- Department of Neurosurgery, University of Toyama, Toyama, Japan.
- Department of Pediatrics, University of Toyama, Toyama, Japan.
- Department of Radiology, University of Toyama, Toyama, Japan.
Correspondence Address:
Satoshi Kuroda, Department of Neurosurgery, University of Toyama, Toyama, Japan.
DOI:10.25259/SNI_828_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shunsuke Hasegawa1, Tomomi Tanaka2, Shusuke Yamamoto1, Daina Kashiwazaki1, Kyo Noguchi3, Satoshi Kuroda1. Late-onset, first-ever involuntary movement after successful surgical revascularization for pediatric moyamoya disease – Report of two cases. 15-Dec-2023;14:430
How to cite this URL: Shunsuke Hasegawa1, Tomomi Tanaka2, Shusuke Yamamoto1, Daina Kashiwazaki1, Kyo Noguchi3, Satoshi Kuroda1. Late-onset, first-ever involuntary movement after successful surgical revascularization for pediatric moyamoya disease – Report of two cases. 15-Dec-2023;14:430. Available from: https://surgicalneurologyint.com/surgicalint-articles/12670/
Abstract
Background: A small number of children with Moyamoya disease develop involuntary movements as an initial presentation at the onset, which usually resolves after effective surgical revascularization. However, involuntary movements that did not occur at the onset first occur after surgery in very rare cases. In this report, we describe two pediatric cases that developed involuntary movements during the stable postoperative period after successful surgical revascularization.
Case Description: A 10-year-old boy developed an ischemic stroke and successfully underwent combined bypass surgery. However, he developed chorea six months later. Another 8-year-old boy developed a transient ischemic attack and successfully underwent combined bypass surgery. However, he developed chorea three years later. In both cases, temporary use of haloperidol was quite effective in resolving the symptoms, and involuntary movements did not recur without any medication during follow-up periods of up to 10 years.
Conclusion: Postoperative first-ever involuntary movement is very rare in pediatric moyamoya disease, and the underlying mechanisms are still unclear, but a temporary, reversible imbalance of excitatory and inhibitory circuits in the basal ganglia may trigger the occurrence of these rare symptoms. Careful follow-up would be mandatory.
Keywords: Bypass surgery, Haloperidol, Involuntary movement, Late-onset, Moyamoya disease
INTRODUCTION
In pediatric moyamoya disease, involuntary movements are known to occur very rarely as the initial presentation, but the underlying mechanisms are still obscure.[
We herein report two pediatric cases that developed chorea during the stable postoperative period after successful cerebral revascularization. Temporary use of haloperidol was quite effective in resolving the symptoms.
CASE PRESENTATION
Case 1
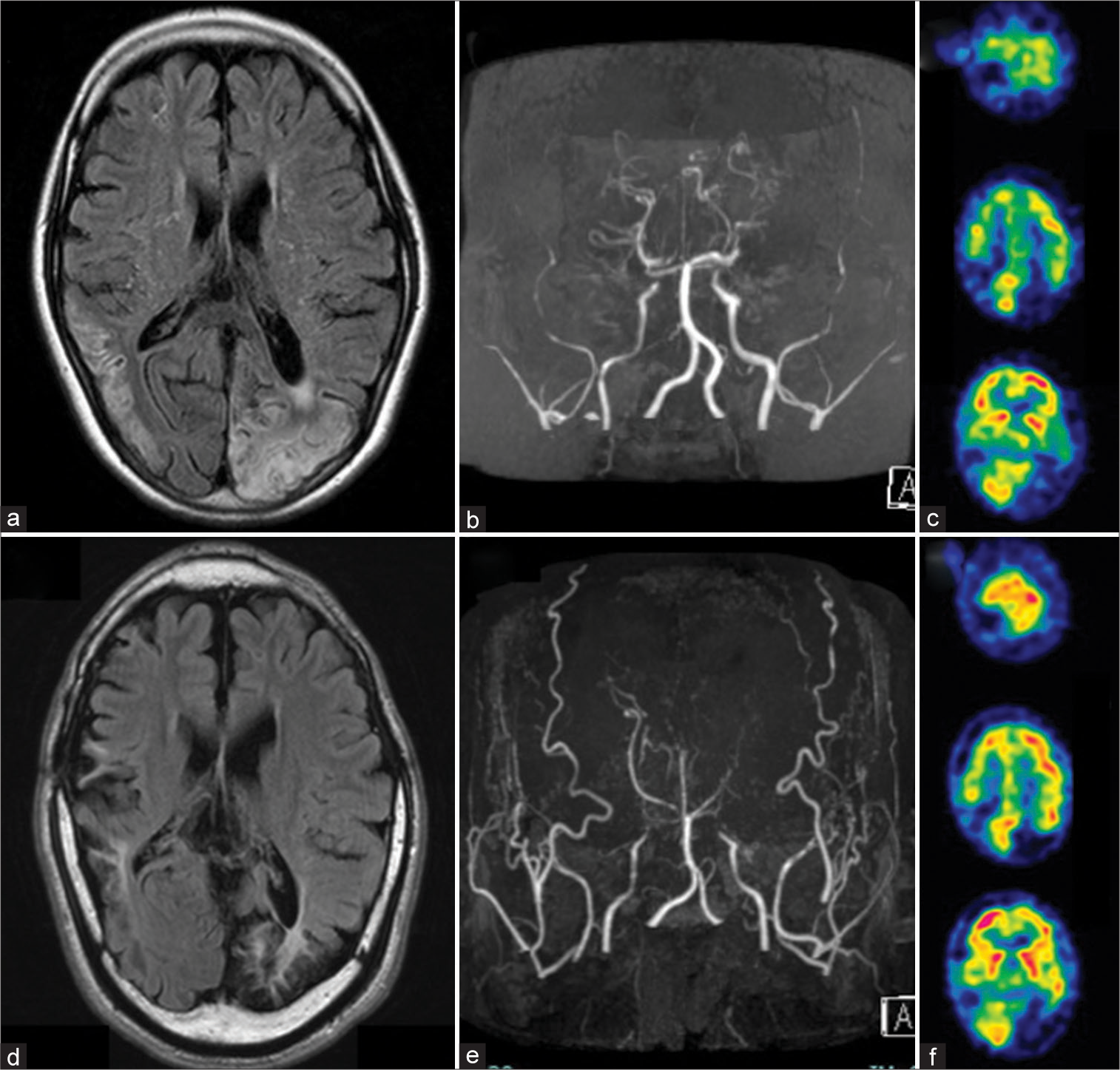
A 10-year-old boy suddenly developed visual field disturbance and cognitive dysfunction and was diagnosed with Moyamoya disease. Neurological examination on admission revealed right homonymous hemianopsia, sensory aphasia, apraxia, and agnosia. Brain magnetic resonance imaging (MRI) showed multiple infarctions in the bilateral deep frontal lobes and cortical infarction in the left occipital lobe and right temporoparietal lobes. Brain magnetic resonance angiography (MRA) demonstrated severe stenosis in the terminal portion of the internal carotid arteries (ICAs) and the posterior cerebral arteries on both sides. Single-photon emission computed tomography (SPECT) showed reduced cerebral blood flow (CBF) in the bilateral cerebral hemispheres [
Figure 1:
Pre- (a-c) and postoperative (d-f) radiological findings of case 1. (a) Fluid-attenuated inversion recovery (FLAIR) image demonstrated small cerebral infarction in the bilateral deep frontal lobes, the left occipital lobe, and the right temporoparietal lobes. (b) Magnetic resonance angiography (MRA) showed severe stenosis of the terminal portion of the internal carotid arteries and the posterior cerebral arteries on both sides. (c) Blood flow study demonstrated a marked decrease in cerebral blood flow (CBF) on both sides. (d) Postoperative FLAIR image showed no newly developed cerebral infarction. (e) Postoperative MRA showed a marked increase in the caliber of superficial temporal arteries, middle meningeal arteries, and deep temporal arteries on both sides, indicating the sufficient development of surgical collaterals through direct and indirect bypass procedures. (f) Postoperative single-photon emission computed tomography demonstrated sufficient improvement of CBF in the vital tissues except for cerebral infarction.
Six months after surgery, however, he developed involuntary movements in the tongue and left extremities. The involuntary movements were sustained and very similar to the chorea. Brain MRI/MRA showed no new abnormalities. He was treated with clonazepam for ten days, but his symptoms did not improve. Then, he was treated with haloperidol (1.5 mg/day); after that, his symptoms gradually improved and completely disappeared after one month. Although haloperidol was tapered and discontinued, involuntary movements have not recurred for ten years.
Case 2
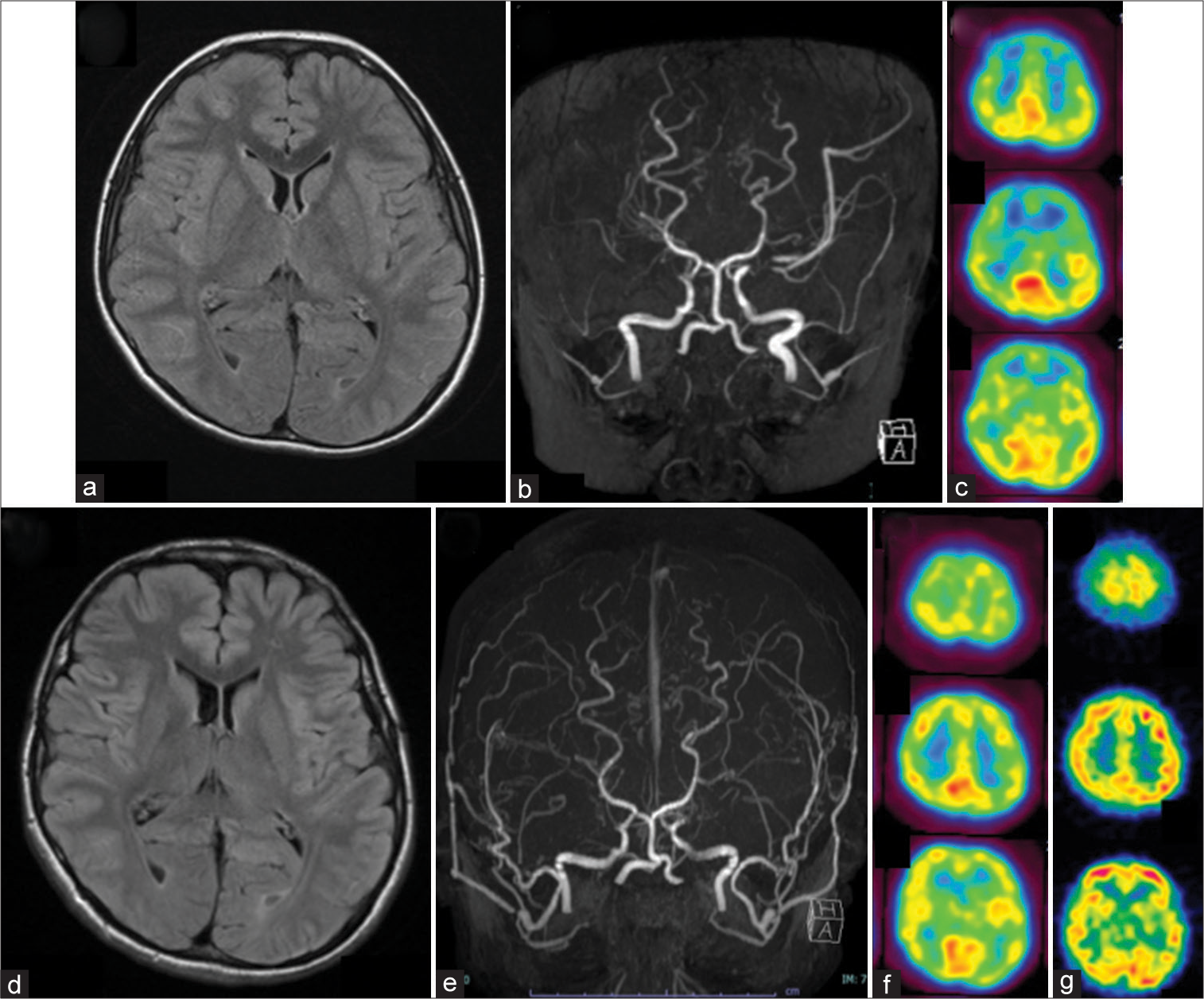
An 8-year-old boy developed a headache attack on the right side and transient weakness of the left extremities and was diagnosed with Moyamoya disease. Neurological examination on admission revealed no abnormalities. Brain MRI showed no parenchymal lesions. Brain MRA showed severe stenosis of the terminal portion of the ICAs on both sides. Brain SPECT showed a marked CBF decrease in the territories of the bilateral cerebral hemispheres, especially in the frontal lobes [
Figure 2:
Pre- (a-c) and postoperative (d-f) radiological findings of case 2. (a) Fluid-attenuated inversion recovery (FLAIR) image demonstrated no parenchymal lesions. (b) Magnetic resonance angiography (MRA) showed severe stenosis of the terminal portion of the internal carotid arteries (ICAs) on both sides. (c) A blood flow study demonstrated a marked decrease in cerebral blood flow (CBF) in the territory of the ICA, especially in the frontal lobes on both sides. (d) Postoperative FLAIR image showed no newly developed cerebral infarction. (e) Postoperative MRA showed a marked increase in the caliber of superficial temporal arteries, middle meningeal arteries, and deep temporal arteries on both sides, indicating the sufficient development of surgical collaterals through direct and indirect bypass procedures. (f) Postoperative single-photon emission computed tomography demonstrated sufficient improvement of CBF on both sides. (g) A blood flow study at the onset of involuntary movements revealed no abnormal distribution of CBF.
Three years after surgery, however, he developed chorea-like involuntary movements in the neck and left extremities. Brain MRI/MRA showed no new abnormalities. Blood flow measurement demonstrated a normal distribution of CBF [
DISCUSSION
According to the previous reports, 3–6% of moyamoya children present with involuntary movements as an initial symptom. A majority of involuntary movements are chorea, but some patients develop dystonia or dyskinesia.[
In this report, we describe two children who first developed involuntary movements six months or three years after successful surgical revascularization. In both cases, there were no episodes of involuntary movements before surgery, indicating that involuntary movements emerged for the 1st time several months or years after surgery. Chorea-like involuntary movements occurred in the tongue and unilateral limbs in one case and the neck and unilateral limbs in another. Their postoperative course was uneventful, and cerebrovascular events had completely resolved after surgery. Follow-up radiological examinations several months after surgery showed a marked improvement in cerebral hemodynamics in response to the well-developed surgical collaterals.
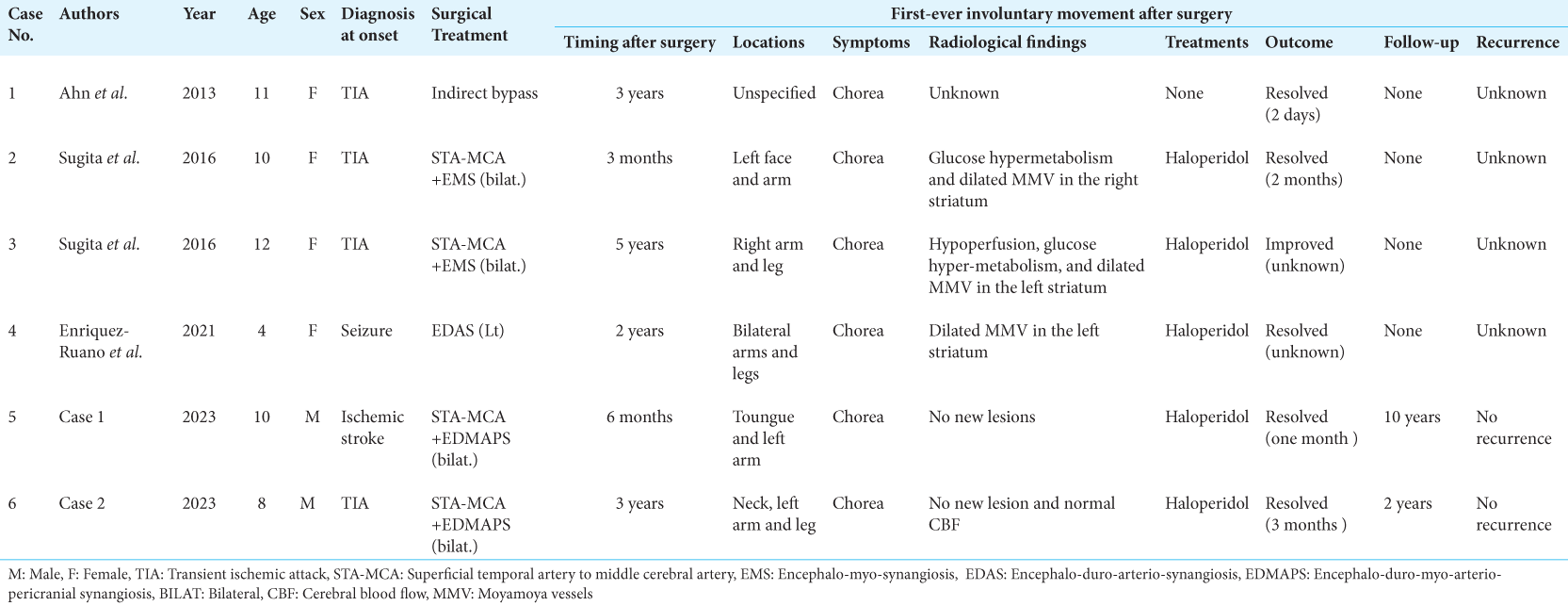
To the best of our knowledge, there are only four similar cases in the literature. Thus, the late-onset, first-ever involuntary movement in pediatric moyamoya disease would be quite rare.[
In five of the six cases, radiological findings were described at the onset of postoperative involuntary movements, and no new lesions were not found on MRI. Therefore, the newly developed cerebral infarction or hemorrhage is unlikely to be the cause of these rare symptoms. Sugita et al. found reduced CBF in the unilateral basal ganglia,[
In one of the six patients, the involuntary movements resolved spontaneously, whereas haloperidol was effective in completely resolving it in the other five cases.[
In the four cases reported previously, there is no description about whether the involuntary movements recurred during follow-up periods or not. In our two cases, however, the symptoms did not recur when they were followed for 2–10 years, although haloperidol was discontinued. The fact strongly suggests that the late-onset, first-ever involuntary movements after surgery for moyamoya disease may result from a temporary, reversible dysfunction of the extrapyramidal system. Since this extremely rare symptom has only occurred in children but not in adults, it may involve some kinds of pediatric-specific pathophysiology.
CONCLUSION
Late-onset, first-ever involuntary movements after surgery are quite rare in pediatric moyamoya disease. The underlying mechanisms are still unclear, but a temporary, reversible imbalance of excitatory and inhibitory circuits in the basal ganglia may trigger the occurrence of these rare symptoms. It is quite important to carefully follow up with pediatric patients for a long time, even after successful surgical revascularization.
Ethical approval
Not applicable.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
The Ministry of Health, Labor and Welfare of Japan.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
This study was partly supported by a grant from the Research Committee on Moyamoya Disease, sponsored by the Ministry of Health, Labor and Welfare of Japan (Grant No. 23FC101).
References
1. Ahn ES, Scott RM, Robertson RL, Smith ER. Chorea in the clinical presentation of moyamoya disease: Results of surgical revascularization and a proposed clinicopathological correlation. J Neurosurg Pediatr. 2013. 11: 313-9
2. Baik JS, Lee MS. Movement disorders associated with moyamoya disease: A report of 4 new cases and a review of literatures. Mov Disord. 2010. 25: 1482-6
3. Bhatia KP, Marsden CD. The behavioural and motor consequences of focal lesions of the basal ganglia in man. Brain. 1994. 117: 859-76
4. Enriquez-Ruano P, Navarro CE, Penagos N, Espitia OM. Late-onset chorea after cerebral revascularization as a clinical manifestation of moyamoya disease. Neurol Sci. 2021. 42: 3027-30
5. Gonzalez-Alegre P, Ammache Z, Davis PH, Rodnitzky RL. Moyamoya-induced paroxysmal dyskinesia. Mov Disord. 2003. 18: 1051-6
6. Koga Y, Kashiwazaki D, Hori E, Akioka N, Kuroda S. Oromandibular dystonia in pediatric moyamoya disease: Two cases report. Surg Neurol Int. 2021. 12: 449
7. Kuroda S, Houkin K, Ishikawa T, Nakayama N, Iwasaki Y. Novel bypass surgery for moyamoya disease using pericranial flap: Its impacts on cerebral hemodynamics and long-term outcome. Neurosurgery. 2010. 66: 1093-101 discussion 1101
8. Kuroda S, Houkin K. Moyamoya disease: Current concepts and future perspectives. Lancet Neurol. 2008. 7: 1056-66
9. Kuroda S, Nakayama N, Yamamoto S, Kashiwazaki D, Uchino H, Saito H. Late (5-20 years) outcomes after STA-MCA anastomosis and encephalo-duro-myo-arteriopericranial synangiosis in patients with moyamoya disease. J Neurosurg. 2020. 134: 909-16
10. Lee JY, Kim SK, Wang KC, Chae JH, Cheon JE, Choi JW. Involuntary movement in pediatric moyamoya disease patients: Consideration of pathogenetic mechanism using neuroimaging studies. Childs Nerv Syst. 2014. 30: 885-90
11. Park J. Movement disorders following cerebrovascular lesion in the basal ganglia circuit. J Mov Disord. 2016. 9: 71-9
12. Ristic A, Marinkovic J, Dragasevic N, Stanisavljevic D, Kostic V. Long-term prognosis of vascular hemiballismus. Stroke. 2002. 33: 2109-11
13. Siniscalchi A, Gallelli L, Labate A, Malferrari G, Palleria C, Sarro GD. Post-stroke movement disorders: Clinical manifestations and pharmacological management. Curr Neuropharmacol. 2012. 10: 254-62
14. Sugita Y, Funaki T, Takahashi JC, Takagi Y, Fushimi Y, Kikuchi T. Reversible striatal hypermetabolism in chorea associated with moyamoya disease: A report of two cases. Childs Nerv Syst. 2016. 32: 2243-7
15. Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969. 20: 288-99