- Department of Neurosurgery, University Hospital of Thessaly, University Hospital of Larissa, Larissa, Greece.
Correspondence Address:
George Fotakopoulos, Department of Neurosurgery, University Hospital of Thessaly, University Hospital of Larissa, Larissa, Greece.
DOI:10.25259/SNI_600_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: George Fotakopoulos, Alexandros Brotis, Kostas Andreas Fountas. Lumbar disc herniation presenting with fecal incontinence without radiculopathy: A case report. 19-Jul-2021;12:353
How to cite this URL: George Fotakopoulos, Alexandros Brotis, Kostas Andreas Fountas. Lumbar disc herniation presenting with fecal incontinence without radiculopathy: A case report. 19-Jul-2021;12:353. Available from: https://surgicalneurologyint.com/surgicalint-articles/10985/
Abstract
Background: Lumbar disc herniation (LDH) usually presents with lower extremity symptoms and signs, but rarely with bladder and bowel complaints. Here, we present a 61-year-old female who suffered solely from fecal incontinence (FI) attributed to a large LDH.
Case Description: The patient presented with FI, but had a normal neurological examination. When the lumbar magnetic resonance imaging of showed a large central L5S1 LDH, the patient underwent an urgent diskectomy. Six months later, her symptoms had improved.
Conclusion: Patients with large central LDHs may present with FI alone warranting urgent/emergent disc removal.
Keywords: Cauda equina syndrome, Fecal incontinence, Lumbar disc herniation
INTRODUCTION
Cauda equina syndromes (CESs) occur in from 1 to 3/100,000 patients. They are typically caused by herniated intervertebral lumbar discs at the L5-S1 level.[
CES, due to the lumbar discs, can be either complete or incomplete.[
Here, we present a 61-year-old female with FI alone attributed to a large L5S1 lumbar disc herniation (LDH), seen on magnetic resonance (MR) (i.e. without further symptoms/signs). Urgent decompression/diskectomy resulted in significant improvement of her deficit.
CASE REPORT
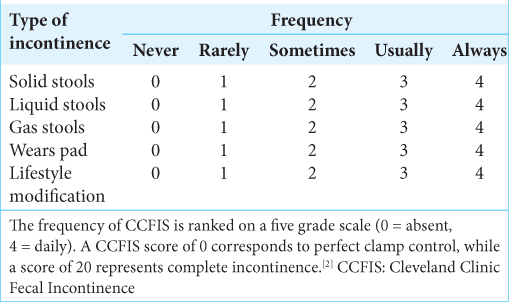
A 61-year-old female patient presented with FI of subacute onset (i.e. occurring up to 6 times a week) for the past 5 weeks (Cleveland Clinic Fecal Incontinence Score [CCFIS] 18; severe incontinence). She had no accompanying; back pain, saddle anesthesia, radiculopathy, myelopathy, or urinary incontinence.
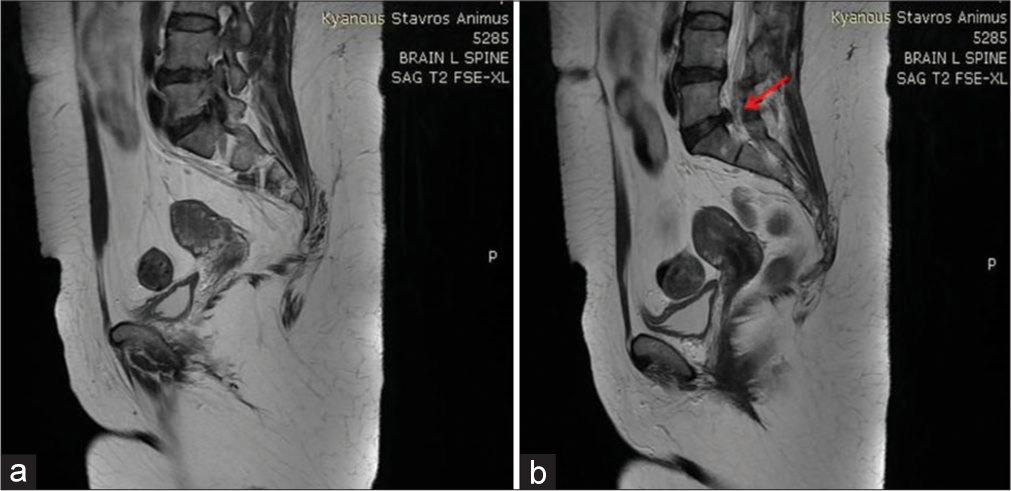
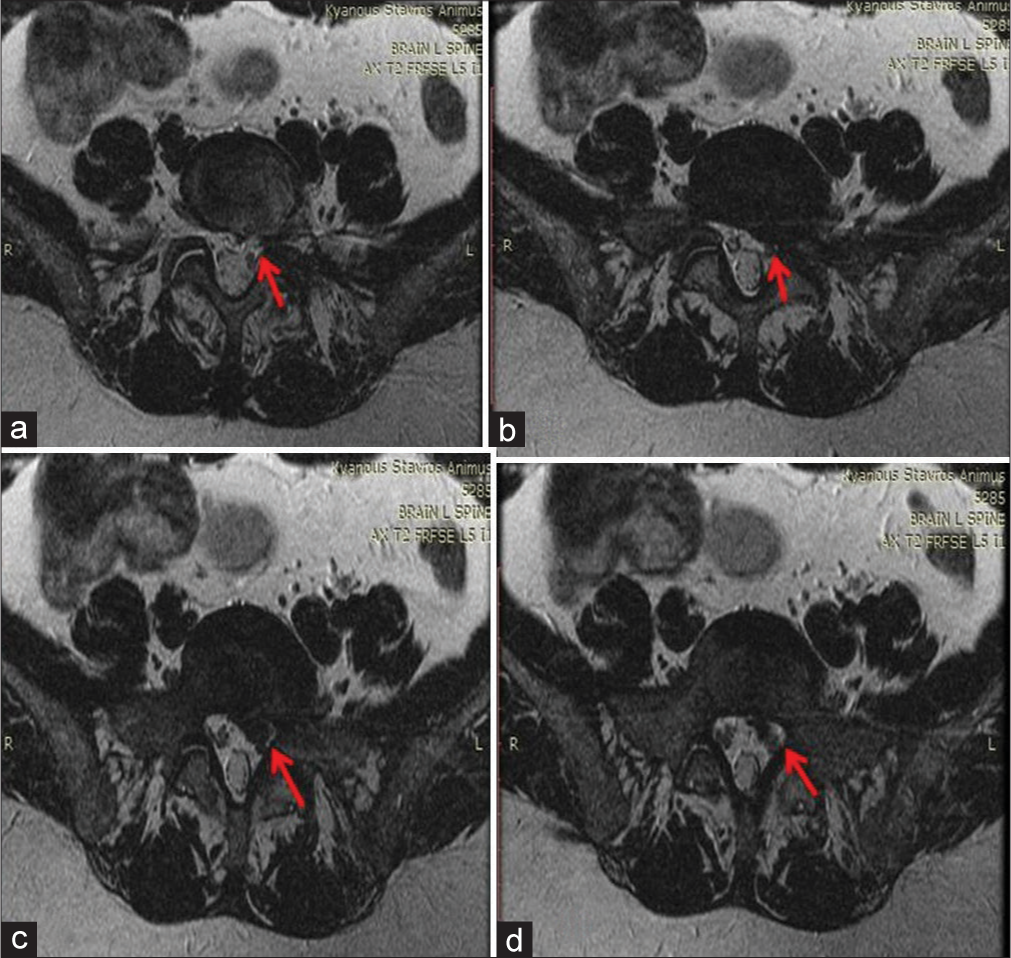
The high-resolution manometry (HRAM-pressure reading) of the anal canal and colonoscopy was normal. The MR imaging of the lumbar spine showed a large left-sided LDH at the L5-S1 level [
Figure 2:
A 61-year-old female patient was admitted with transient fecal incontinence and an asymptomatic lumbar disc herniation: (a-d) magnetic resonance imaging axial T2 thin slices 2.5 mm is sequence which was conducted with the abdomen coil after the observation of the existence of a hernia. A distracted intervertebral disk piece left, which presses the L5-S1 roots without creating vertebral stenosis (arrows).
DISCUSSION
Approximately 0.12% of the LDHs are likely to present with CES.[
CES, characterized by bladder and/or bowel dysfunction, saddle anesthesia, sexual dysfunction, and L5-S1 radiculopathy, is present in up to 2–6% of patients undergoing lumbar disc operations.[
Table 1:
CCFIS score.[
CONCLUSION
Patients with large L5S1 disc herniation may present with FI alone warranting urgent/emergent surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bharucha AE, Dunivan G, Goode PS, Lukacz ES, Markland AD, Matthews CA. Epidemiology, pathophysiology, and classification of fecal incontinence: State of the science summary for the national institute of diabetes and digestive and kidney diseases (NIDDK) workshop. Am J Gastroenterol. 2015. 110: 127-36
2. Dias AL, de Araújo FF, Cristante AF, Marcon RM, de Barros Filho TE, Letaif OB. Epidemiology of cauda equina syndrome. What changed until 2015. Rev Bras Ortop. 2018. 53: 107-12
3. Gardner A, Gardner E, Morley T. Cauda equina syndrome: A review of the current clinical and medico-legal position. Eur Spine J. 2011. 20: 690-7
4. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993. 36: 77-97
5. Kapetanakis S, Chaniotakis C, Kazakos C, Papathanasiou JV. Cauda equina syndrome due to lumbar disc herniation: A review of literature. Folia Med (Plovdiv). 2017. 59: 377-86
6. Lavy C, James A, Wilson-MacDonald J, Fairbank J. Cauda equina syndrome. BMJ. 2009. 338: b936
7. Long B, Koyfman A, Gottlieb M. Evaluation and management of cauda equina syndrome in the emergency department. Am J Emerg Med. 2020. 38: 143-8