- Department of Neurosurgery, University of Medical Sciences, Rasool Akram Hospital, Tehran, Iran
Correspondence Address:
Morteza Taheri
Department of Neurosurgery, University of Medical Sciences, Rasool Akram Hospital, Tehran, Iran
DOI:10.4103/2152-7806.194516
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ali Babashahi, Morteza Taheri, Arash Fattahi. Long standing lumbosacral dermoid tumor and intracranial fat droplet dissemination: A case report. 21-Nov-2016;7:
How to cite this URL: Ali Babashahi, Morteza Taheri, Arash Fattahi. Long standing lumbosacral dermoid tumor and intracranial fat droplet dissemination: A case report. 21-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/long-standing-lumbosacral-dermoid-tumor-and-intracranial-fat-droplet-dissemination-a-case-report/
Abstract
Background:Dermoid tumors are slow growing, benign CNS lesions.
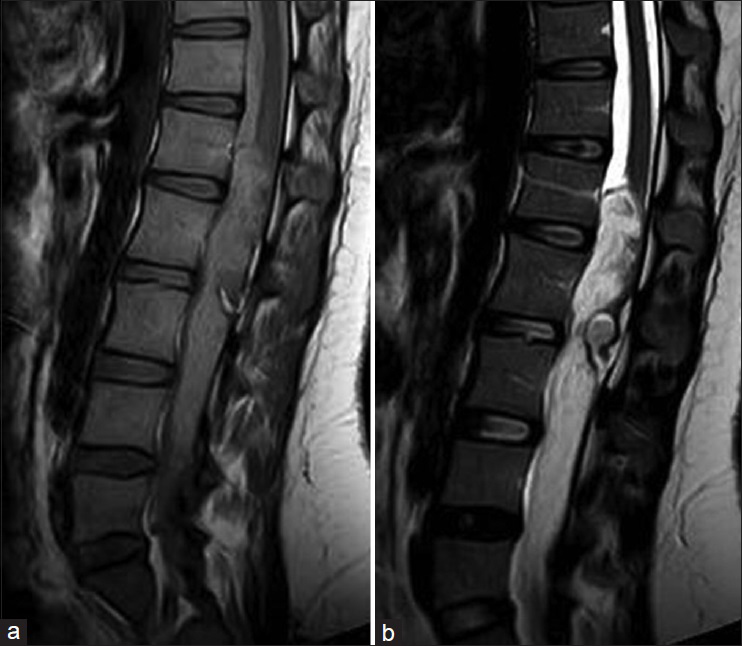
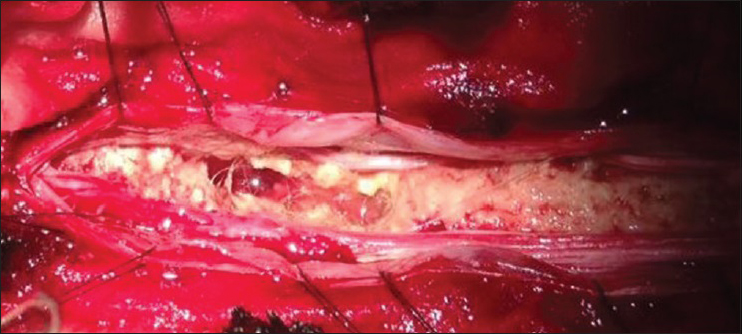
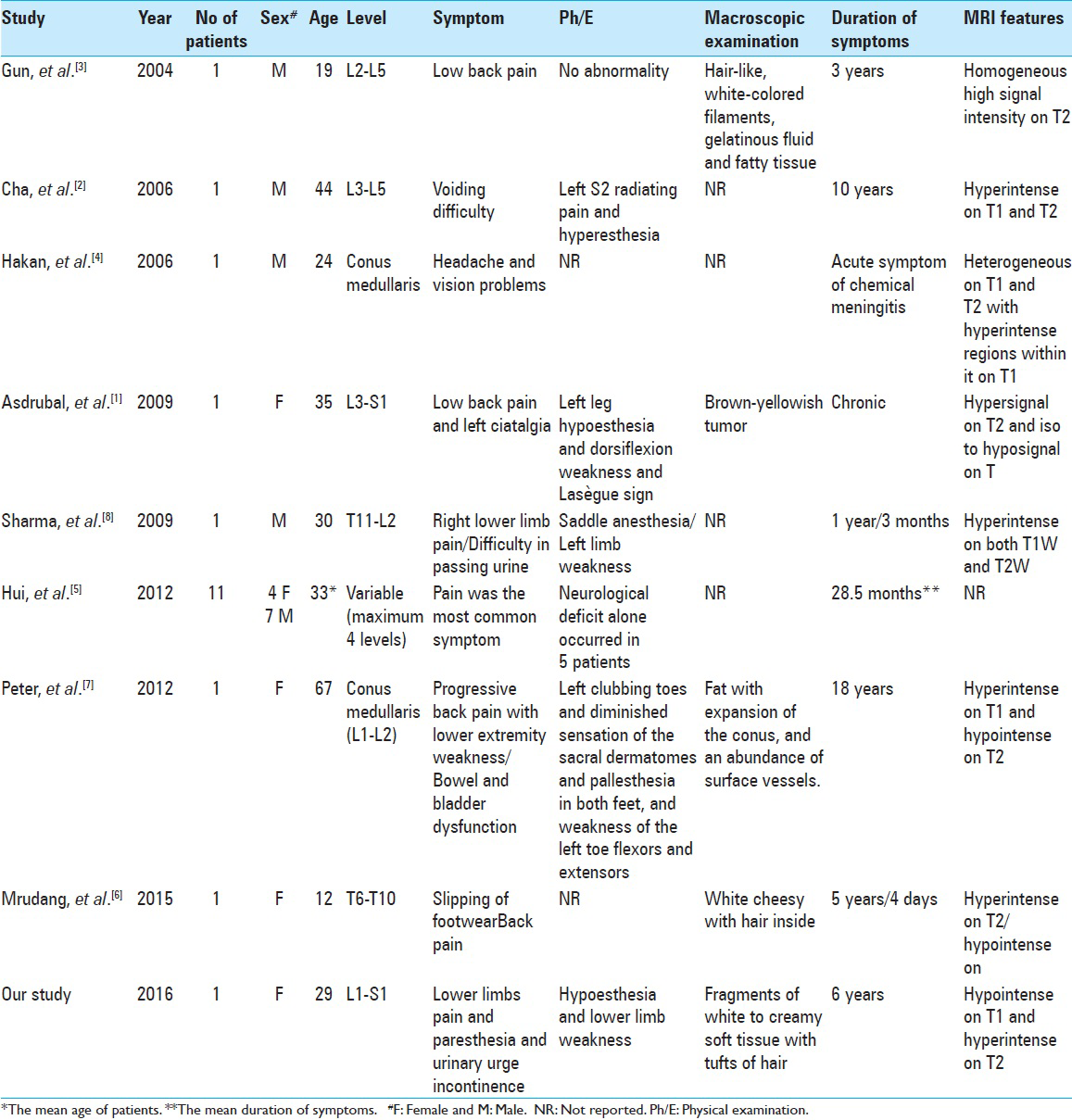
Case Description:This case study concerns a 29-year-old female with a 6-year history of lower extremity paresthesias attributed to magnetic resonance (MR)/computed tomography (CT) documented intradural dermoid tumor that extended from L1 to S1. On MR, it was hypointense on T1, hyperintense on T2, and did not enhance with gadolinium. CT showed hyperdensity at the L1-L2 levels. The craniocervical MR imaging showed small hyperintense foci in the cisternal space favoring “fat dissemination.” L1-S2 laminectomy revealed an intradural lesion characterized by “a solid and firm component compatible with fat tissue adherent to the conus medullaris and a solid-soft component within the cauda equina;” there were also “multiple fragments of white-creamy soft tissue with hair.” Following tumor resection, the brain CT scan demonstrated fat dissemination within the intraventricular and cisternal space. Histopathologic examination confirmed the diagnosis of a dermoid tumor.
Conclusion:Dermoid tumors should be considered among the differential diagnosis of intradural lesions in young patients even without any other congenital abnormality.
Keywords: Dermoid tumor, fat droplet dissemination, intraspinal tumor
INTRODUCTION
Dermoid tumors, attributed to superficial ectoderm dysembriogenesis occurring during the gastrulation phase of fetal development, are slow growing, benign tumors occasionally found within the nervous system.[
CASE DESCRIPTION
A 29-year-old female complained of low back pain and lower limbs paresthesias for 6 years; symptoms had exacerbated for the last 1.5 years. She also had urinary urge incontinence, sacral hypoesthesia, and 4/5 lower extremity weakness. The lumbosacral magnetic resonance (MR) imaging showed an intradural lesion filling the canal from L1 to S1; it was hypointense on T1, hyperintense on T1, and showed no enhancement with gadolinium injection [
Surgery
The L1-S2 laminectomy revealed an intradural lesion that filled the spinal canal. There were fragments of white-to-creamy soft tissue with tufts of hair [
DISCUSSION
Dermoid tumors are rare benign tumors that are more common in the brain than the spine.[
CONCLUSION
Dermoid tumors should be considered amongst the differential diagnoses of intradural spinal lesions in younger patients even without accompanying congenital abnormalities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asdrubal F, Orlando R, Alisson R. Concomitant dermoid cysts of conus medullaris and cauda equine. Arq Neuropsiquiatr. 2009. 67: 293-6
2. Cha JG, Paik SH, Park JS, Park SJ, Kim DH, Lee HK. Ruptured spinal dermoid cyst with disseminated intracranial fat droplets. Br J Radiol. 2006. 79: 167-9
3. Gun WW, Kim SJ, Cho DS, Seo EK. Multiple Lumbar Intradural Dermoid Cysts without Spinal Dysraphism. J Korean Neurosurg Soc. 2004. 36: 505-7
4. Hakan A, Ömer K, Cem Ç, Nilgün Y. A spinal dermoid tumor that ruptured into the subarachnoidal space and syrinx cavity. Diagn Interv Radiol. 2006. 12: 171-3
5. Hui L, Jian-Ning Z, Tao Z. Microsurgical treatment of spinal epidermoid and dermoid cysts in the lumbosacral region. J Clin Neurosci. 2012. 19: 712-7
6. Mrudang R, Sunita P, Vineet M, Tanay S. Ruptured thoracic intraspinal dermoid cyst in a patient with skeletal abnormalities of thoracic spine- A case report. Egyptian J Radiol Nuclear Med. 2015. 46: 435-9
7. Peter ND, David JM, Tim RK, Abhijit G. Spinal Conus Dermoid Cyst with Lipid Dissemination. Radiographics. 2012. 32: 1215-21
8. Sharma NC, Tushar C, Anshu S, Manish B, Ravinder K. Long-segment intramedullary spinal dermoid. Indian J Radiol Imaging. 2009. 19: 148-50