- Department of Neurosurgery, Graduate School of Medicine and Pharmacological Science, University of Toyama, Toyama, Japan
Correspondence Address:
Shusuke Yamamoto
Department of Neurosurgery, Graduate School of Medicine and Pharmacological Science, University of Toyama, Toyama, Japan
DOI:10.4103/sni.sni_472_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shusuke Yamamoto, Satoshi Kuroda. Long-term effect of surgical revascularization on silent microbleeds in adult moyamoya disease: A case report. 05-Jun-2017;8:99
How to cite this URL: Shusuke Yamamoto, Satoshi Kuroda. Long-term effect of surgical revascularization on silent microbleeds in adult moyamoya disease: A case report. 05-Jun-2017;8:99. Available from: http://surgicalneurologyint.com/surgicalint-articles/long%e2%80%91term-effect-of-surgical-revascularization-on-silent-microbleeds-in-adult-moyamoya-disease-a-case-report/
Abstract
Background:Recent development of magnetic resonance (MR) imaging has shown that silent microbleeds can be observed in a certain subgroup of adult patients with moyamoya disease. The patients with microbleeds are at higher risk for hemorrhagic stroke. However, the beneficial effects of surgical revascularization have not been established in asymptomatic patients with moyamoya disease. The authors present a case that underwent surgical revascularization for asymptomatic moyamoya disease because the number of silent microbleeds increases on serial MR examinations.
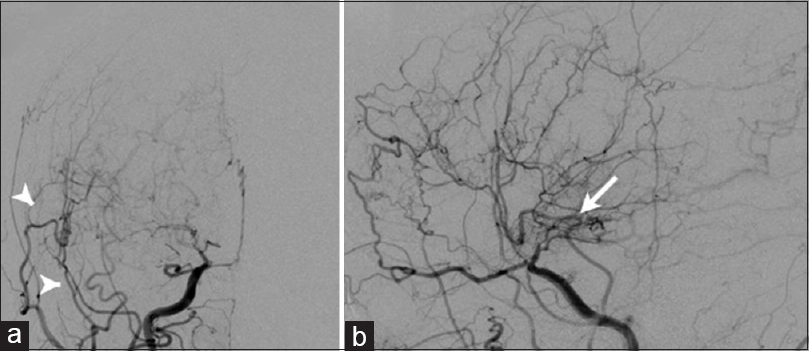
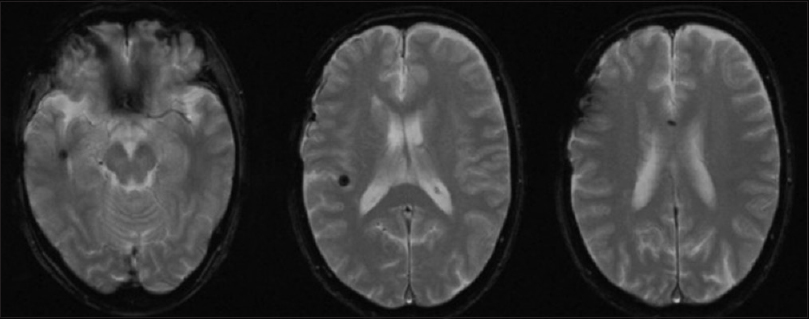
Case Description:A 61-year-old female was referred to our hospital because of nonspecific headache. T2-weighted MR imaging revealed silent microbleeds in the corpus callosum. She was diagnosed as moyamoya disease on cerebral angiography. She was conservatively followed up, however, de novo microbleeds developed in the right temporal and frontal lobes on follow-up MR imaging 6 months later. Superficial temporal artery to middle cerebral artery (STA-MCA) anastomosis and indirect bypass were performed on the right side to prevent hemorrhagic stroke. Postoperative course was uneventful. Follow-up cerebral angiography performed 10 months after surgery showed a marked development of surgical collateral through both direct and indirect bypass and the diminishment of moyamoya vessels. For the last 7 years after surgery, she is free from any cerebrovascular events, and serial MR examinations revealed no further development of de novo microbleeds.
Conclusions:Surgical revascularization may be useful to reduce the moyamoya vessels and prevent cerebrovascular events in a certain subgroup of patients with asymptomatic moyamoya disease, although its universal benefits on asymptomatic moyamoya disease have not been established yet.
Keywords: Moyamoya disease, prognosis, silent microbleeds, surgical revascularization
BACKGROUND
Moyamoya disease is a unique cerebrovascular disorder characterized by progressive occlusion in the terminal portion of internal carotid artery (ICA) and its main branches, anterior and middle cerebral arteries (ACA and MCA, respectively). The perforating arteries are markedly dilated to supply collateral blood flow to the ischemic brain, called as moyamoya vessels. Pediatric patients usually develop transient ischemic attack (TIA) or ischemic stroke, whereas adult patients also develop hemorrhagic stroke.[
On the other hand, recent development of magnetic resonance imaging (MRI) has shown that silent microbleeds can be observed in a certain subgroup of adult patients with moyamoya disease. Silent microbleeds are identified more frequently in patients with moyamoya disease than in healthy individuals. They are found in the basal ganglia, thalamus, and periventricular region where intracranial bleeding often occurs in moyamoya disease.[
Here, the authors present a 61-year-old female who underwent surgical revascularization for asymptomatic moyamoya disease because serial MRI demonstrated an increase in the number of silent cerebral microbleeds. For the last 7 years, she has been free from both de novo microbleeds and any cerebrovascular events.
CASE DESCRIPTION
A 61-year-old female complained of chronic, nonspecific headache and was referred to our hospital. She had no past history and no family history of moyamoya disease. Neurological and laboratory examinations revealed no definite abnormalities. Although T1- and T2-weighted MRI demonstrated no lesion, T2-weighted MRI revealed a microbleed in the genu of corpus callosum [
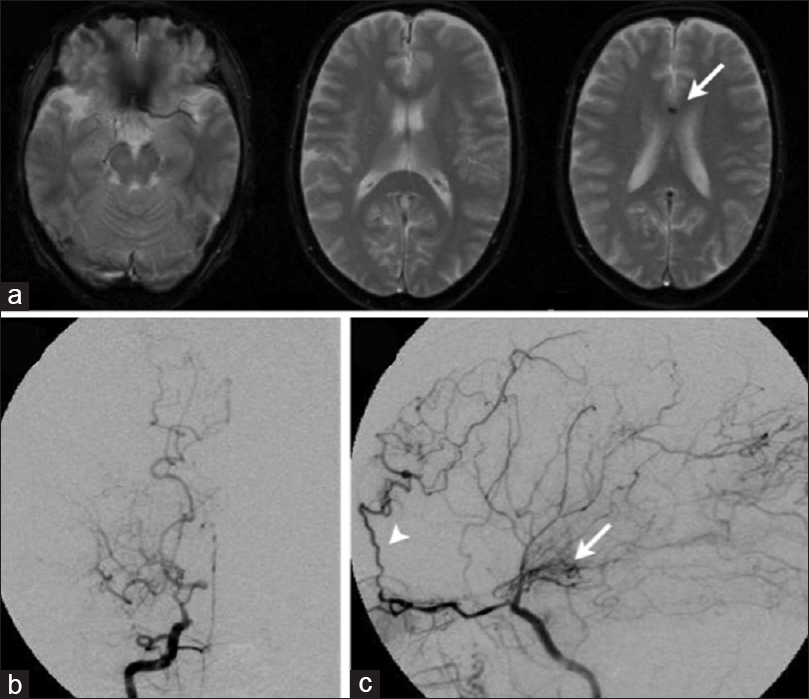
Figure 1
T2-weighted MRI at initial presentation (a) showed silent microbleed in the genu of corpus callosum (arrow). AP (b) and lateral views (c) of preoperative right internal carotid angiography showed severe stenosis in the terminal portion of the right internal carotid artery (ICA) associated with the development of basal moyamoya vessels (arrow). Note the development of collateral pathway to the anterior cerebral artery through the ophthalmic artery
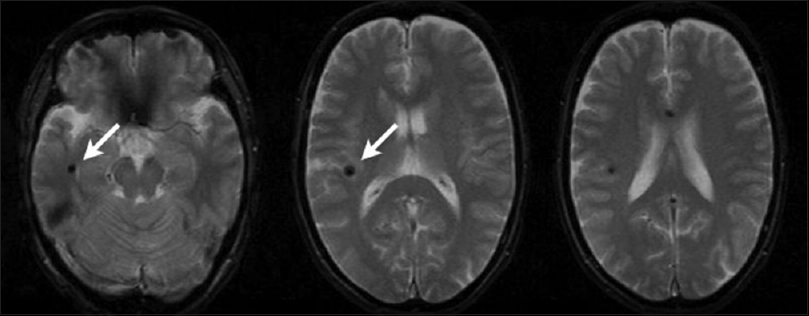
Follow-up MRI was obtained 6 months later. Although she developed no cerebrovascular episodes, T2-weighted MRI revealed two de novo microbleeds in the right deep temporal lobe adjacent to the temporal horn and the right frontal lobe [
DISCUSSION
The present case was considered at very high risk for hemorrhagic stroke in near future and underwent surgical revascularization without any cerebrovascular episodes. There are several reasons for this exceptional decision. First, initial T2-weighted MRI identified a silent microbleed in the corpus callosum. The annual risk of hemorrhagic stroke is significantly higher in adult patients with silent microbleeds at initial presentation than those without (6.6% and 0%, respectively).[
Surgical revascularization is widely known to be useful in reducing the risk of both ischemic and hemorrhagic stroke.[
CONCLUSION
The authors report an adult case with asymptomatic moyamoya disease that successfully underwent combined surgical revascularization because follow-up T2-weighted MRI identified de novo microbleeds. She has reported no cerebrovascular events in the last 7 years after surgery. The benefits of surgical revascularization on asymptomatic moyamoya disease should carefully be evaluated in the near future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ishikawa T, Kuroda S, Nakayama N, Terae S, Kudou K, Iwasaki Y. Prevalence of asymptomatic microbleeds in patients with moyamoya disease. Neurol Med Chir (Tokyo). 2005. 45: 495-500
2. Kawai K, Kuroda S, Kawabori M, Nakayama N, Terasaka S, Iwasaki Y. Revascularization surgery for asymptomatic adult moyamoya disease presenting silent disease progression: Report of two cases. No Shinkei Geka. 2010. 38: 825-30
3. Kazumata K, Shinbo D, Ito M, Shichinohe H, Kuroda S, Nakayama N. Spatial relationship between cerebral microbleeds, moyamoya vessels, and hematoma in moyamoya disease. J Stroke Cerebrovasc Dis. 2014. 23: 1421-8
4. Kikuta K, Takagi Y, Nozaki K, Hanakawa T, Okada T, Mikuni N. Asymptomatic microbleeds in moyamoya disease: T2*-weighted gradient-echo magnetic resonance imaging study. J Neurosurg. 2005. 102: 470-5
5. Kikuta K, Takagi Y, Nozaki K, Okada T, Hashimoto N. Histological analysis of microbleed after surgical resection in a patient with moyamoya disease. Neurol Med Chir (Tokyo). 2007. 47: 564-7
6. Kikuta K, Takagi Y, Nozaki K, Sawamoto N, Fukuyama H, Hashimoto N. The presence of multiple microbleeds as a predictor of subsequent cerebral hemorrhage in patients with moyamoya disease. Neurosurgery. 2008. 62: 104-11
7. Kuroda S, Group AS. Asymptomatic moyamoya disease: Literature review and ongoing AMORE study. Neurol Med Chir (Tokyo). 2015. 55: 194-8
8. Kuroda S, Hashimoto N, Yoshimoto T, Iwasaki Y. Radiological findings, clinical course, and outcome in asymptomatic moyamoya disease: Results of multicenter survey in Japan. Stroke. 2007. 38: 1430-5
9. Kuroda S, Houkin K. Moyamoya disease: Current concepts and future perspectives. Lancet Neurol. 2008. 7: 1056-66
10. Kuroda S, Houkin K, Ishikawa T, Nakayama N, Iwasaki Y. Novel bypass surgery for moyamoya disease using pericranial flap: Its impacts on cerebral hemodynamics and long-term outcome. Neurosurgery. 2010. 66: 1093-101
11. Kuroda S, Kashiwazaki D, Ishikawa T, Nakayama N, Houkin K. Incidence, locations, and longitudinal course of silent microbleeds in moyamoya disease: A prospective T2*-weighted MRI study. Stroke. 2013. 44: 516-8
12. Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T. Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: Results of the Japan adult moyamoya trial. Stroke. 2014. 45: 1415-21
13. Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969. 20: 288-99
14. Takahashi JC, Funaki T, Houkin K, Inoue T, Ogasawara K, Nakagawara J. Significance of the Hemorrhagic Site for Recurrent Bleeding: Prespecified Analysis in the Japan Adult Moyamoya Trial. Stroke. 2016. 47: 37-43