- Department of Neurosurgery, Royal Prince Alfred Hospital, Camperdown, New South Wales, Australia.
- Department of Ear Nose and Throat, Royal Prince Alfred Hospital, Camperdown, New South Wales, Australia.
- Department of Radiology, Royal Prince Alfred Hospital, Camperdown, New South Wales, Australia.
Correspondence Address:
Elissa Xian, Department of Neurosurgery, Royal Prince Alfred Hospital, Camperdown, New South Wales, Australia.
DOI:10.25259/SNI_32_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Elissa Xian1, Joel Hardman2, Geoffrey Parker3, Arjuna Nirmalananda2. Management of cerebrospinal fluid rhinorrhea as a rare complication of antiphospholipid syndrome. 01-Mar-2024;15:61
How to cite this URL: Elissa Xian1, Joel Hardman2, Geoffrey Parker3, Arjuna Nirmalananda2. Management of cerebrospinal fluid rhinorrhea as a rare complication of antiphospholipid syndrome. 01-Mar-2024;15:61. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12783
Abstract
Background: Antiphospholipid syndrome is a complex autoimmune condition associated with the formation of recurrent thrombosis in any vascular bed throughout the body. Jugular vein thrombosis is very rare with only a 0.9% occurrence and is not typically associated with cerebrospinal rhinorrhea as a result of raised intracranial pressure.
Case Description: A 54-year-old patient presented with a 9-month history of cerebrospinal fluid (CSF) rhinorrhea and headache on a background of antiphospholipid syndrome. Investigations showed a superior vena cava (SVC) and right internal jugular vein (IJV) obstruction with moderately elevated intracranial venous pressures. Her magnetic resonance imaging (MRI) brain was consistent with a CSF leak. The patient underwent successful endovascular stenting of her obstructed SVC and right IJV followed by surgical repair of a herniating meningocele in the posterior left ethmoid air cells.
Conclusion: CSF rhinorrhea is uncommon and never previously reported associated with SVC thrombosis induced by antiphospholipid syndrome. A combination of endovascular techniques and surgical repair is recommended for this challenging presentation.
Keywords: Antiphospholipid syndrome, Cerebrospinal fluid rhinorrhea, Endovascular stenting, Superior vena cava obstruction
INTRODUCTION
Cerebrospinal fluid (CSF) rhinorrhea is an uncommon condition classified as either traumatic or nontraumatic and is the result of a pathway formed between the subarachnoid space and the nasopharynx or nasal cavity. Traumatic causes include blunt force injuries and surgical complications.[
Antiphospholipid syndrome is a complex autoimmune condition with complications, including the formation of recurrent thrombosis in any vascular bed throughout the body.[
We present an unusual case of a patient who presented with CSF rhinorrhea secondary to raised ICP as a result of an SVC and right IJV thrombosis due to antiphospholipid syndrome.
CASE PRESENTATION
A 54-year-old female presented with a 9-month history of spontaneous CSF rhinorrhea associated with blurred vision and headache. This is on a background of antiphospholipid syndrome for which she requires life-long anti-coagulation with warfarin. She also has a history of several deep vein thromboses and pulmonary emboli as well as a near total, chronic thrombosis of her SVC.
Investigations and treatment
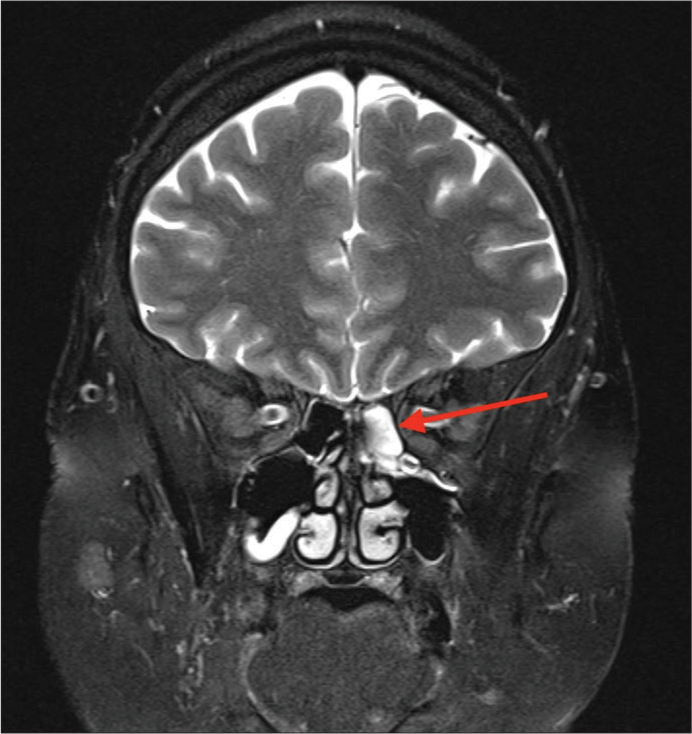
She was admitted to the hospital and investigated with an MRI brain demonstrating fluid in the left posterior ethmoid air cells as well as optic nerve sheath enlargement bilaterally, consistent with intracranial hypertension and CSF leak [
Based on the clinical and radiological findings, a multidisciplinary decision was made to proceed with a combined interventional neuroradiology procedure to stent the SVC and right IJV before endoscopic endonasal repair of the skull base defect.
Under general anesthetic, a 6F Cook Shuttle sheath was introduced through the right common femoral vein. A second venotomy was performed with a 5F short sheath placed in the right IJV and a venography showed severe stenosis of the right IJV at the level of C4 with extensive collaterals flowing into a distended azygos vein. A second severe stenosis was noted in the SVC above the junction with the azygos vein. A communicating channel between the upper and lower SVC was selected from above with a 035 guide wire and an Amplatz super stiff exchange wire was passed to the right common iliac vein. A 10F short sheath was exchanged into the right common femoral vein and a Gooseneck 15 mm device was used to ensnare the exchange wire. Graduated balloon angioplasty (6 mm × 40 mm and 10 mm × 40 mm Advance balloons) of the stenosed SVC was performed and a 16 mm × 40 mm Venovo stent was subsequently deployed over the narrowed segment. A post-stent angioplasty was also completed with a 14 mm × 40 mm XXL balloon. The stenosed section of the right IJV also underwent balloon dilatation (12 mm × 40 mm Advance balloon).
Successful stenting of the patient’s SVC and balloon dilatation of her right IJV [
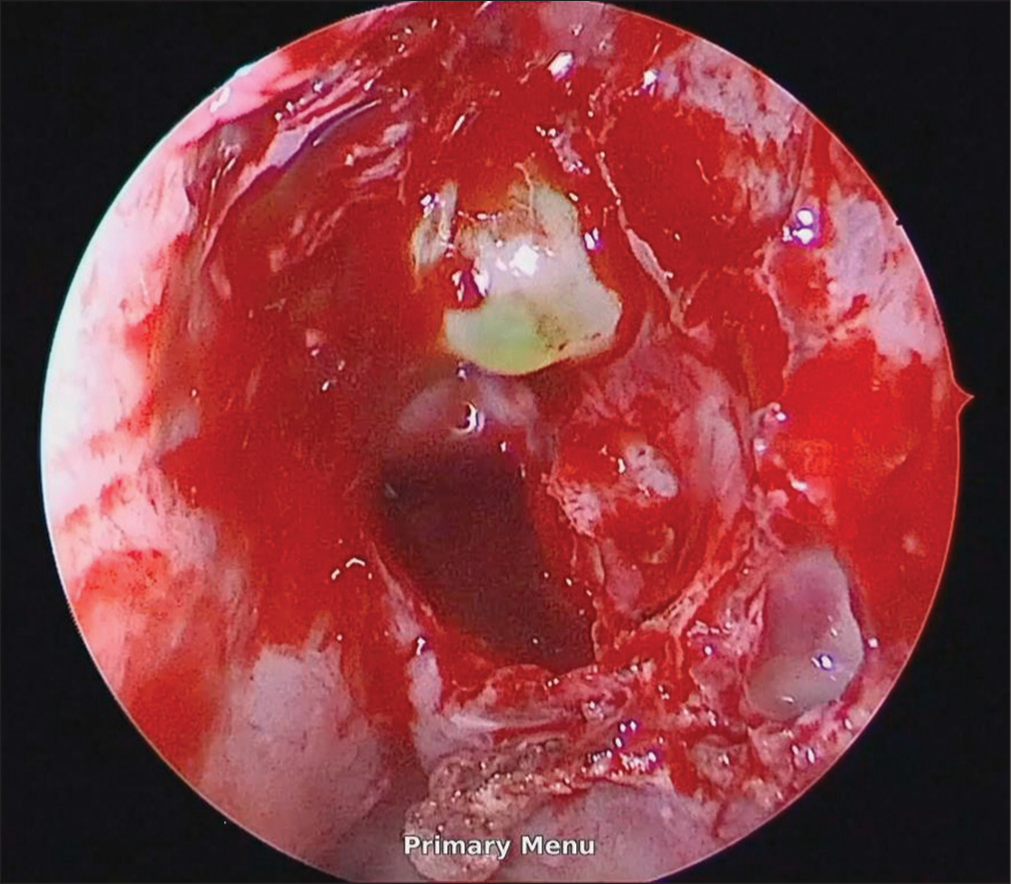
A preoperative intrathecal injection of fluorescein was used to localize the origin of the leak. An endoscopic approach was employed with a left antrostomy and bilateral ethmoidectomy performed to access the posterior ethmoid space. The source of the leak was identified as a herniating meningocele in the left posterior ethmoid [
Outcome and follow-up
Following the operation, the patient recovered well and her symptoms continue to improve. There was no further rhinorrhea. She was commenced on a heparin infusion postoperatively and then converted to aspirin and warfarin. She was followed up 6 weeks post-intervention with complete resolution of her CSF leak as well as headache and vision. Her postoperative MRI demonstrated an adequate septal flap placement and replacement of the previous posterior ethmoid fluid with diffuse postoperative changes of chronic sinusitis. Contrast computed tomography of the chest confirmed the patency of the SVC stent. She was returned to her hematologist for the long-term management of her antiphospholipid syndrome.
DISCUSSION
CSF rhinorrhea is an uncommon presentation that can result in serious complications such as bacterial meningitis if left untreated.[
There has not been a published case describing a patient whose antiphospholipid syndrome was associated with the incidence of CSF rhinorrhea. This may be due to the rarity of chronic nonmalignant SVC syndrome induced by antiphospholipid syndrome resulting in CSF rhinorrhea.[
Surgical endoscopic endonasal repair is the preferred treatment method with good outcomes for most causes of CSF rhinorrhea.[
CONCLUSION
CSF rhinorrhea secondary to SVC obstruction resulting from antiphospholipid syndrome has never been reported in the literature. Surgery is the main treatment modality for CSF leak; however, in this case, stent treatment for the SVC obstruction was also required to alleviate the patient’s raised ICP. Therefore, a combined endovascular and surgical approach is recommended for this challenging presentation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Amiral J, Peyrafitte M, Dunois C, Vissac AM, Seghatchian J. Anti-phospholipid syndrome: Current opinion on mechanisms involved, laboratory characterization and diagnostic aspects. Transfus Apher Sci. 2017. 56: 612-25
2. Banu MA, Kim JH, Shin BJ, Woodworth GF, Anand VK, Schwartz TH. Low-dose intrathecal fluorescein and etiology-based graft choice in endoscopic endonasal closure of CSF leaks. Clin Neurol Neurosurg. 2014. 116: 28-34
3. Ducros A, Biousse V. Headache arising from idiopathic changes in CSF pressure. Lancet Neurol. 2015. 14: 655-68
4. Flint PW, Haughey BH, Lund VJ, Robbins KT, Thomas JR, Francis HW, editors. Cummings otolaryngology: Head and neck surgery. Netherlands: Elsevier; 2020. p.
5. Gómez-Puerta JA, Cervera R. Diagnosis and classification of the antiphospholipid syndrome. J Autoimmun. 2014. 48-49: 20-5
6. Gonen L, Monteiro E, Klironomos G, Alghonaim Y, Vescan A, Zadeh G. Endoscopic endonasal repair of spontaneous and traumatic cerebrospinal fluid rhinorrhea: A review and local experience. Neurosurg Clin N Am. 2015. 26: 333-48
7. Rizvi AZ, Kalra M, Bjarnason H, Bower TC, Schleck C, Gloviczki P. Benign superior vena cava syndrome: Stenting is now the first line of treatment. J Vasc Surg. 2008. 47: 372-80
8. Sfyroeras GS, Antonopoulos CN, Mantas G, Moulakakis KG, Kakisis JD, Brountzos E. A review of open and endovascular treatment of superior vena cava syndrome of benign aetiology. Eur J Vasc Endovasc Surg. 2017. 53: 238-54
9. Sharma SD, Kumar G, Bal J, Eweiss A. Endoscopic repair of cerebrospinal fluid rhinorrhoea. Eur Ann Otorhinolaryngol Head Neck Dis. 2016. 133: 187-90