- Department of Neurosurgery, Maastricht University Medical Center, Maastricht, Netherlands.
- Department of Pathology, Maastricht University Medical Center, Maastricht, Netherlands.
Correspondence Address:
Sem M. M. Hermans, Department of Neurosurgery, Maastricht University Medical Center, Maastricht, Netherlands.
DOI:10.25259/SNI_85_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sem M. M. Hermans1, Jasper van Aalst1, Jan Beckervordersandforth2, Tim A. M. Bouwens van der Vlis1. Lumbar spinal stenosis in a patient with complex spinal dysraphism caused by a supplementary midline muscle: A case report. 31-Mar-2022;13:121
How to cite this URL: Sem M. M. Hermans1, Jasper van Aalst1, Jan Beckervordersandforth2, Tim A. M. Bouwens van der Vlis1. Lumbar spinal stenosis in a patient with complex spinal dysraphism caused by a supplementary midline muscle: A case report. 31-Mar-2022;13:121. Available from: https://surgicalneurologyint.com/surgicalint-articles/11498/
Abstract
Background: The clinical tethered cord syndrome (TCS) can become symptomatic during adulthood, known as adult tethered cord syndrome (ATCS). Distinguishing ATCS from neurogenic claudication attributed to lumbar spinal stenosis may pose a clinical challenge.
Case Description: A 66-year-old male with an underlying complex occult spinal dysraphism (OSD) presented with new onset of lower back and bilateral leg pain plus neurogenic claudication. Magnetic resonance imaging documented OSD, and lumbar spinal stenosis (LSS) attributed to a supplementary midline muscle. Following decompressive surgery for LSS without untethering the ATCS, the patient’s symptoms resolved.
Conclusion: A patient with OSD and ATCS with LSS due to a supplementary midline muscle presented with new onset of neurogenic claudication. Surgical decompression of the LSS by removing the supplementary midline muscle resolved patients’ symptoms.
Keywords: Decompressive surgery, Neurogenic claudication, Spinal dysraphism, Spinal stenosis, Supplementary midline muscle, Tethered cord
INTRODUCTION
Clinically, occult spinal dysraphism (OSD) may be associated with the clinical tethered cord syndrome (TCS) which includes pain, symptoms of motor and sensory loss in the lower extremities, and bladder dysfunction.[
CASE REPORT
Clinical presentation
A 66-year-old male presented with neurogenic claudication characterized as lower back and bilateral leg pain. The patient had a known complex OSD that included ATCS and multiple other congenital anomalies. Consequently, the left leg was shortened and atrophied. Further neurological examination revealed diffuse weakness 4/5 in both legs, absence of the left patellar and Achilles responses, and an unsteady gait.
Imaging
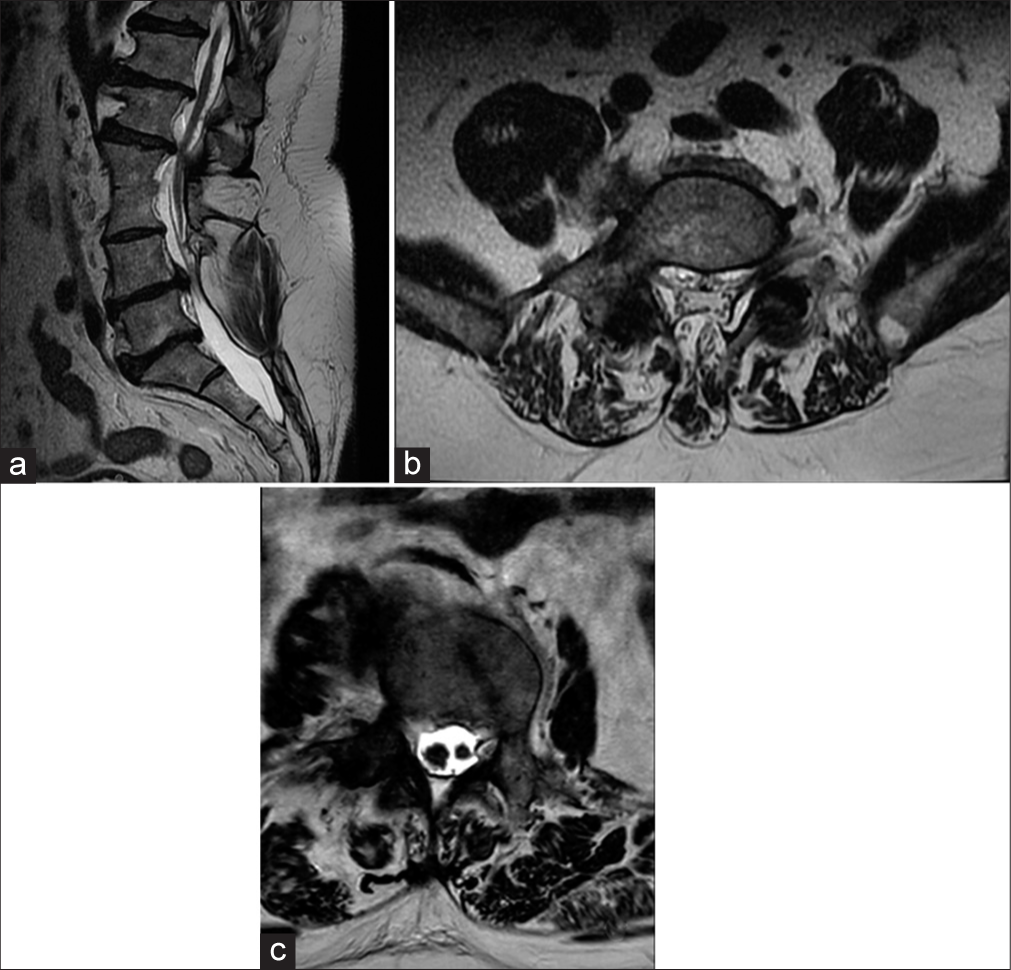
MRI of the lumbar spine revealed OSD in combination with spondylotic changes [
Figure 1:
(a) Preoperative sagittal MRI T2 scan showing fusion of the L2 and L3 vertebrae, hemivertebrae of L4 and L5, unfused spinous process L2, an interspinosal lipoma at the level of L3, and a tethered cord. (b) Preoperative axial MRI T2 scan L4-L5. The midline muscular abnormality causes spinal cord compression. Furthermore, a left foraminal stenosis is seen. (c) Preoperative axial MRI T2 scan L1 showing diastematomyelia of the spinal cord.
Surgery
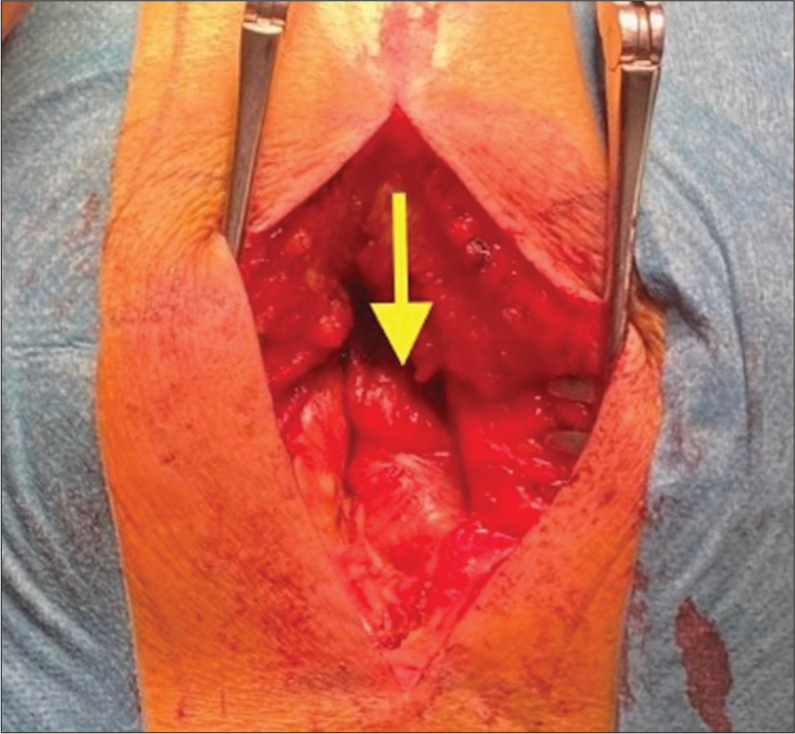
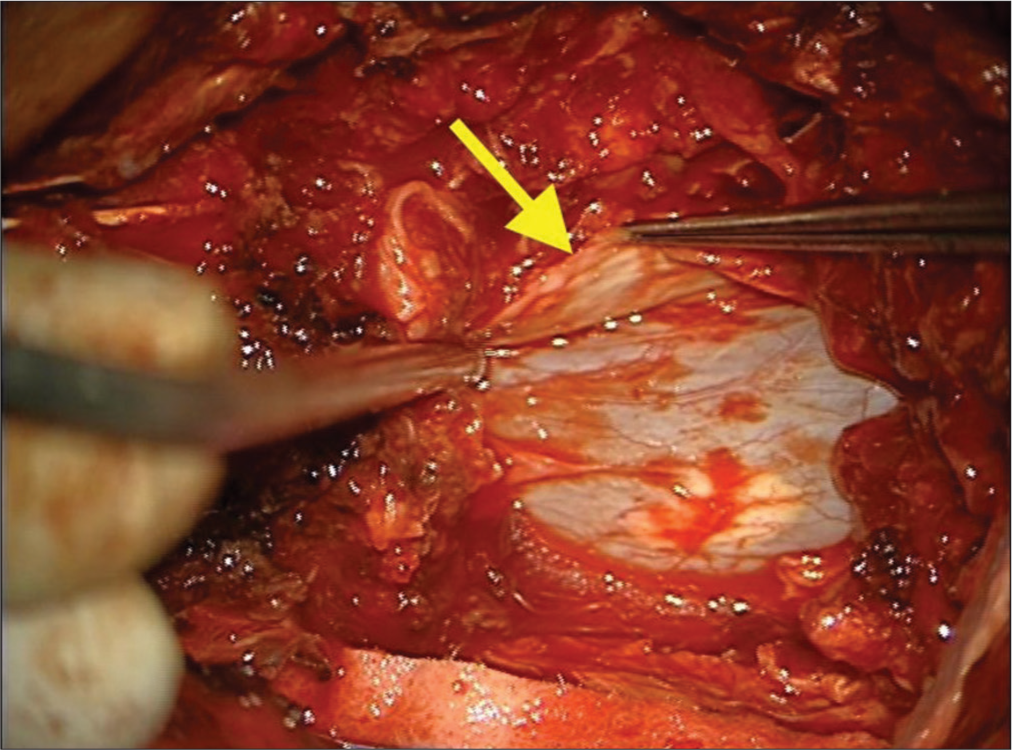
The spinal canal was approached from the left side through a L4/L5 hemi-laminectomy [
Outcome
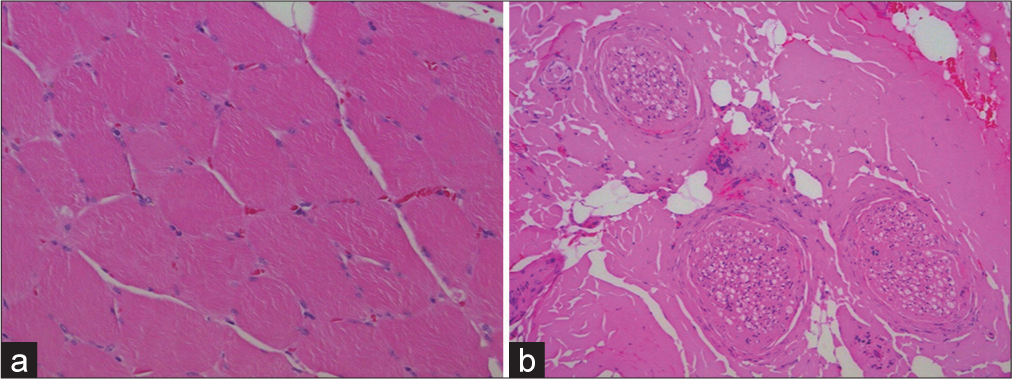
Postoperatively, the patient experienced transient complaint of a left-sided lateral femoral cutaneous nerve entrapment syndrome, which resolved spontaneously. The patient was discharged 2 days later, and 2 months later reported a significant reduction in neurogenic claudication. The pathology report confirmed that the tissue removed was normal muscle tissue [
DISCUSSION
The patient in this report was known to have complex surgically untreated OSD in conjunction with multiple other congenital anomalies including ATCS and a hemivertebrae at the L4/L5 level. Due to direct muscle adherence to the dura through the L4/L5 hemivertebral defect, the patient had developed new symptoms of neurogenic claudication. Following the lysis of these adhesions and decompression of the L4/L5 lumbar canal, the patient’s symptoms significantly improved (i.e., within 2 postoperative months).
Etiology of supplementary midline muscle
The developmental mechanism of the supplementary midline muscle in our patient remained unclear. The muscle was located in midline at L5 and extended in the spinal canal through the hemivertebrae of L4 and L5. Possibly, during the development of the spine, the hemivertebrae provided extra space, which was then filled up by the supplementary muscle, or vice versa, the muscle was obstruent for the vertebrae to correctly develop.
CONCLUSION
A 66-year-old male with OSD and multiple congenital anomalies (i.e., including a hemivertebrae at L4/L5) presented with new onset of neurogenic claudication and symptoms/ signs of lumbar stenosis. As the MR revealed adherence of the midline musculature to the dura through the L4/ L5 hemivertebral defect, the patient’s stenosis was relieved following a lysis of these adhesions and canal decompression at the L4/5 level.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurg Clin N Am. 2007. 18: 531-47
2. Aufschnaiter K, Fellner F, Wurm G. Surgery in adult onset tethered cord syndrome (ATCS): Review of literature on occasion of an exceptional case. Neurosurg Rev. 2008. 31: 371-83