solely the existence of clonus in the lower extremities and localized cervical and low thoracic pain. In the ED, the patient's international normalized ratio was only mildly elevated. Spinal magnetic resonance imaging revealed a large thoracolumbar subdural hematoma with some epidural components in the upper thoracic spine levels. Spinal cord edema was also noted at the T6-T7 vertebral level. The patient was admitted to the neurosurgical intensive care unit for close surveillance and reversal of her coagulopathy. She was treated conservatively with pain medication, fresh frozen plasma, and vitamin K. She was discharged off of warfarin without any neurological deficit.
Conclusions:Conservative management of spinal hematomas secondary to induced coagulopathies can be effective. This case suggests that, in the face of neuroimaging findings of significant edema and epidural blood, the clinical examination should dictate the management, especially in such complicated patients.
Keywords: Caesarean section, hematoma, intensive care unit, subdural–epidural
INTRODUCTION
Post-traumatic, iatrogenic or spontaneous spinal hematomas (epidural and/or subdural) are rare and have different pathophysiological causes. Several factors contribute to the genesis of a spinal hematoma, such as vascular malformations, coagulopathies, thrombolytic drug administration, tumors, autoimmune diseases, pregnancy, excessive exercise, previous epidural anesthesia, cardiac surgery, and lumbar puncture.[
Here, we present a rare case of a large multicomponent, combined epidural and subdural spinal hematoma extending from the cervical spine to the low thoracic spine that was treated conservatively.
CASE DESCRIPTION
History
A 38-year-old woman who had recently undergone epidural spinal anesthesia for a caesarean section 4 days prior presented to the emergency department (ED) of our institute complaining of severe neck and low back pain. Postpartum, her postoperative course was complicated by dyspnea and chest pain that was found to be secondary to a new pulmonary embolism. During her initial hospitalization, she received antithrombotic therapy sustained by unfractionated heparin (with close monitoring of her clotting mechanism) and was bridged to warfarin therapy prior to her discharge to home. At the ED, she did not have any weakness, paresthesias, or changes in motor “function,” although she described some nonspecific back pain.
Examination
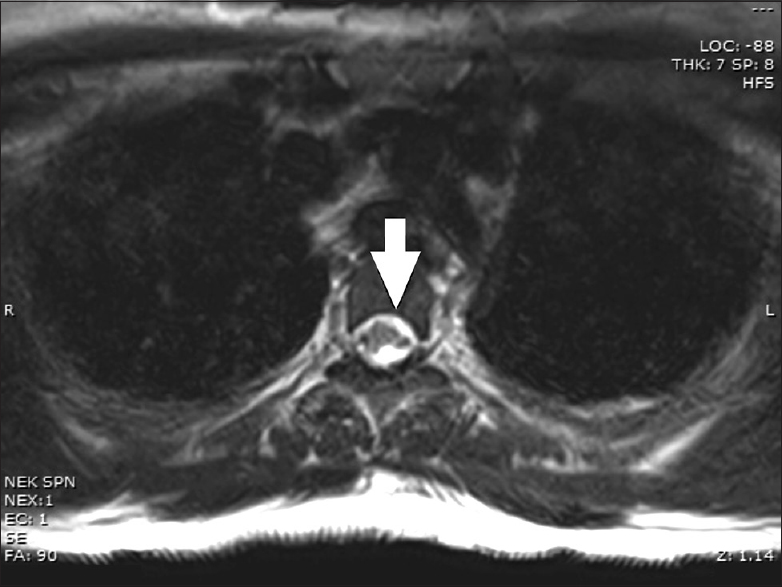
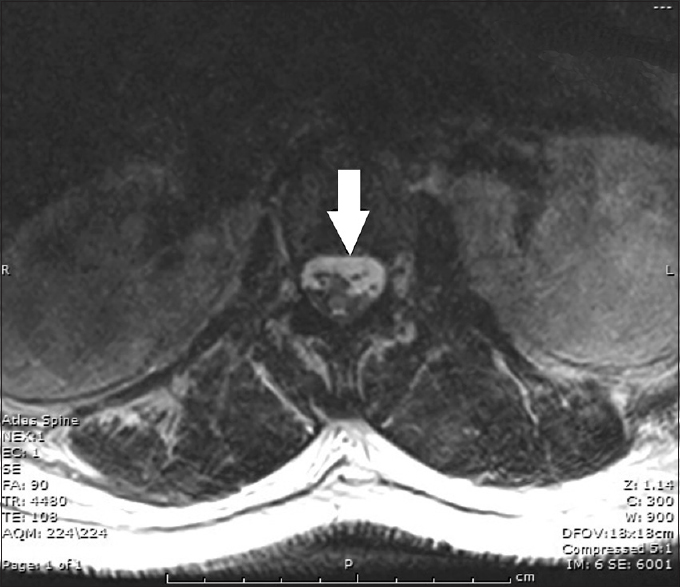
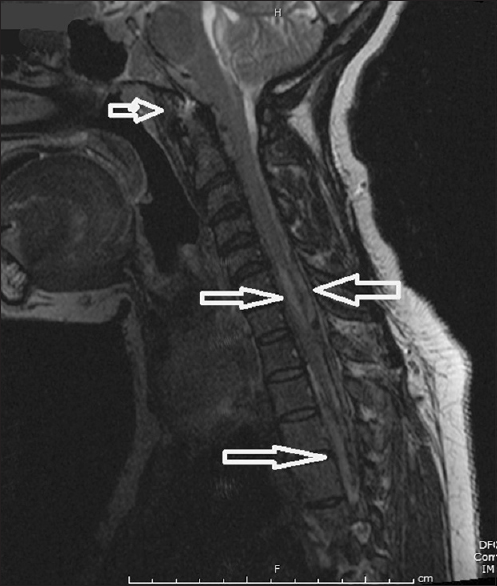
On examination in the ED, the patient had 5/5 strength in all muscle groups in the upper and lower extremities, no signs of sensory deficits, or signs of cauda equina syndrome, but she did have several beats of clonus in the lower extremities. Laboratory testing demonstrated only a mildly elevated international normalized ratio of 1.8, which was below the expected value. Magnetic resonance imaging (MRI) of the entire spine demonstrated a large amount of mixed epidural and subdural blood collection within the high thoracic and lumbar spine as well as cord edema near T6-7 [Figures
Figure 1
Thoracic magnetic resonance imaging (MRI), sagittal T2 sequence with contrast enhancement, showing extra-axial subdural abnormality involving the entirety of the thoracic spinal canal extending from the cervical to the lumbar spine (small arrows). Minor signal within the spinal cord parenchyma is most likely associated with edema (large arrow). These findings were consistent with extensive acute/subacute subdural–epidural hemorrhage
Figure 4
Cervical MRI, sagittal T2 sequence without contrast enhancement, showing an extensive extra-axial hematoma initiating from the prepontine premedullary cistern to the upper thoracic spine (left arrows). At the C6-C7 level, a pathological signal is noted within the spinal cord parenchyma with minor mass effect (right arrow)
Hospital course
After the diagnosis was made, the patient was admitted to the neurosurgical intensive care unit (neuroICU) for reversal of her mild coagulopathy (due to previous warfarin therapy) with the administration of fresh frozen plasma and vitamin K, as well as for pain control and surveillance. While in the neuroICU, she experienced an episode of tachycardia and shortness of breath for which she underwent thoracic computed tomographic angiography, which showed a small right basilar atelectasis. These symptoms were thought to be due to a transfusion reaction to the plasma and vitamin K. She was treated conservatively with pain control management and bedrest. After gradual mobilization, she was discharged without any neurological deficits or complications. Her atelectasis and pain were resolved; the hematoma had stabilized according to the last imaging study performed during her hospitalization. The last MRI study, obtained 9 months after her discharge, showed that the hematoma is slowly resolving. The patient is neurologically stable and is completely mobile, although she is still having episodes of low back pain and wears a brace for comfort.
DISCUSSION
Although many cases of spinal subdural or epidural hematomas have been described in the literature, this case is unique because it is a case of a mixed hematoma that was successfully managed conservatively. Although epidural anesthesia is a commonly used means of anesthesia, it can be associated with serious complications in 0.1–1 per 10000 epidural injections.[
The treatment of spinal subdural, epidural, or combination hematomas may be conservative or surgical, although the borders between these two options are sometimes subjective.[
Given our patient's recovery, we believe that clinical examination findings should dictate the management for such patients. Imaging findings, such as size of the hematoma, should never be used as the only guide for treatment strategizing.[
Author contributions
Concept and design: Dimopoulos, Siasios; Acquisition of data: Siasios, Vakharia; Analysis and interpretation of data: all authors; Drafting the manuscript: Siasios, Vakharia; Critically revising the manuscript: all authors; Final approval of the manuscript: all authors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank Paul H. Dressel BFA for preparation of the illustrations and Debra J. Zimmer for editorial assistance.
References
1. Badar F, Kirmani S, Rashid M, Azfar SF, Yasmeen S, Ullah E. Spontaneous spinal epidural hematoma during pregnancy: A rare obstetric emergency. Emerg Radiol. 2011. 18: 433-6
2. Buchanan CC, Lu DC, Buchanan C, Tran TT. Spontaneous spinal epidural hematoma and spinal cord infarction following orthotopic liver transplantation: Case report and review of the literature. Surg Neurol Int. 2013. 4: S359-61
3. Cabral AJ, Barros A, Aveiro C, Vasconcelos R. Spontaneous spinal epidural haematoma due to arteriovenous malformation in a child. BMJ Case Rep 2011. 2011. p.
4. Caruso G, Galarza M, Borghesi I, Pozzati E, Vitale M. Acute presentation of spinal epidural cavernous angiomas: Case report. Neurosurgery. 2007. 60: E575-6
5. Chen CL, Lu CH, Chen NF. Spontaneous spinal epidural hematoma presenting with quadriplegia after sit-ups exercise. Am J Emerg Med. 2009. 27: 1170 e3-7
6. Connolly ES, Winfree CJ, McCormick PC. Management of spinal epidural hematoma after tissue plasminogen activator. A case report. Spine. 1996. 21: 1694-8
7. Deger SM, Emmez H, Bahadirli K, Kale A, Ebinc FA, Turkoglu M. A spontaneous spinal epidural hematoma in a hemodialysis patient: A rare entity. Intern Med. 2009. 48: 2115-8
8. Doymaz S, Schneider J. Spontaneous spinal epidural hematoma in a teenage boy with cholestasis: A case report. Pediatr Emerg Care. 2013. 29: 227-9
9. Dziedzic T, Kunert P, Krych P, Marchel A. Management and neurological outcome of spontaneous spinal epidural hematoma. J Clin Neurosci. 2015. 22: 726-9
10. Fleager K, Lee A, Cheng I, Hou L, Ryu S, Boakye M. Massive spontaneous epidural hematoma in a high-level swimmer: A case report. J Bone Joint Surg Am. 2010. 92: 2843-6
11. Foo D, Rossier AB. Preoperative neurological status in predicting surgical outcome of spinal epidural hematomas. Surg Neurol. 1981. 15: 389-401
12. Garcia Lopez A, Perez Lara JM, Herrainz Hidalgo R, Puente Gonzalo E. Spinal epidural hematoma following thrombolytic therapy for acute myocardial infarction. Orthopedics. 1999. 22: 987-8
13. Groen RJ, van Alphen HA. Operative treatment of spontaneous spinal epidural hematomas: A study of the factors determining postoperative outcome. Neurosurgery. 1996. 39: 494-508
14. Hentschel SJ, Woolfenden AR, Fairholm DJ. Resolution of spontaneous spinal epidural hematoma without surgery: Report of two cases. Spine. 2001. 26: E525-7
15. Hosoki K, Kumamoto T, Kasai Y, Sakata K, Ito M, Iwamoto S. Infantile spontaneous spinal epidural hematoma. Pediatr Int. 2010. 52: 507-8
16. Hutt PJ, Herold ED, Koenig BM, Gilchrist GS. Spinal extradural hematoma in an infant with hemophilia A: An unusual presentation of a rare complication. J Pediatr. 1996. 128: 704-6
17. Kiehna EN, Waldron PE, Jane JA. Conservative management of an acute spontaneous holocord epidural hemorrhage in a hemophiliac infant. J Neurosurg Pediatr. 2010. 6: 43-8
18. Kin H, Mukaida M, Koizumi J, Kamada T, Mitsunaga Y, Iwase T. Spontaneous spinal epidural hematoma presenting as paraplegia after cardiac surgery. Gen Thorac Cardiovasc Surg. 2016. 64: 153-5
19. Kitamura Y, Onozuka S, Ichimura S, Yoshida K. Spontaneous spinal epidural hematoma (SSEH) after coil embolization of cerebral aneurysm: Implication of high SSEH frequency in East Asia. Clin Neurol Neurosurg. 2013. 115: 649-50
20. Kivity S, Rajz G, Segal G, Merkel D, Sidi Y. Spontaneous spinal epidural hematoma as the initial presentation of polycythemia vera. Acta Haematol. 2010. 123: 34-6
21. Liao CC, Lee ST, Hsu WC, Chen LR, Lui TN, Lee SC. Experience in the surgical management of spontaneous spinal epidural hematoma. J Neurosurg. 2004. 100: 38-45
22. Lim SH, Hong BY, Cho YR, Kim HS, Lee JI, Kim HW. Relapsed spontaneous spinal epidural hematoma associated with aspirin and clopidogrel. Neurol Sci. 2011. 32: 687-9
23. Muhonen MG, Piper JG, Moore SA, Menezes AH. Cervical epidural hematoma secondary to an extradural vascular malformation in an infant: Case report. Neurosurgery. 1995. 36: 585-7
24. Nakanishi K, Nakano N, Uchiyama T, Kato A. Hemiparesis caused by cervical spontaneous spinal epidural hematoma: A report of 3 cases. Adv Orthop 2011. 2011. p. 516382-
25. Narawong D, Gibbons VP, McLaughlin JR, Bouhasin JD, Kotagal S. Conservative management of spinal epidural hematoma in hemophilia. Pediatr Neurol. 1988. 4: 169-71
26. Pahapill PA, Lownie SP. Conservative treatment of acute spontaneous spinal epidural hematoma. Can J Neurol Sci. 1998. 25: 159-63
27. Persson J, Flisberg P, Lundberg J. Thoracic epidural anesthesia and epidural hematoma. Acta Anaesthesiol Scand. 2002. 46: 1171-4
28. Sandvik U, Svensdotter E, Gustavsson B. Spinal cavernous extradural angiolipoma manifesting as a spontaneous spinal epidural hematoma in a child. Childs Nerv Syst. 2015. 31: 1223-6
29. Sheikh AA, Abildgaard CF. Medical management of extensive spinal epidural hematoma in a child with factor IX deficiency. Pediatr Emerg Care. 1994. 10: 26-9
30. Singh DP, Lamtha SC, Kumar S. Spontaneous spinal epidural haematoma during pregnancy. J Assoc Physicians India. 2009. 57: 540-2
31. Sirin S, Arslan E, Yasar S, Kahraman S. Is spontaneous spinal epidural hematoma in elderly patients an emergency surgical case?. Turk Neurosurg. 2010. 20: 557-60
32. Snarr J. Risk, benefits and complications of epidural steroid injections: A case report. AANA J. 2007. 75: 183-8
33. Solero CL, Fornari M, Savoiardo M. Spontaneous spinal epidural haematoma arising from ruptured vascular malformation. Case report. Acta Neurochir. 1980. 53: 169-74
34. Subbiah M, Avadhani A, Shetty AP, Rajasekaran S. Acute spontaneous cervical epidural hematoma with neurological deficit after low-molecular-weight heparin therapy: Role of conservative management. Spine J. 2010. 10: e11-5
35. Tawk C, El Hajj Moussa M, Zgheib R, Nohra G. Spontaneous epidural hematoma of the spine associated with oral anticoagulants: 3 Case Studies. Int J Surg Case Rep. 2015. 13: 8-11
36. Tremolizzo L, Patassini M, Malpieri M, Ferrarese C, Appollonio I. A case of spinal epidural haematoma during breath-hold diving. Diving Hyperb Med. 2012. 42: 98-100
37. Ulivieri S, Oliveri G. Spinal epidural hematoma following epidural anesthesia. Case report. G Chir. 2009. 30: 51-2
38. Walters MA, Van de Velde M, Wilms G. Acute intrathecal haematoma following neuraxial anaesthesia: Diagnostic delay after apparently normal radiological imaging. Int J Obstet Anesth. 2012. 21: 181-5