- Department of Neurosurgery, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
Correspondence Address:
Nancy Ellen Epstein
Department of Neurosurgery, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
DOI:10.4103/2152-7806.182545
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Epstein NE. Low reoperation rate following 336 multilevel lumbar laminectomies with noninstrumented fusions. Surg Neurol Int 17-May-2016;7:
How to cite this URL: Epstein NE. Low reoperation rate following 336 multilevel lumbar laminectomies with noninstrumented fusions. Surg Neurol Int 17-May-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/low-reoperation-rate-following-336-multilevel-lumbar-laminectomies-with-noninstrumented-fusions/
Abstract
Background:Few reoperations are required in older patients undergoing multilevel lumbar laminectomy with noninstrumented fusions for spinal stenosis with/without spondylolisthesis/instability, and they rarely require instrumentation.
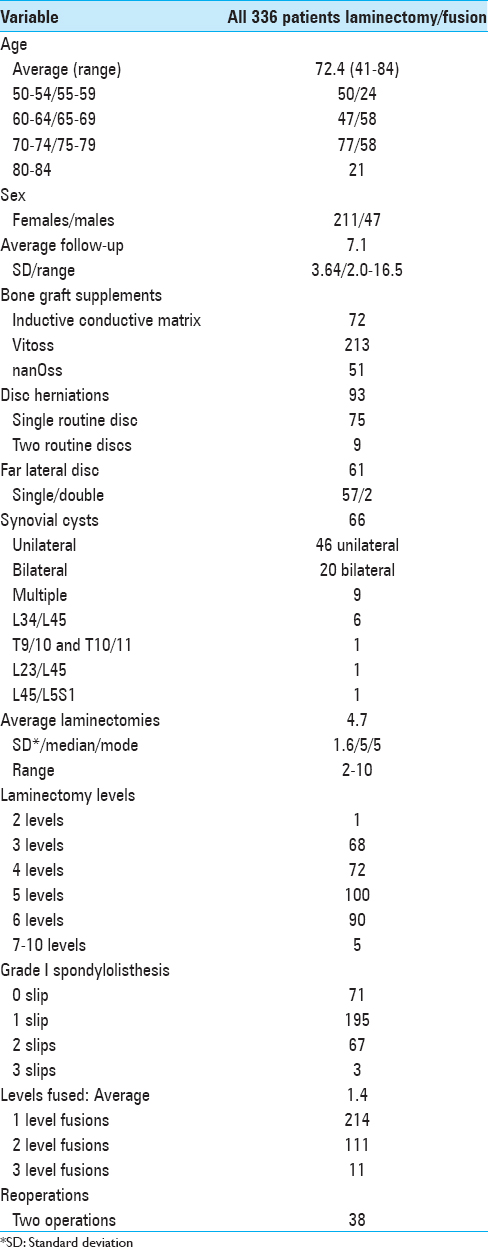
Methods:We reviewed 336 patients averaging 66.5 years of age undergoing initial average 4.7 level lumbar laminectomies with average 1.4 level noninstrumented fusions over an average 7.1-year period (range 2.0–16.5 years). Patients uniformly exhibited spinal stenosis, instability (Grade I [195 patients] or Grade II spondylolisthesis [67 patients]), disc herniations (154 patients), and/or synovial cysts (66 patients). Reoperations, including for adjacent segment disease (ASD), addressed new/recurrent pathology.
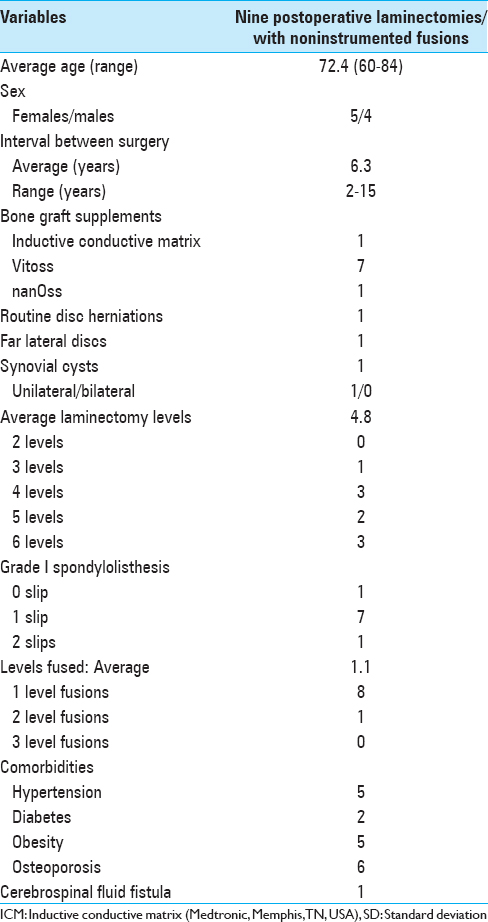
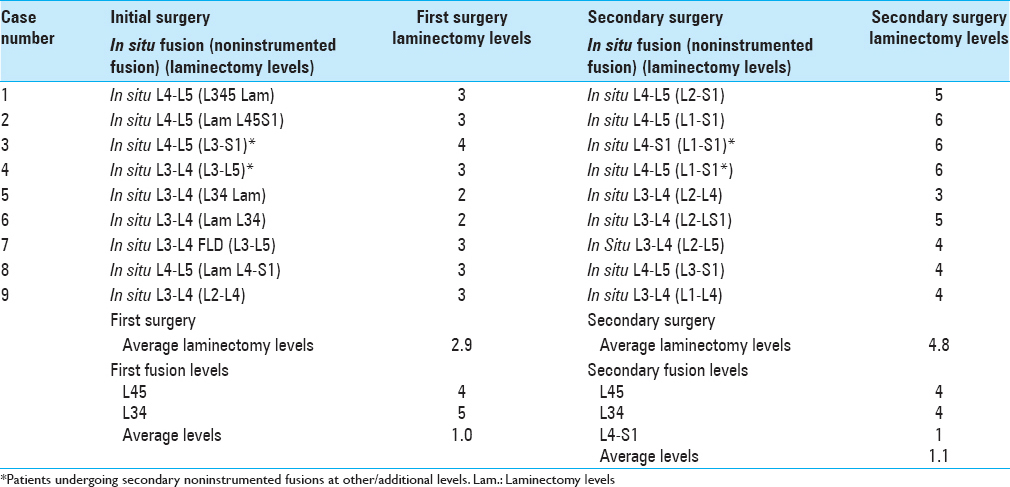
Results:Nine (2.7%) of 336 patients required reoperations, including for ASD, an average of 6.3 years (range 2–15 years) following initial 4.7 level laminectomies with 1.4 level noninstrumented fusions. Second operations warranted average 4.8 level (range 3–6) laminectomies and average 1.1 level non instrumented fusions addressing stenosis with instability (Grade I [7 patients] or Grade II [1 patient] spondylolisthesis), new disc herniations (2 patients), and/or a synovial cyst (1 patient).
Conclusions:Only 9 (2.7%) of 336 patients required reoperations (including for ASD) consisting of multilevel laminectomies with noninstrumented fusions for recurrent/new stenosis even with instability; these older patients were not typically unstable, or were likely already fused, and did not require instrumentation. Alternatively, reoperation rates following instrumented fusions in other series approached 80% at 5 postoperative years. Therefore, we as spinal surgeons should realize that older patients even with instability rarely require instrumentation and that the practice of performing instrumented fusions in everyone, irrespective of age, needs to stop.
Keywords: Adjacent segment disease, diskectomy, laminectomy, low reoperation rate, lumbar surgery, multilevel laminectomy, noninstrumented fusion, spondylolisthesis, synovial cysts
INTRODUCTION
Multilevel lumbar laminectomies with 1–2 level noninstrumented fusions with/without spondylolisthesis, offer a myriad of advantages particularly for geriatric patients with more comorbid risk factors including osteoporosis. The lack of instrumentation not only avoids implant loosening but also should markedly reduce the frequency of reoperations, including for adjacent segment disease (ASD). In Park et al., the risk of reoperations largely for ASD following no fusion/noninstrumented fusions (e.g., without pedicle screw instrumentation) was 5.2–5.6% (44.8 months postoperatively) whereas ASD after transpedicular fusions occurred in 12.2–18.5% of cases (average 164 months postoperatively).[
MATERIALS AND METHODS
Data from 336 patients undergoing multilevel laminectomy with noninstrumented fusions were collected over a 16.5-year period [
RESULTS
Nine (2.7%) patients required reoperations (including some for ASD) an average of 6.3 years after initial lumbar laminectomies with noninstrumented fusions [Tables
DISCUSSION
Summary of study
This study documented a very low 2.7% (9 patients) incidence of reoperations following 336 multilevel laminectomies with noninstrumented fusions performed in largely older patients averaging 72.4 years of age; the nine patients undergoing secondary surgery averaged 66.3 years of age [Tables
Better outcomes and low reoperation rates for lumbar laminectomy with/without predominantly noninstrumented fusions for spinal stenosis
Improved outcomes and low reoperation rates were documented for patients undergoing lumbar laminectomy with/without predominantly noninstrumented fusions for spinal stenosis.[
Low reoperation rates for noninstrumented versus high reoperation rates for instrumented fusions
Reoperation rates following noninstrumented lumbar fusions are typically lower than for instrumented fusions.[
Comparable or improved outcomes with noninstrumented versus instrumented fusions
Multiple studies document comparable or improved outcomes following noninstrumented versus instrumented fusions.[
Comparable 1–2 level fusion rates for noninstrumented versus instrumented fusion
Comparable 1–2 level fusion rates have been reported utilizing either noninstrumented versus instrumented fusions.[
Instrumented fusions, especially with interbody devices, correlate with high reoperation, and complication rates versus noninstrumented fusions
Higher reoperation and complication rates were reported for instrumented fusions, particularly utilizing interbody devices versus noninstrumented fusions.[
Noninstrumented fusions are more cost effective than instrumented fusions
In 2000, Kuntz et al. determined the average cost of noninstrumented fusions ($56,500 per quality-adjusted year of life [QALY]) versus instrumented fusions (QALY was $82,400); although instrumented fusions cost more, there were no clear-cut clinical advantages or documented “value added” for these procedures.[
SUMMARY
This study documented a 2.7% (9 patients) incidence of reoperations, including some for ASD, following 336 multilevel lumbar laminectomies with noninstrumented 1–2 level fusions for spinal stenosis with/without instability. These older patients, averaging 72.4 years of age (most age 65–79) with spondylolisthesis/instability and were not very unstable or were sufficiently spontaneously fused that no instrumented fusions were warranted [
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdu WA, Lurie JD, Spratt KF, Tosteson AN, Zhao W, Tosteson TD. Degenerative spondylolisthesis: Does fusion method influence outcome.Four-year results of the spine patient outcomes research trial?. Spine (Phila Pa 1976). 2009. 34: 2351-60
2. Andersen T, Christensen FB, Niedermann B, Helmig P, Høy K, Hansen ES. Impact of instrumentation in lumbar spinal fusion in elderly patients: 71 patients followed for 2-7 years. Acta Orthop. 2009. 80: 445-50
3. Axelsson P, Johnsson R, Strömqvist B, Arvidsson M, Herrlin K. Posterolateral lumbar fusion.Outcome of 71 consecutive operations after 4 (2-7) years. Acta Orthop Scand. 1994. 65: 309-14
4. Bydon M, Abt NB, De la Garza-Ramos R, Olorundare IO, McGovern K, Sciubba DM. Impact of age on short-term outcomes after lumbar fusion: An analysis of 1395 patients stratified by decade cohorts. Neurosurgery. 2015. 77: 347-53
5. Bydon M, Macki M, Abt NB, Sciubba DM, Wolinsky JP, Witham TF. Clinical and surgical outcomes after lumbar laminectomy: An analysis of 500 patients. Surg Neurol Int. 2015. 6: S190-3
6. Bydon M, Macki M, De la Garza-Ramos R, McGovern K, Sciubba DM, Wolinsky JP. Incidence of adjacent segment disease requiring reoperation after lumbar laminectomy without fusion: A study of 398 patients. Neurosurgery. 2016. 78: 192-9
7. Chaichana KL, Bydon M, Santiago-Dieppa DR, Hwang L, McLoughlin G, Sciubba DM. Risk of infection following posterior instrumented lumbar fusion for degenerative spine disease in 817 consecutive cases. Clin Neurol Neurosurg. 2015. 138: 117-23
8. Epstein NE, Epstein JA. SF-36 outcomes and fusion rates after multilevel laminectomies and 1 and 2-level instrumented posterolateral fusions using lamina autograft and demineralized bone matrix. J Spinal Disord Tech. 2007. 20: 139-45
9. Epstein NE. Fusion rates and SF-36 outcomes after multilevel laminectomy and noninstrumented lumbar fusions in a predominantly geriatric population. J Spinal Disord Tech. 2008. 21: 159-64
10. Jäger M, Seller K, Raab P, Krauspe R, Wild A. Clinical outcome in monosegmental fusion of degenerative lumbar instabilities: Instrumented versus non-instrumented. Med Sci Monit. 2003. 9: CR324-7
11. Katz JN, Lipson SJ, Lew RA, Grobler LJ, Weinstein JN, Brick GW. Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis.Patient selection, costs, and surgical outcomes. Spine (Phila Pa 1976). 1997. 22: 1123-31
12. Kuntz KM, Snider RK, Weinstein JN, Pope MH, Katz JN. Cost-effectiveness of fusion with and without instrumentation for patients with degenerative spondylolisthesis and spinal stenosis. Spine (Phila Pa 1976). 2000. 25: 1132-9
13. Macki M, Bydon M, Weingart R, Sciubba D, Wolinsky JP, Gokaslan ZL. Posterolateral fusion with interbody for lumbar spondylolisthesis is associated with less repeat surgery than posterolateral fusion alone. Clin Neurol Neurosurg. 2015. 138: 117-23
14. McGuire RA, Amundson GM. The use of primary internal fixation in spondylolisthesis. Spine (Phila Pa 1976). 1993. 18: 1662-72
15. Mehta VA, McGirt MJ, Garcés Ambrossi GL, Parker SL, Sciubba DM, Bydon A. Trans-foraminal versus posterior lumbar interbody fusion: Comparison of surgical morbidity. Neurol Res. 2011. 33: 38-42
16. Nakashima H, Kawakami N, Tsuji T, Ohara T, Suzuki Y, Saito T. Adjacent segment disease after posterior lumbar interbody fusion: Based on cases with a minimum of 10 years of follow-up. Spine (Phila Pa 1976). 2015. 40: E831-41
17. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine (Phila Pa 1976). 2004. 29: 1938-44
18. Santiago-Dieppa D, Bydon M, Xu R, De la Garza-Ramos R, Henry R, Sciubba DM. Long-term outcomes after non-instrumented lumbar arthrodesis. J Clin Neurosci. 2014. 21: 1393-7
19. Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis.Four-year results in the spine patient outcomes research trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009. 91: 1295-304
20. Ye YP, Chen D, Xu H. The comparison of instrumented and non-instrumented fusion in the treatment of lumbar spondylolisthesis: A meta-analysis. Eur Spine J. 2014. 23: 1918-26