- Department of Neurosurgery, LTMMC and GH, Sion, Mumbai, Maharashtra, India.
- Department of Surgery, Zen Hospital and Research Centre, Chembur, Mumbai, Maharashtra, India.
Correspondence Address:
Batuk Diyora, Department of Neurosurgery, 904, Krishna Co Operative Society, CD Burfiwala Lane, Andheri (West), Mumbai, Maharashtra, India.
DOI:10.25259/SNI_96_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Batuk Diyora1, Mehool Patel1, Gagan Dhall1, Pramod Kale2, Vishakha Kalikar2, Tanveer Majeed2, Kavin Devani1, Anup Purandare1, Roy Patankar2. Life-threatening perforating brain injury by a rusty iron rod – A case report. 20-May-2022;13:207
How to cite this URL: Batuk Diyora1, Mehool Patel1, Gagan Dhall1, Pramod Kale2, Vishakha Kalikar2, Tanveer Majeed2, Kavin Devani1, Anup Purandare1, Roy Patankar2. Life-threatening perforating brain injury by a rusty iron rod – A case report. 20-May-2022;13:207. Available from: https://surgicalneurologyint.com/surgicalint-articles/11609/
Abstract
Background: When an object traverses through the cranium leaving behind both an entry and exit wound, it is called perforating brain injury. Perforating open brain injury is rare. A paucity of published literature on such cases and a lack of a standard management protocol pose significant challenges in managing such cases.
Case Description: We present a case of a 24-year-old man who worked as a carpenter at the construction site. He slipped while working and fell from a height of 13 feet onto a rusty, vertically placed 3 feet iron rod located on the ground. Iron rod entered his body from the right upper chest, came out from the neck, and again re-entered through the right upper neck medial to the angle of the mandible and finally came out from the posterosuperior surface of the right side of the head. He presented to the emergency department in a conscious state, but his voice was heavy and slow-paced, and he showed signs of lower cranial nerve palsy on the right side. He underwent numerous radiological investigations. The iron rod was removed in the operation theater under strict aseptic precautions. On day 7 after surgery, he developed right lobar pneumonia, and on day 21, he developed an altered sensorium, followed by a loss of consciousness. He did not regain consciousness and, unfortunately, succumbed after 30 days of sustaining the injuries.
Conclusion: Perforating open brain injuries are rare, especially in civilian society, and are usually associated with significant morbidity and mortality. Due to a lack of standard guidelines for managing such severe injuries and limited knowledge, many patients with these injuries do not survive. Although each case presents differently, certain management principles must be followed.
Keywords: CT angiography, CT venogram, Iron rod, Perforating brain injury, Traumatic brain injury
INTRODUCTION
Penetrating brain injury is a wound through which an object breaks into the skull but does not exit it. Perforating brain injury occurs when an object traverses through the skull, leaving behind an entry and exit wound. Such open brain injuries have further classified as a missile or no missile (velocity <100 m/s) based on their impact velocity.[
CASE REPORT
A 24-year-old carpenter working at the construction site slipped and fell from a height of 13 feet onto a rusty vertical 3 feet iron rod, which perforated his body twice, first entering and exiting from the chest, and then from the head. Iron rod cuts with a hacksaw by his coworker at the site. He was brought to the hospital emergency department with an iron rod in situ. He was conscious, exhibited a Glasgow Coma Scale score of 15 (E4V5M6), and was well oriented to time, place, and person. His voice was heavy and slow-paced. His vital signs at the time of presentation were normal. On closer inspection, the right eye showed corneal opacity (due to an old injury), while his left pupil was normal in size and reacting well to the light. His extraocular movements were bilaterally normal. He showed signs of the lower cranial nerve palsy on the right side. His power in all four limbs was near normal.
Local examination
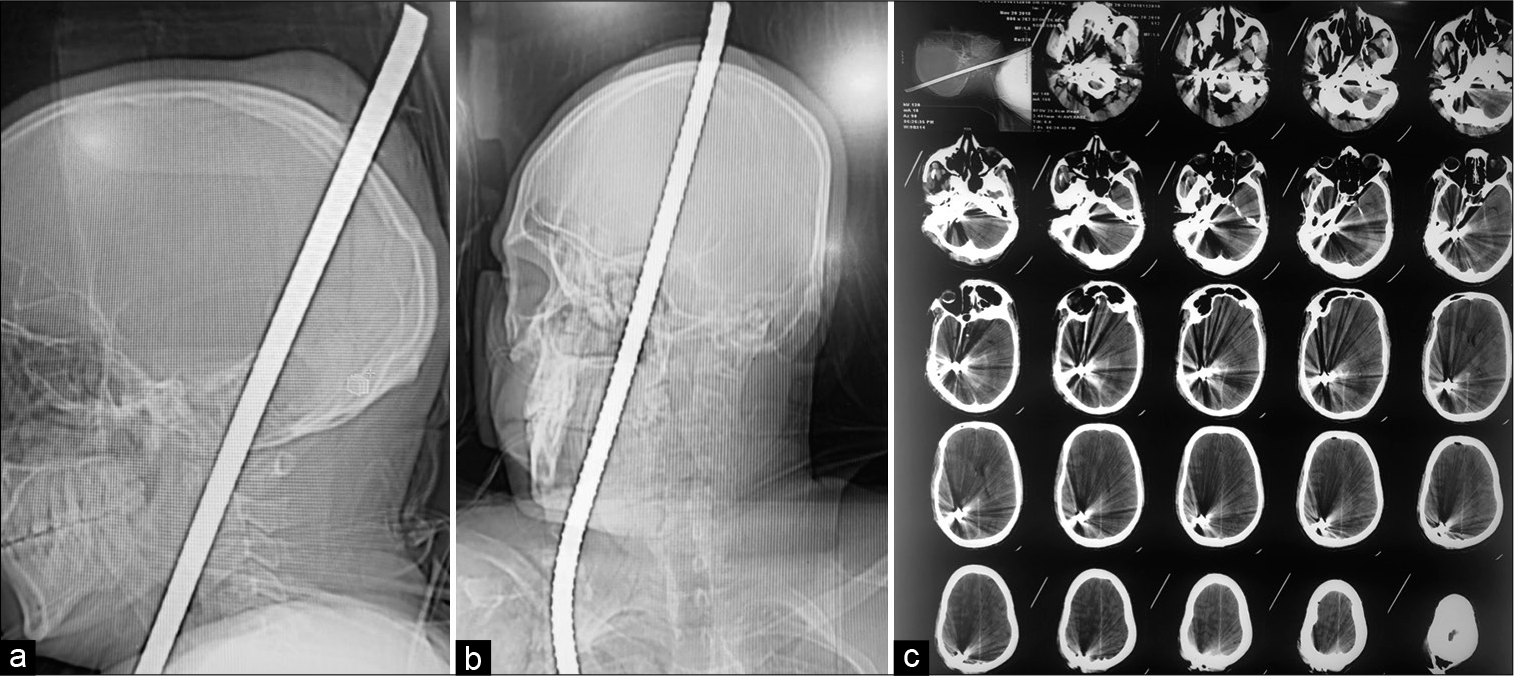
On local examination, a 3 feet iron rod with a thin coating of rust, approximately 1 cm in diameter, had entered the patient’s body by piercing through the skin and subcutaneous tissue of the right upper lateral chest wall just below the right clavicle and came out from the inferior half of the right side of the neck [
Emergency treatment
Following his presentation to the emergency department, he was started on oxygen therapy at a flow rate of 8 L/min through a face mask. He received a prophylactic tetanus toxoid injection. He was also administered intravenous phenytoin sodium, diclofenac sodium, and broad-spectrum antibiotics, including vancomycin and ceftriaxone, and mannitol. His wounds were cleaned with antiseptic solutions. He underwent an X-ray skull that revealed a metal rod in the skull [
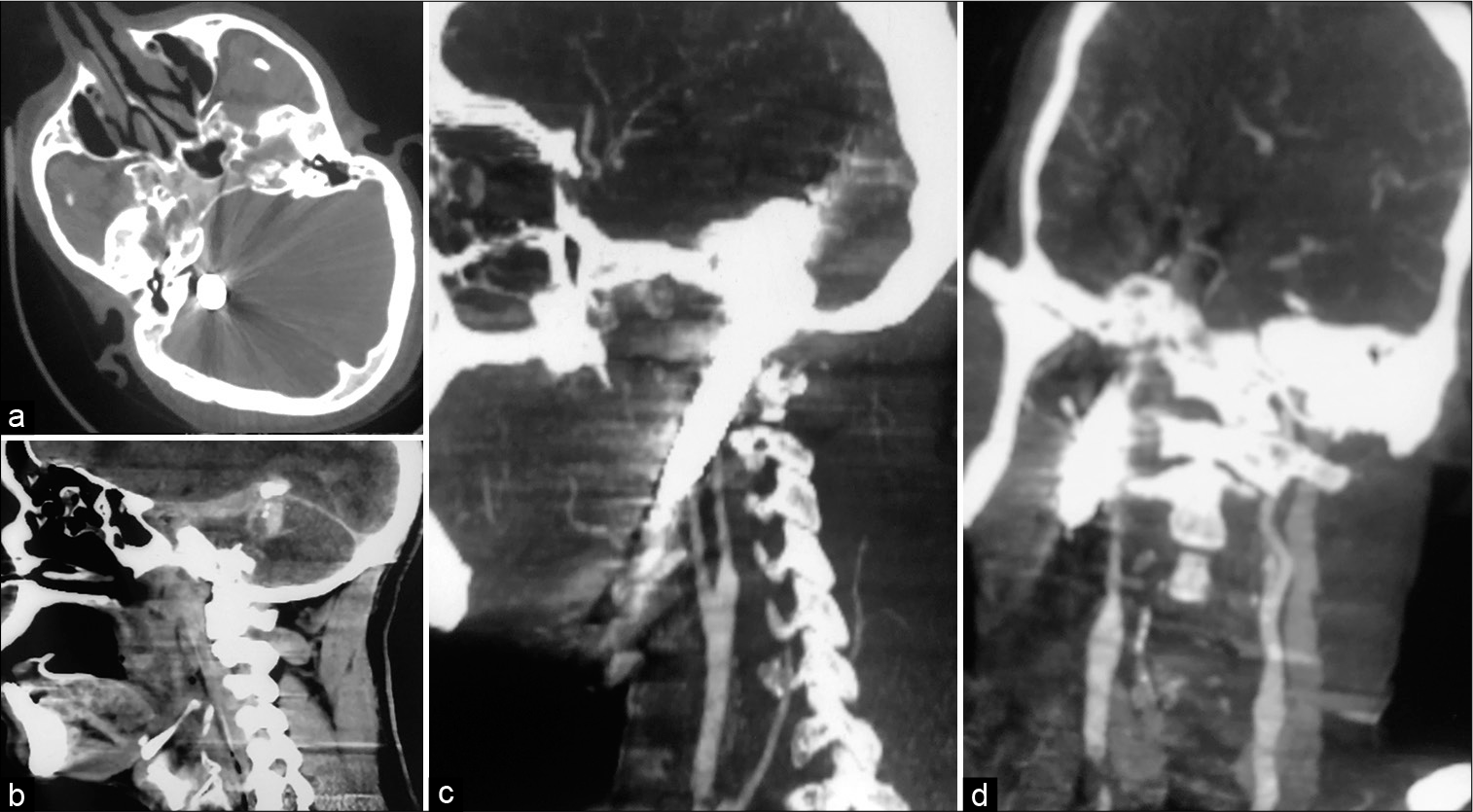
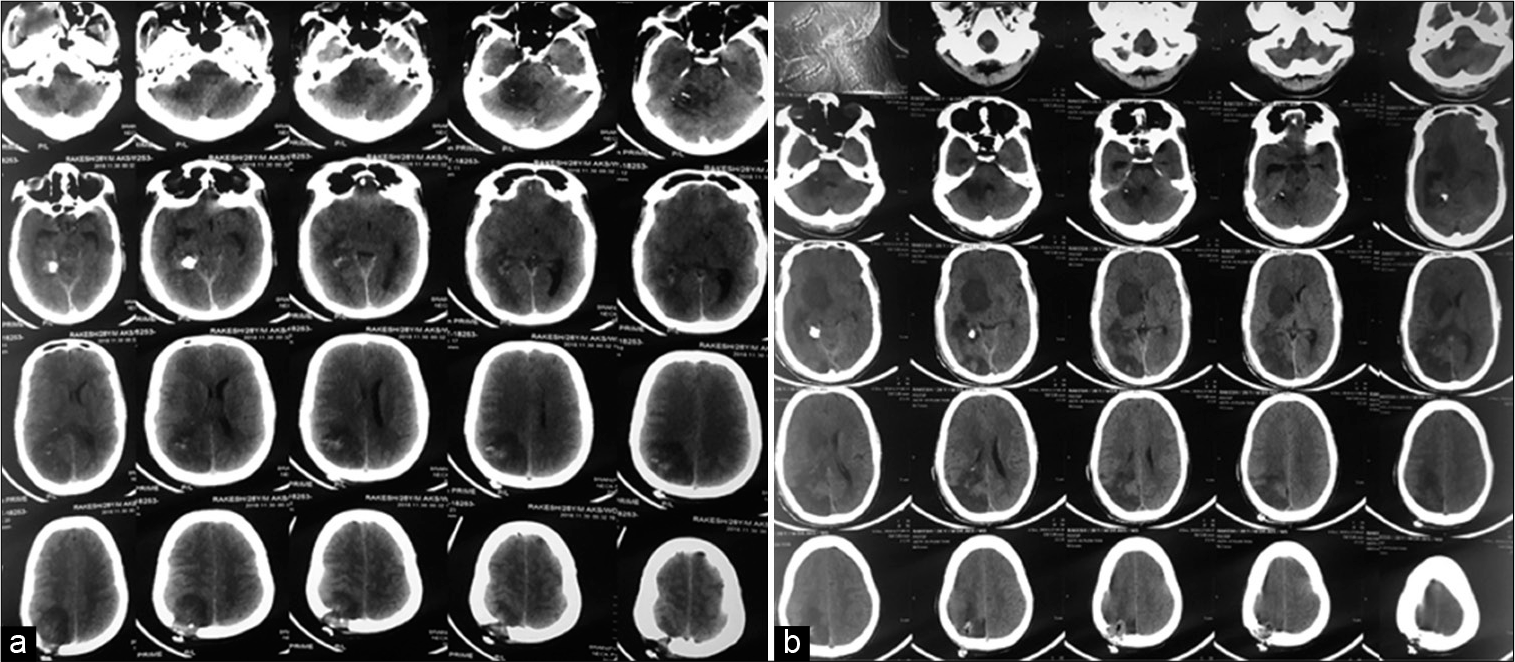
The thoracic and brain CT scan revealed the impaled metallic rod in the right upper chest, neck, and head region, along with metal streak artifacts. The rod has seen piercing through the right superolateral portion of the right pectoralis major muscle. It then passed briefly through the said muscle and exited it from its superomedial border just anterior to the right clavicle. Iron rod again pierced through the superior half of the neck on the right side in the right submandibular region lateral to the right submandibular gland and entered the skull base in the area of the right jugular foramen. The right internal carotid artery was seen below the skull base, crossing from the posteromedial aspect to the rod’s anterolateral part and appeared to have been partially indented by the rod. The rod, then, on its way up, was seen passing through the posterolateral portion of the right cerebellar hemisphere and, finally, exiting the skull through the posterior segment of the right parietal bone. A few hemorrhagic spots were noticed along the tract created by the rod [
Figure 3:
CT scan head (bone window) showing metallic iron rod in behind right petrous bone (a) and a sagittal view showing its passage through tentorium (b). CT angiography of the neck showing intact left and right carotid artery and left internal jugular vein with the absence of the right jugular vein (c and d).
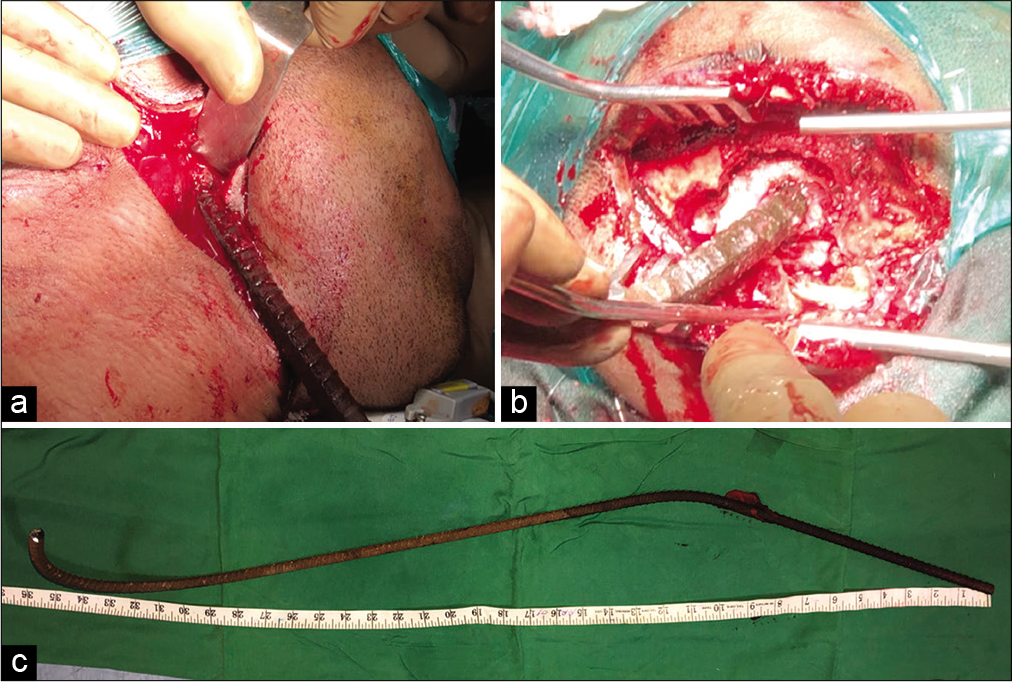
The patient was shifted to the operating room and the wound was explored. Securing his airway was a challenge as his neck was fixed in flexion and laterally tilted to the right side. Although mouth opening was good, negotiating laryngoscope in the mouth was not possible as the handle was getting obstructed due rod protruding out on the right side of the chest. There was absolutely no movement of the neck. There was a thick bridge of the skin and subcutaneous tissue on the rod at the neck, restricting lateral movement of the neck. With mild sedation and local anesthesia, part of the skin, subcutaneous tissue, and part of the right pectoralis major muscle cut to release the rod so that head can be manipulated. After doing so, we got the little lateral movement of the neck and we could negotiate laryngoscope and could intubate over the boogie [
The patient was turned to the left lateral position to reach the entry and exit wounds. The rusty iron rod (at the right parietal area) was carefully cleaned with saline, hydrogen peroxide, and betadine solution at the exit wound for 15 min. Two separate teams of surgeons performed the surgery. The neurosurgical team made an incision around the exit wound, explored the iron rod coming out of the parietal area, and completed a small craniectomy around the rod. The dura mater opened around the rod [
Postoperative CT scan
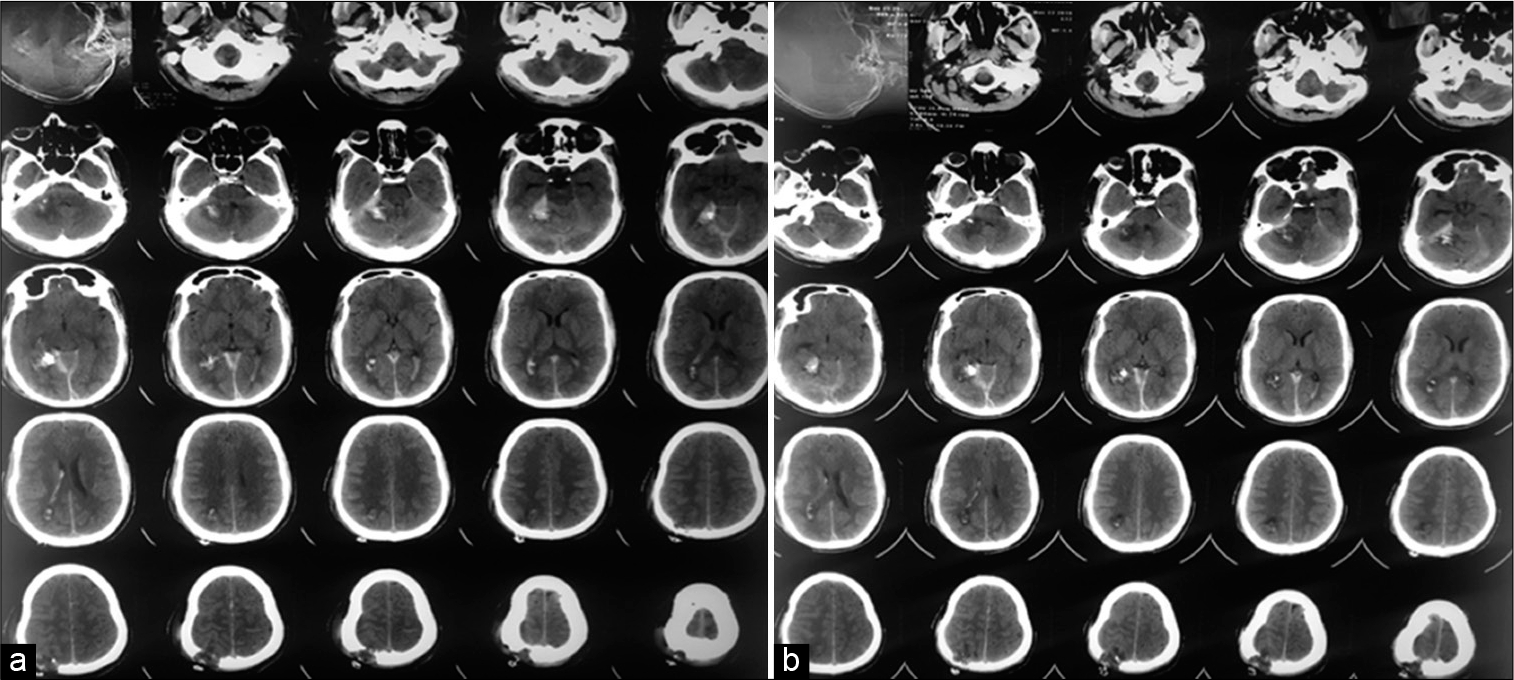
The patient’s postoperative CT scan brain revealed a linear tract of bleeding along the course of the impacted rod, which was seen extending from the right skull base, right lateral hemi-cerebellum, right tentorium cerebelli, and right parietal region. Additional findings were observed, including calvarial defects, minor right intraventricular bleed, and little right frontal extra-axial pneumocephalus. A small right subdural hematoma along the tentorial leaflet was noted. A few osseous hyperdensities were seen adjacent to the right tentorial leaflet, suggesting displaced bone fragments. The bone window revealed a minimally displaced fracture of the right occipital bone, superior to the right occipital condyle. Bone fragments were also seen in the right jugular foramen [
Postoperative sequelae
Postoperatively, the patient was ventilated and extubated after 48 h. On the 4th postoperative day, he underwent a CT scan brain plain study [
Figure 7:
Furthermore, a small fragment of bone was noticed traversed along with the iron rod just below the tent and the right parietal craniectomy defect. CT scan brain on the 10th postoperative day showing temporal resolution of hematoma along the course of an iron rod (a) and on the 21st postoperative day showing new hypodensity in the region of the right ganglion capsular region and right parieto-occipital region suggestive of recent infarct in the right posterior cerebral artery territory (b).
DISCUSSION
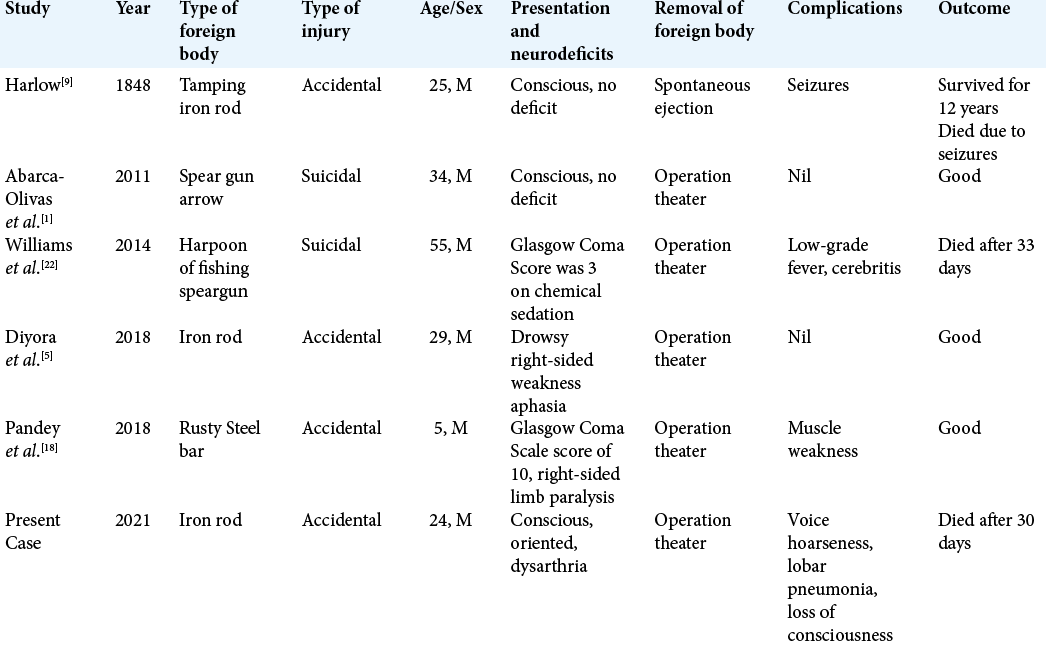
As described in our case report, the incidence of perforating open brain injuries is meager compared to penetrating brain injuries. Since the first-ever report of a perforating brain injury back in 1848 by Harlow,[
One should not attempt to remove the iron rod at the site (construction site in our case) where the patient suffered the injury. It is recommended to cut the perforating object (iron rod in our case) to such size that the patient can be transported easily to the hospital. Simultaneously, cutting the rod (iron rod in our case) should not create too much to and fro movements.[
Once the patient arrives at the emergency department, the patient must be received a prophylactic tetanus toxoid injection along with antibiotics, anti-edema therapy, and anti-convulsive medications by intravenous route. The wound’s primary dressing should be ensured, and again, no attempt should be made to pull out the rod in the emergency room without an attached operation theater.
A good understanding of the mechanism and mode of injury is necessary for optimum patient management with perforating brain injury. Depending on the perforating metallic object’s location, a routine CT scan of the brain parenchyma and bone window study is essential. It is also recommended to perform CT angiography and CT venography to rule out significant arterial or venous injury.[
The fundamental goals of surgery are removing the rod/ perforating body as soon as possible, preferably within 12 h,[
In cases of penetrating head injuries, the incidence of vascular complications, including actual and pseudoaneurysm, arteriovenous malformation, and subarachnoid hemorrhage, has been reported to be ranging from 5% to 40%. A preoperative digital subtraction angiography study has been recommended in managing such cases.[
CONCLUSION
Perforating open brain injuries are rare, especially in civilian society, and are usually associated with significant morbidity and mortality. Due to a lack of standard guidelines for managing such severe injuries and limited knowledge, many patients with these injuries do not survive. Although each case presents differently, certain management principles must be followed. Several factors, such as mechanism, site, size, and extent of the damage and time taken to transport the patient to the hospital, collectively determine this injury’s outcome.
Ethical approval
All procedures performed in this study were as per with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abarca-Olivas J, Concepcion-Aramendıa L, Bano-Ruiz E, Caminero-Canas MA, Navarro-Moncho JA, Botella-Asuncion C. Perforating brain injury from a speargun. A case report. Neurocirugia. 2011. 22: 271-510
2. Agilinko J, Gomati A, Keh SM, Brewis C, Shakeel M. Glass foreign body in the jugular foramen: Surgery versus conservative management. J Clin Case Rep. 2020. 3: 1027
3. Cemil B, Tun K, Yigenoglu O, Kaptanoglu E. Attempted suicide with screw penetration into the cranium. Ulus Travma Acil Cerrahi Derg. 2009. 15: 624-7
4. Chibbaro S, Tacconi L. Orbito-cranial injuries caused by penetrating nonmissile foreign bodies. Experience with eighteen patients. Acta Neurochir. 2006. 148: 937-41
5. Diyora B, Kotecha N, Mulla M, Dethe S, Bhende B, Patil S. Perforating head injury with an iron rod and its miraculous escape: Case report and review of the literature. Trauma Case Rep. 2018. 14: 11-9
6. Esposito DP, Walker JB. Contemporary management of penetrating brain injury. Neurosurg Q. 2009. 19: 249-54
7. Farhadi MR, Becker M, Stippich C, Unterberg AW, Kiening KL. Transorbital penetrating head injury by a toilet brush handle. Acta Neurochir. 2009. 151: 685-7
8. Fernández-Melo R, Morán AF, López-Flores G, BouzaMolina W, García-Maeso I, Benavides-Barbosas J. Penetrating head injury from harpoon. Case report. Neurocirugia (Astur). 2002. 13: 397-400
9. Harlow JM. Passage of an iron rod through the head. Boston Med Surg J. 1848. 39: 389-93
10. Helling TS, McNabney WK, Whittaker CK, Shultz CC, Watkins M. The role of early surgical intervention in civilian gunshot wounds to head. J Trauma. 1992. 32: 398-400
11. Hoeffner EG, Case I, Jain R, Guiar SK, Shah GV, Deveikis JP. Cerebral perfusion CT: Technique and clinical applications. Radiology. 2004. 231: 632-44
12. Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011. 4: 395-402
13. Levy ML, Rezai A, Masri LS, Litofsky SN, Giannotta SL, Apuzzo ML. The significance of subarachnoid hemorrhage after penetrating craniocerebral injury: Correlation with angiography and outcome in a civilian population. Neurosurgery. 1993. 32: 532-40
14. Mitilian D, Charon B, Brunelle F, Di Rocco F. Removal of a chopstick out of the cavernous sinus, pons, and cerebellar vermis through the superior orbital fissure. Acta Neurochir. 2009. 151: 1295-7
15. Nathoo N, Boodhoo H, Naidoo SR, Gouws E. Transcranial brain-stem stab injuries: A retrospective analysis of 17 patients. Neurosurgery. 2000. 47: 1117-22
16. . Neuroimaging in the management of penetrating brain injury. J Trauma. 2001. 51: S7-11
17. Offiah C, Twigg S. Imaging assessment of penetrating craniocerebral and spinal trauma. Clin Radiol. 2009. 64: 1146-57
18. Pandey S, Li L, Cui DM, Wang K, Gao L. Perforating brain injury by a rusty steel bar. J Craniofac Surg. 2018. 29: e372-5
19. Pascual JM, Navas M, Carrasco R. Penetrating ballistic-like frontal brain injury caused by a metallic rod. Acta Neurochir. 2009. 151: 689-691
20. Schreckinger M, Orringer D, Thompson BG, Marca FL, Sagher O. Transorbital penetrating injury: Case series, review of the literature, and proposed management algorithm. J Neurosurg. 2011. 114: 53-61
21. Sweeney JM, Lebovitz JJ, Eller JL, Coppens JR, Bucholz RD, Abdulrauf SI. Management of nonmissile penetrating brain injuries: A description of three cases and review of the literature. Skull Base Rep. 2011. 1: 39-46
22. Williams JR, Aghion DM, Doberstein CE, Cosgrove GR, Asaad WF. Penetrating brain injury after a suicide attempt with spear gun: Case study and review of the literature. Front Neurol. 2014. 5: 113
23. Yu L, Primak AN, Liu X, McCollough CH. Image quality optimization and evaluation of linearly mixed images in dual-source, dual-energy CT. Med Phys. 2009. 36: 1019-24