- Department of Neurosurgery, Kasr Alainy Faculty of Medicine, Cairo University, Egypt.
- Department of Neurosurgery, Al-Azhar University, Cairo, Egypt.
- Department of Anesthesia and Critical Care, Cairo University, Giza, Egypt.
Correspondence Address:
Hieder Al-Shami, Department of Neurosurgery, Al-Azhar University, Cairo, Egypt.
DOI:10.25259/SNI_425_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Ashry1, Hieder Al-Shami2, Medhat Gamal3, Ahmed M Salah1. Local anesthesia versus general anesthesia for evacuation of chronic subdural hematoma in elderly patients above 70 years old. 12-Jan-2022;13:13
How to cite this URL: Ahmed Ashry1, Hieder Al-Shami2, Medhat Gamal3, Ahmed M Salah1. Local anesthesia versus general anesthesia for evacuation of chronic subdural hematoma in elderly patients above 70 years old. 12-Jan-2022;13:13. Available from: https://surgicalneurologyint.com/surgicalint-articles/11339/
Abstract
Background: The aim of this study was to assess the safety and efficacy of chronic subdural hematoma (CSDH) evacuation by two burr-hole craniostomies under local versus general anesthesia (GA) in elderly patients over 70 years.
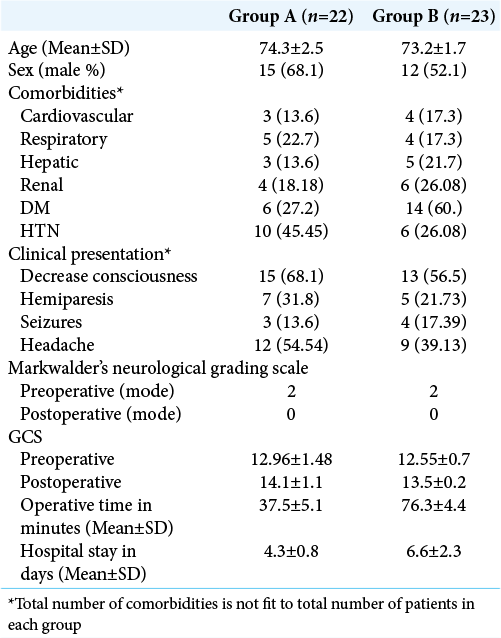
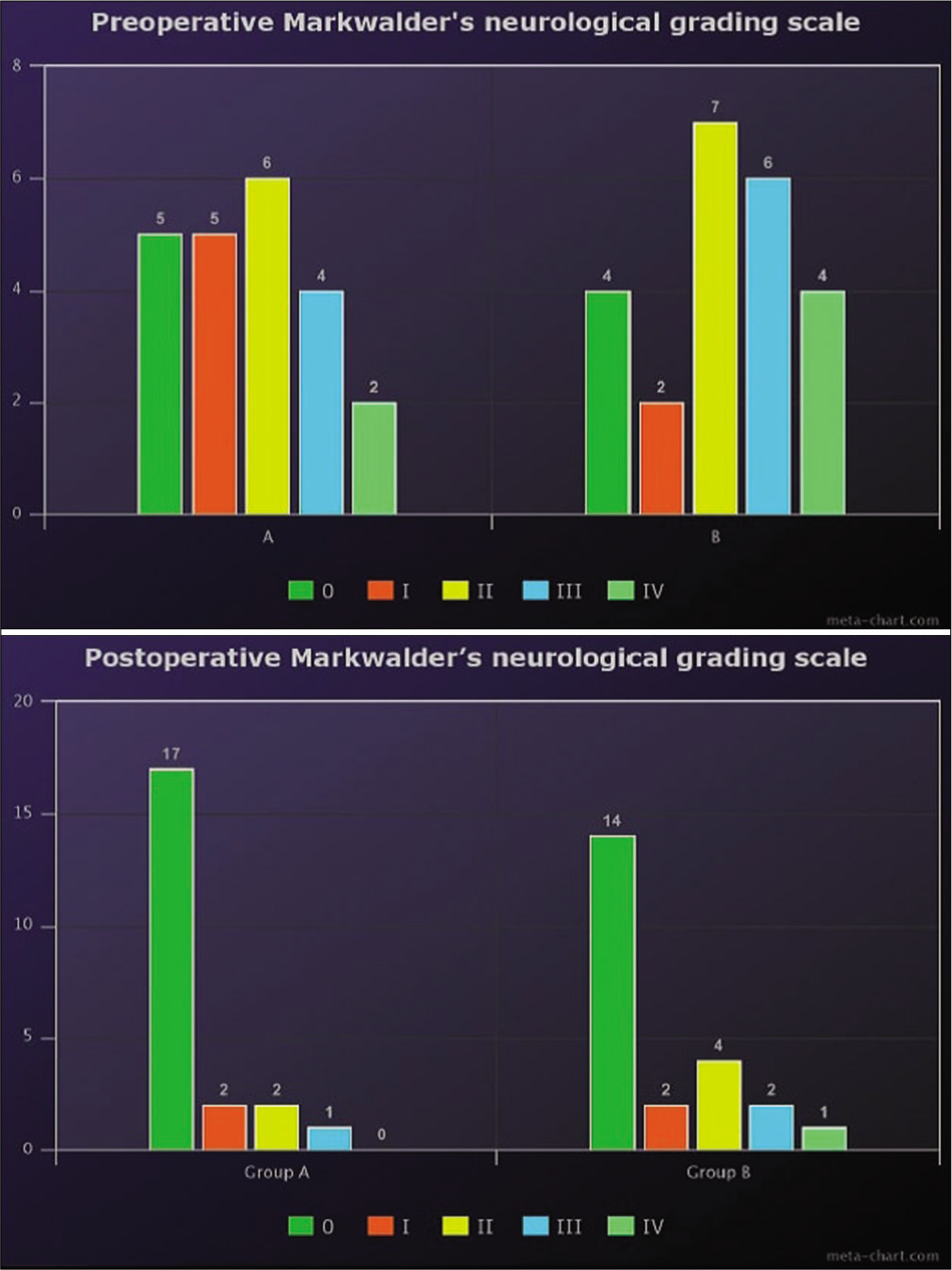
Methods: This retrospective study included 45 patients with CSDH aged over 70 years old treated from March 2018 to April 2020. The cases were subdivided into Group A (n = 22) that underwent evacuation under local anesthesia and Group B (n = 23) that was treated under GA. Patients’ demographics and history of comorbidities were recorded. Variables including pre- and post-operative neurological status and Markwalder’s score, complication rate, operative time, and length of hospital stay were evaluated.
Results: The mean and standard deviation of patients’ age of groups (A) and (B) were 74.3 ± 2.5 and 73.2 ± 1.7 years, respectively. Postoperative Glasgow Coma Scale of group (A) was statistically higher than Group B at postoperative day 1 (P = 0.01). Operative time was statistically shorter in Group A than B (P P = 0.0001). The complication rate was found to be higher in group (B) than (A) (P = 0.044).
Conclusion: Evacuation of CSDH under local anesthesia in elderly patients over 70 years is effective, safe, and economic with less complication rate than the traditional technique with GA.
Keywords: Chronic subdural hematoma, General anesthesia, Local anesthesia
INTRODUCTION
The management of chronic subdural hematoma (CSDH) is completely dependent on the amount of blood, midline shift, and symptomatology.[
MATERIALS AND METHODS
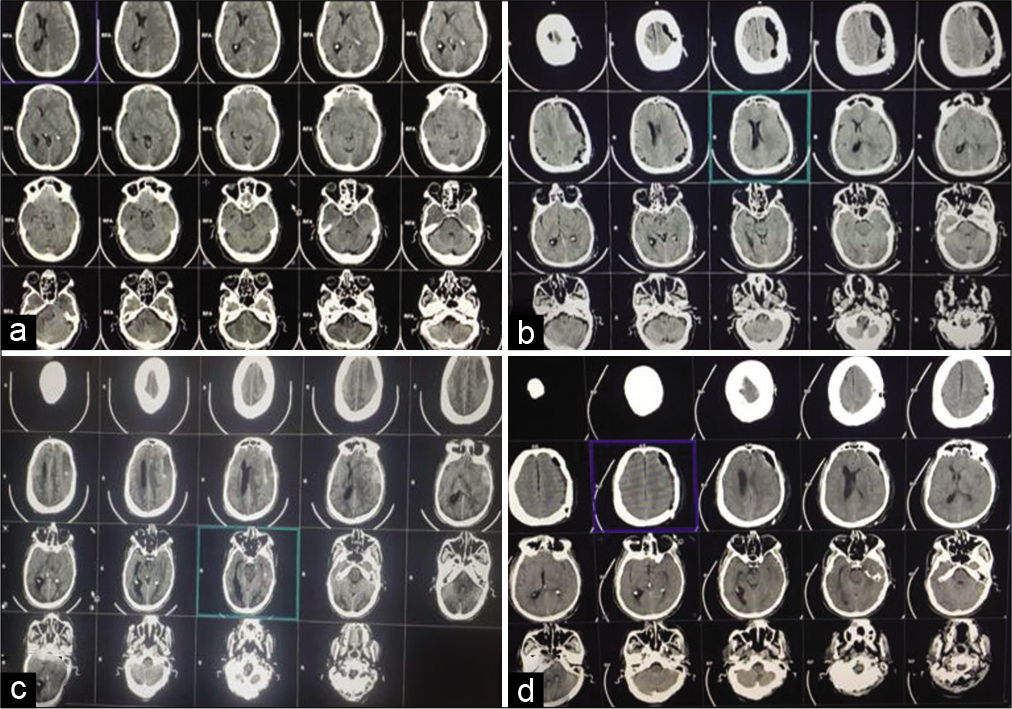
After approval from the Institutional Review Board of our institute, we retrospectively reviewed all patients with CSDH who were surgically treated from March 2018 to April 2020. Inclusion criteria involved patients aged over 70 years with comorbidities, unilateral or bilateral hematomas, and evacuation by two burr-hole craniostomies with opening of membranes. We excluded patients with acute on top of chronic hematomas, concomitant intracranial lesions, previous neurological disability, transition from local to GA, and those who were treated by craniotomy or single burr-hole craniostomy. The study included 45 patients who were divided into two groups. Group (A) included 22 patients treated under local anesthesia (LA). LA is applied by both – blocking corresponding scalp nerve supply (supraorbital, supratrochlear, zygomaticotemporal, auriculotemporal, great auricular, and lesser and greater occipital) using 0.5% bupivacaine added to 1:200,000 epinephrine with maximum dose of bupivacaine 2 mg/kg each nerve was blocked by 2–5 cc. Local infiltration by lidocaine 2% added to 1:100,000 intradermally max dose 5 mg/kg. After sterilizing skin, 2–5 ml of bupivacaine/epinephrine was located around nerve to be blocked additional 5–10 cc lidocaine 2% at burr-hole site. Sedatives (midazolam 2–4 mg/h or propofol 1–3 mg/kg/h) were given selectively for irritable patients. The other group (B) included 23 patients treated under GA by giving fentanyl 0.5 mg/kg IV bolus followed by a continuous infusion dose at a rate of 0.25 mg/kg/min. Pain during the procedure was treated by a supplemental injection of fentanyl. A local infiltration of scalp with adrenaline and lignocaine 2% after skin preparation was applied. For frontoparietal and frontotemporoparietal CSDH, a 2 cm scalp incision was put and twist drill trephination was performed using hand drill at a point 1 cm anterior or posterior to the coronal suture along the superior temporal line. Dura mater and outer membrane of CSDH were gently pierced. Note that, 10 FG infant feeding tube was inserted perpendicularly at a depth of 1–2 cm from the inner table and fixed to the scalp with suture. The distal end of the infant feeding tube was connected to urinary drainage bag. The patient was positioned supine in neutral position. Continuous gravity-dependent drainage was kept. The drain was removed after 24 h and scalp stapled. Computed tomography scan was taken in the postoperative period [
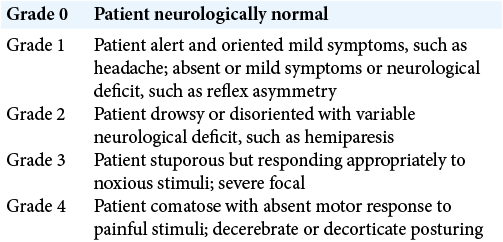
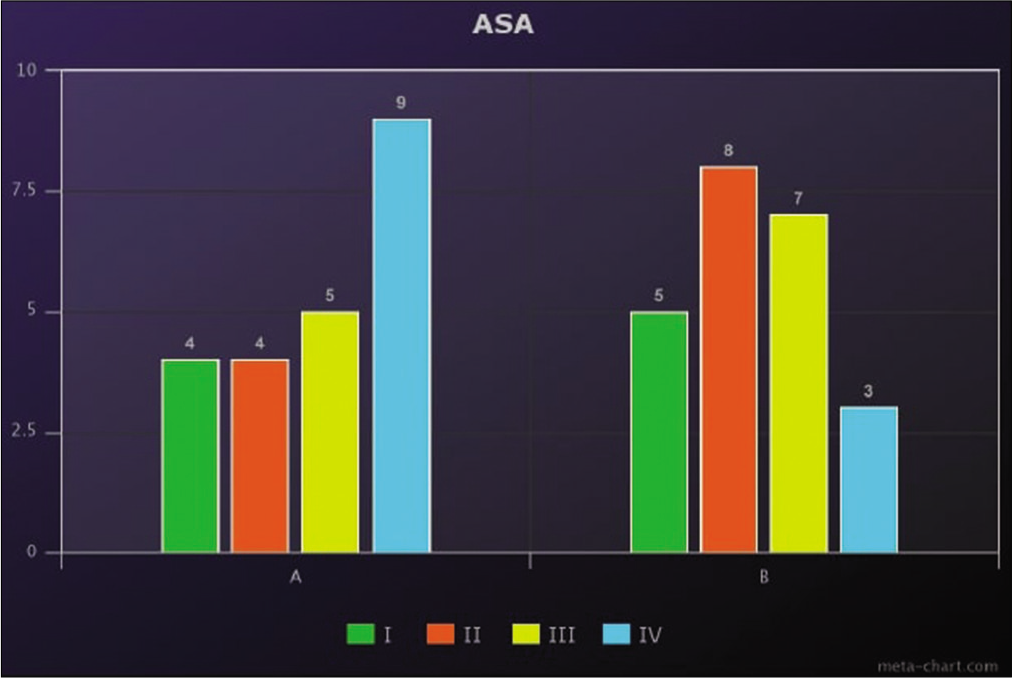
Patients’ demographics and associated comorbidities were recorded. General health conditions were classified according to the American Society of Anesthesiology (ASA) grades. Complete neurological assessment including Glasgow Coma Score (GCS) and Markwalder grade [
RESULTS
Patients’ criteria are illustrated in [
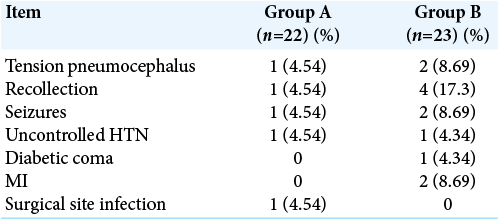
Postoperative complications are illustrated in [
DISCUSSION
CSDH is a common neurosurgical disorder that usually affects elderly patients after minor head trauma.[
Although local anesthesia was used during evacuations of CSDH by many authors, patients may become anxious and experience discomfort during the procedure.[
In our study, the most frequent presentation of patients was impairment of consciousness. The diagnosis of CSDH in elderly patients is usually delayed as neurological symptoms are usually related to vascular insufficiency or dementia. Conscious level improved more markedly in postoperative day 1 in the LA group. GA carries an additional risk of postoperative cognitive impairment and delirium hindering recovery in spite of the disappearance of the hematoma on serial postoperative images.[
We used to evacuate CSDH through two burr holes for better determination of hematoma boundary.[
The recurrence rate of hematomas was higher in the GA group. This can be explained by the occurrence of rebound hypertension during the awakening process.[
In the LA group, early mobilization of patients could be achieved. This decreased the incidence of postoperative deep venous thrombosis and lung atelectasis, abandoning the need for intensive care unit admission.[
Postoperative complications were found to be significantly more in the GA group. The majority of patients necessitated other departmental consultations which lengthened their hospital stays. The length of hospital stay was shorter in the LA group which proved to be economical and reduced hospital-acquired infections.[
This retrospective study has some limitations. The clinical and radiological data of the patients had to be obtained from the medical records. However, the results of our study suggested that surgical evacuation using local anesthesia should be the default treatment for CSDH, especially in high-risk elderly patients.
CONCLUSION
Evacuation of CSDH under local anesthesia in elderly patients above 70 years of age is effective and economical with fewer complications than the traditional technique with GA.
Ethics approval and consent to participate
An ethical approval from our institutional board was obtained before recruitment of the study.
Availability of data and materials
All the data retrieved in this article are already published previously and available at ease.
Authors’ contributions
Conceptualization: AHA. Data curation: AHA and AMS. Formal analysis: AHA and MG. Methodology: AHA, HA, and MG. Project administration: AHA and HA. Visualization: AHA, HA, and AMS. Writing – original draft: AHA, HA, and AMS. Writing – review and editing: HA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Many thanks to our neurosurgery team for their support, knowledge, and empowering our skills at Kasr Al-Ainy University Hospital.
References
1. Abe Y, Maruyama K, Yokoya S, Noguchi A, Sato E, Nagane M. Outcomes of chronic subdural hematoma with preexisting comorbidities causing disturbed consciousness. J Neurosurg. 2017. 126: 1042-6
2. Atsumi H, Sorimachi T, Honda Y, Sunaga A, Matsumae M. Effects of pre-existing comorbidities on outcomes in patients with chronic subdural hematoma. World Neurosurg. 2019. 122: e924-32
3. Farid A, Shakal AA, El Gamal E. Chronic subdural hematoma: Complication avoidance. Tanta Med J. 2014. 42: 6-13
4. Guzel A, Kaya S, Ozkan U, Aluclu MU, Ceviz A, Belen D. Surgical treatment of chronic subdural haematoma under monitored anaesthesia care. Swiss Med Wkly. 2008. 138: 398-403
5. Kidangan GS, Thavara BD, Rajagopalawarrier B. Bedside percutaneous twist drill craniostomy of chronic subdural hematoma-a single-center study. J Neurosci Rural Pract. 2020. 11: 84-8
6. Lee KS. How to treat chronic subdural hematoma? Past and now. J Korean Neurosurg Soc. 2019. 62: 144-52
7. Mahmood SD, Waqas M, Baig MZ, Darbar A. Mini-craniotomy under local anesthesia for chronic subdural hematoma: An effective Choice for elderly patients and for patients in a resource-strained environment. World Neurosurg. 2017. 106: 676-9
8. Mehta V, Harward SC, Sankey EW, Nayar G, Codd PJ. Evidence based diagnosis and management of chronic subdural hematoma: A review of the literature. J Clin Neurosci. 2018. 50: 7-15
9. Mersha A, Abat S, Temesgen T, Nebyou A. Outcome of chronic subdural hematoma treated with single burr hole under local anesthesia. Ethiop J Health Sci. 2020. 30: 101-6
10. Rauhala M, Helén P, Huhtala H, Heikkilä P, Iverson GL, Niskakangas T. Chronic subdural hematoma-incidence, complications, and financial impact. Acta Neurochir (Wien). 2020. 162: 2033-43
11. Salama H. Outcome of single burr hole under local anesthesia in the management of chronic subdural hematoma. Egypt J Neurosurg. 2019. 34: 8
12. Savoia G, Loreto M, Gravino E, Canfora G, Frangiosa A, Cortesano P. Monitored anesthesia care and loco-regional anesthesia. Vascular surgery use. Minerva Anestesiol. 2005. 71: 539-42
13. Seizeur R, Abed-Rabbo F, Obaid S, Saliou P, Simon A, Hieu PD. Chronic subdural haematomas in elderly population. Neurosurgical aspects and focus on the single-burr hole technique performed under assisted local anaesthesia. Br J Neurosurg. 2017. 31: 258-61
14. Sinclair RCF, Faleiro RJ. Delayed recovery of consciousness after anaesthesia. Contin Educ Anaesth Crit Care Pain. 2006. 6: 114-8
15. Surve RM, Bansal S, Reddy M, Philip M. Use of dexmedetomidine along with local infiltration versus general anesthesia for burr hole and evacuation of chronic subdural hematoma (CSDH). J Neurosurg Anesthesiol. 2017. 29: 274-80