- Physician, Intensive Care Unit, Fundación Valle del Lili, Cali, Colombia
- Physician, CIDEIM, International Biomedical Research Center, Cali, Colombia
- Pathologist, Fundación Valle del Lili, Professor of Pathology, Universidad ICESI, Fundación Valle del Lili, Cali, Colombia
- Neurosurgeon, Fundación Valle del Lili, Professor of Neuroanatomy and Neurosurgery, Universidad ICESI, Cali, Colombia
Correspondence Address:
Javier Lobato-Polo
Neurosurgeon, Fundación Valle del Lili, Professor of Neuroanatomy and Neurosurgery, Universidad ICESI, Cali, Colombia
DOI:10.4103/2152-7806.189732
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Quinones E, Potes LI, Silva N, Lobato-Polo J. Lymphomatoid granulomatosis of the brain: A case report. Surg Neurol Int 01-Sep-2016;7:
How to cite this URL: Quinones E, Potes LI, Silva N, Lobato-Polo J. Lymphomatoid granulomatosis of the brain: A case report. Surg Neurol Int 01-Sep-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/lymphomatoid-granulomatosis-brain-case-report/
Abstract
Background:Lymphomatoid granulomatosis is a rare disorder of the central nervous system (CNS) with few cases being reported in literature. We present the case of an adult with an unusual lesion of the CNS who presented with motor seizures and was diagnosed with lymphomatoid granulomatosis, followed by a discussion of the process of evaluation and management.
Case Description:A 42-year-old male presented with motor seizures and loss of consciousness for 10 minutes along with dysarthria and left hemiplegia. Neurological examination and imaging with magnetic resonance imaging (MRI) of the brain revealed a mass in the right striatum. The patient was hospitalized and underwent an image-guided right frontal craniotomy using the Leksell Stereotactic G-Frame. Pathology reported a lymphomatoid granulomatosis. Being immunocompetent, the patient received medical treatment with prednisone and rituximab. Two years after his diagnosis, the patient had no active disease and his brain MRI did not show contrast enhancement. After almost 3 years of follow-up, the patient has a mild weakness in the left-side of his body (4/5), is seizure-free, and can walk and perform daily activities.
Conclusions:This rare lesion in an adult, immunocompetent patient, debuting with motor seizures represents a challenge in terms of diagnosis and treatment. After surgical and medical treatment, the patient had a satisfactory recovery. Clinical features, imaging, differential diagnosis, and pathology are discussed.
Keywords: Brain tumor, lymphomatoid granulomatosis, stereotactic neurosurgery, symptomatic epilepsy
INTRODUCTION
Lymphomatoid granulomatosis (LG) is a disease that was first described in 1972 by Liebow et al.,[
Because there is still much to be learned about this disease, we present the following case along with a detailed description of its radiological, pathological, and clinical findings.
CASE REPORT
A 42-year-old man, previously healthy, was living with his step father and other members of an extended family in a small farm. He presented with a first episode of a motor seizure that started on the left side of his body before becoming generalized. Shortly afterwards, he noticed left hemiparesis and dysarthria; he was admitted to our institution through the emergency department.
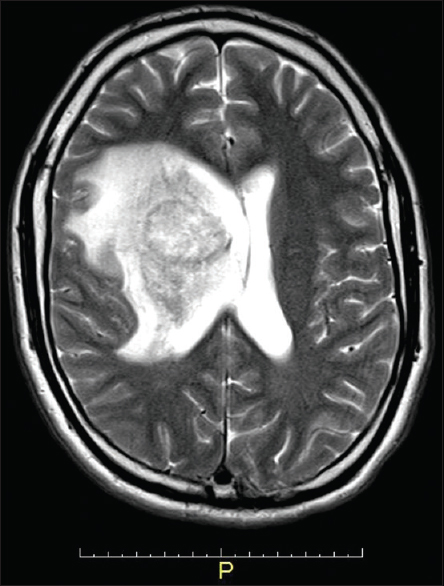
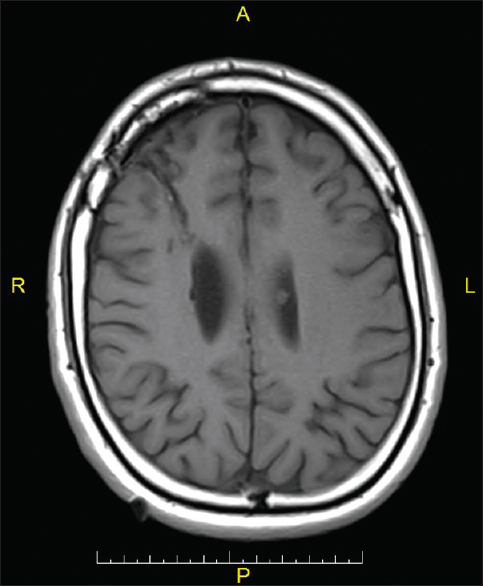
After a physical examination, magnetic resonance imaging (MRI) of the patient revealed a well-defined, spherical lesion, located in the superior aspect of the anterior limb of the internal capsule and right striatum, with surrounding edema [
Figure 1
Magnetic resonance T1 image. A round-shaped, well-limited lesion, with contrast enhancement, located in the right striatum besides the the lateral ventricle with compressive effect on the brain parenchyma and adjacent structures deviation midline approximately 8.0 mm. Surrounding edema is observed
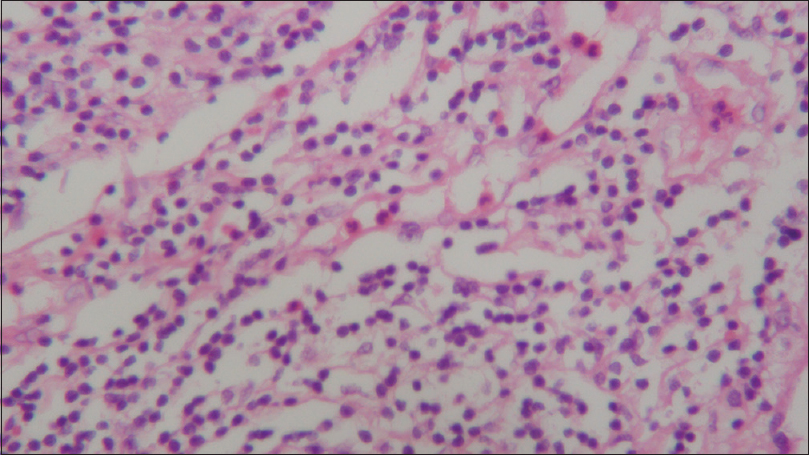
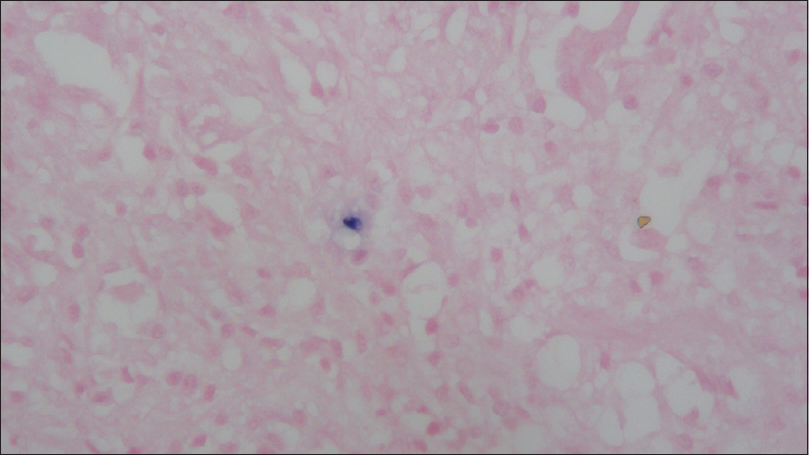
In the pathological analysis, there was an evident atypical T and B infiltrate; morphological and phenotypical characteristics of Grade 1 lymphomatoid granulomatosis. The patient was subjected to thoracic and abdominal screening, which revealed paratracheal, jugular, and inguinal adenopathies, but no other masses.
After consulting with the hematology group, the patient received a four-cycle medical treatment with rituximab and prednisone. Clinically, he recovered almost completely with strength of 4/5 and complete reintegration to his daily activities, which involved bimanual work. Six months after his diagnosis, a new MRI showed the absence of new or residual lesions.
Two years after the surgery the patient continued to be free of seizures, and his MRI showed no evidence of new lesions, areas of restriction of diffusion, or anomalous enhancements that could indicate residual or recurrent tumor [
DISCUSSION
LG is a lymphoproliferative disorder, in which tumorous B cells transform after infection with the Epstein-Barr virus.[
The pathogenesis of LG is unknown. Studies based on clinicopathological, immunophenotypic, and clonal evidence have shown that this is a unique type of extranodal, malignant lymphoma.[
LG can be graded based on the relative amount of tumor reactive cells and accompanying tumor cells.[
Radiological, lymphomatoid granulomatosis (LG) appearance in a brain computed tomography (CT) varies. It is common to find intraparenchymal lesions, which may be unilateral or multifocal, supra or infratentorial. These lesions may appear as low-density areas within the cerebral white matter; they may be solid or ring-like, sometimes with accompanying edema.[
Because of its angiocentric and angiodestructive character, LG can debut with intraparenchymal hemorrhage, stroke, or aneurysms.[
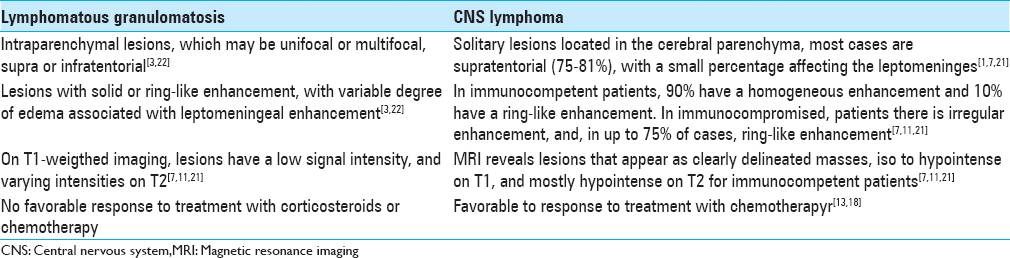
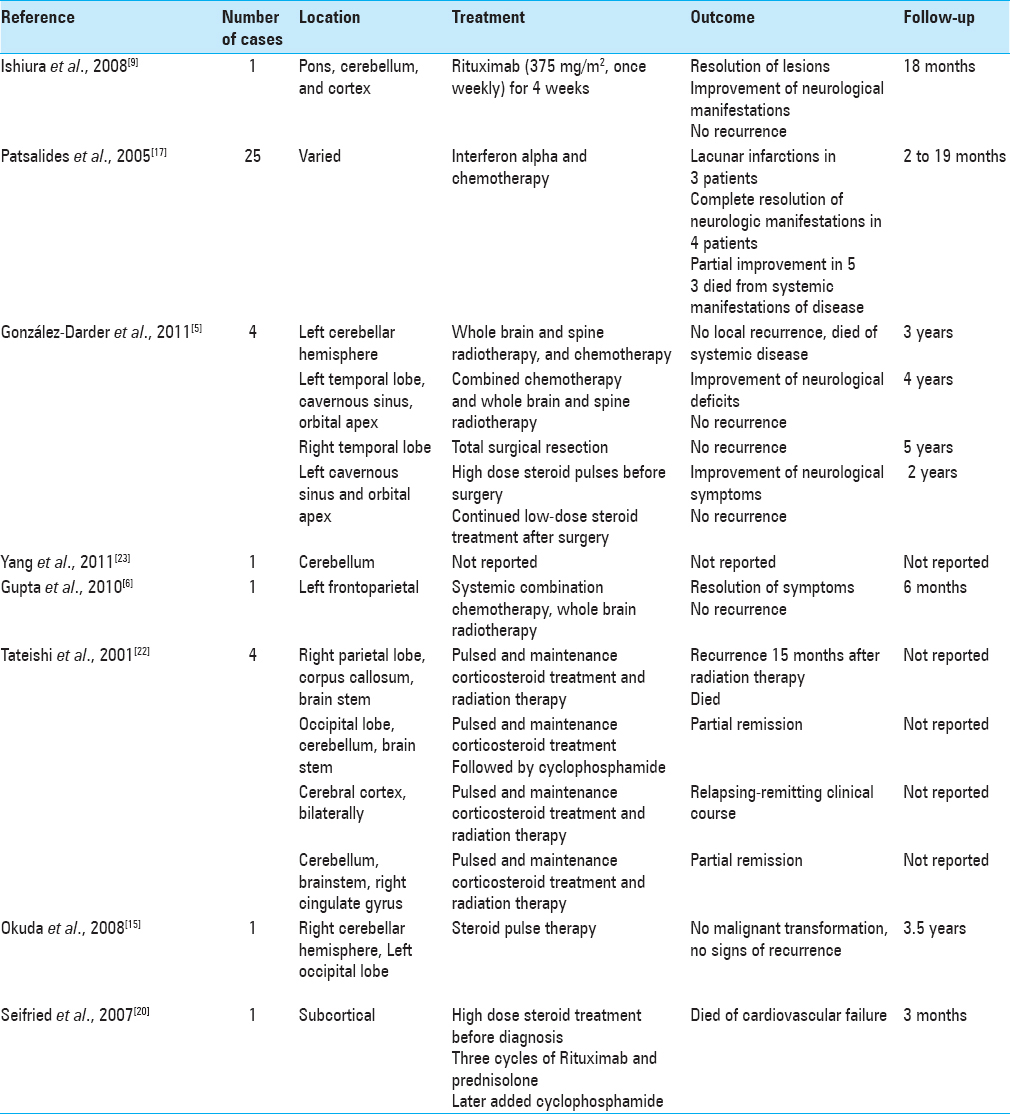
LG and CNS lymphoma share similar radiological features that may be difficult to distinguish on an MRI or CT image [
Our patient, unlike what literature reports [
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ayuso-Peralta L, Orti-Pareja M, Zurdo-Hernandez M, Jimenez-Jimenez FJ, Tejeiro-Martinez J, Ricoy JR. Cerebral lymphoma presenting as a leukoencephalopathy. J Neurol Neurosurg Psychiatry. 2001. 71: 243-6
2. Batchelor TT, Grossman SA, Mikkelsen T, Ye X, Desideri S, Lesser GJ. Rituximab monotherapy for patients with recurrent primary CNS lymphoma. Neurology. 2011. 76: 929-30
3. George JC, Caldemeyer KS, Smith RR, Czaja JT. CNS lymphomatoid granulomatosis in AIDS: CT and MR appearances. AJR Am J Roentgenol. 1993. 161: 381-3
4. Gimeno J, Alameda F, García M, Bellosillo B, Juanpere N, López L. Granulomatosis linfomatoide con presentación neurológica. A propósito de un caso y revisión de la literatura. Revista Españla de Patología. 2010. 43: 114-9
5. González-Darder JM, Vera-Román JM, Pesudo-Martínez JV, Cerdá-Nicolás M, Ochoa E. Tumoral presentation of primary central nervous system lymphomatoid granulomatosis. Acta neurochirurgica. 2011. 153: 1963-1970
6. Gupta T, Wadasadawala T, Shet T, Jalali R, Menon H. Isolated central nervous system involvement by lymphomatoid granulomatosis in an adolescent: A case report and review of literature. Pediatr Hematol Oncol. 2010. 27: 150-9
7. Haldorsen IS, Espeland A, Larsson EM. Central nervous system lymphoma: Characteristic findings on traditional and advanced imaging. AJNR Am J Neuroradiol. 2011. 32: 984-92
8. Hamilton MG, Demetrick DJ, Tranmer BI, Curry B. Isolated cerebellar lymphomatoid granulomatosis progressing to malignant lymphoma. Case report. J Neurosurg. 1994. 80: 314-20
9. Ishiura H, Morikawa M, Hamada M, Watanabe T, Kako S, Chiba S. Lymphomatoid granulomatosis involving central nervous system successfully treated with rituximab alone. Arch Neurol. 2008. 65: 662-5
10. Kerr RS, Hughes JT, Blamires T, Teddy PJ. Lymphomatoid granulomatosis apparently confined to one temporal lobe. Case report. J Neurosurg. 1987. 67: 612-5
11. Koeller KK, Smirniotopoulos JG, Jones RV. Primary central nervous system lymphoma: Radiologic-pathologic correlation. Radiographics. 1997. 17: 1497-526
12. Lee JS, Tuder R, Lynch DA. Lymphomatoid granulomatosis: Radiologic features and pathologic correlations. AJR Am J Roentgenol. 2000. 175: 1335-9
13. Liebow AA. Lymphomatoid granulomatosis. Calif Med. 1972. 116: 48-9
14. Lucantoni C, De Bonis P, Doglietto F, Esposito G, Larocca LM, Mangiola A. Primary cerebral lymphomatoid granulomatosis: Report of four cases and literature review. J Neurooncol. 2009. 94: 235-42
15. Okuda T, Akai F, Kataoka K, Taneda M. A case of lymphomatoid granulomatosis followed for 14 months on the basis of clinical and histological findings. Brain Tumor Pathol. 2008. 25: 33-8
16. Olusina D, Ezemba N, Nzegwu MA. Pulmonary lymphomatoid granulomatosis: Report of a case and review of literature. Niger Med J. 2011. 52: 60-3
17. Patsalides AD, Atac G, Hedge U, Janik J, Grant N, Jaffe ES. Lymphomatoid granulomatosis: Abnormalities of the brain at MR imaging 1. Radiology. 2005. 237: 265-73
18. Rubenstein JL, Gupta NK, Mannis GN, Lamarre AK, Treseler P. How I treat CNS lymphomas. Blood. 2013. 122: 2318-30
19. Schalper KA, Valbuena JR. [Primary cerebral lymphomatoid granulomatosis in a HIV-positive patient. Case report]. Rev Med Chil. 2011. 139: 218-23
20. Seifried C, Weidauer S, Hinsch N, Bug R, Steinmetz H. [Cerebral lymphomatoid granulomatosis. A case report]. Nervenarzt. 2007. 78: 193-7
21. Slone HW, Blake JJ, Shah R, Guttikonda S, Bourekas EC. CT and MRI findings of intracranial lymphoma. AJR Am J Roentgenol. 2005. 184: 1679-85
22. Tateishi U, Terae S, Ogata A, Sawamura Y, Suzuki Y, Abe S. MR imaging of the brain in lymphomatoid granulomatosis. AJNR Am J Neuroradiol. 2001. 22: 1283-90
23. Yang J, Shin S, Fowkes M, Krieger S, Strauchen JA, Smethurst M. Teaching NeuroImages: Lymphomatoid granulomatosis involving lung and brain in an immunocompetent woman. Neurology. 2011. 77: e75-6