- Department of Anesthesiology, Advocate Illinois Masonic Medical Center, Chicago, Illinois, USA
- Ghaly Neurosurgical Associates, Aurora, Chicago, Illinois, USA
- Department of Anesthesiology, University of Illinois, Chicago, Illinois, USA
Correspondence Address:
Ramsis F. Ghaly
Department of Anesthesiology, Advocate Illinois Masonic Medical Center, Chicago, Illinois, USA
Department of Anesthesiology, University of Illinois, Chicago, Illinois, USA
DOI:10.4103/sni.sni_357_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ramsis F. Ghaly, Armen Haroutunian, Kenneth D. Candido, Nebojsa Nick Knezevic. Management of concomitant metabolic encephalopathy and meningioma with vasogenic edema and impending herniation. 08-Feb-2018;9:25
How to cite this URL: Ramsis F. Ghaly, Armen Haroutunian, Kenneth D. Candido, Nebojsa Nick Knezevic. Management of concomitant metabolic encephalopathy and meningioma with vasogenic edema and impending herniation. 08-Feb-2018;9:25. Available from: http://surgicalneurologyint.com/surgicalint-articles/management-of-concomitant-metabolic-encephalopathy-and-meningioma-with-vasogenic-edema-and-impending-herniation/
Abstract
Background:Altered mental status describes impaired mental functioning ranging from confusion to coma and indicates an illness, either metabolic or structural in nature. Metabolic causes include hypothyroidism, hyperuremia, hypo/hyperglycemia, hypo/hypernatremia, and encephalopathy. The structural causes include tumors, brain hemorrhage, infection, and stroke. To our knowledge, this is the first case in which a patient presented with altered mental status from both metabolic (myxedema coma) and structural diseases (frontal meningioma) with vasogenic edema and midline shift.
Case Description:A 55-year-old female presented with progressive coma. The clinical features included bradycardia and hypothermia. The imaging demonstrated a large frontal meningioma with a significant midline shift with laboratory findings suggestive of severe hypothyroidism and myxedema coma. Hypothyroidism was treated aggressively with intravenous T3 and T4 with close neurosurgical observation. Osmodiuretics and steroids were administered as temporizing agents prior to craniotomy. Craniotomy was successfully undertaken after using these appropriate pre-emptive measures.
Conclusions:Management of concomitant metabolic encephalopathy and meningioma with vasogenic edema and impending herniation can be challenging. Correction of the encephalopathy is crucial to minimize perioperative morbidity and mortality. Awareness of metabolic causes of acute decompensation is critical for perioperative management, so a high index of clinical suspicion can make an important timely diagnosis for treatment initiation. Severely hypothyroid patients are sensitive to anesthetic agents and are at a high risk for perioperative complications. Prompt treatment prior to surgical intervention can help minimize perioperative complications.
Keywords: Altered mental status, hypothyroidism, meningioma, myxedema coma, neoplasm
INTRODUCTION
Altered mental status is a general term used to describe various disorders of mental functioning that can range from slight confusion to coma. A high index of clinical suspicion is required for timely diagnosis and treatment. The causes of altered mental status can be divided into metabolic and structural diseases. Metabolic causes include drugs and toxins, infections, hypo/hyperglycemia, electrolyte abnormalities, uremia, hepatic encephalopathy, hypoxia, hypertensive encephalopathy, and hypo/hyperthyroidism.[
Mental status changes with apathy, and inattention may result from structural disorders of the brain. Meningioma is the most common primary brain tumor in adults, accounting for 35–40% of symptomatic primary brain tumors.[
Metabolic causes of acute altered mental status must also be ruled out and are common among the elderly with complex underlying medical conditions. Acute metabolic encephalopathy is a condition of global cerebral dysfunction in the absence of primary structural brain disease. Examples include hypertensive, toxic, hepatic, hypoxic ischemic, and Hashimoto's encephalopathy (myxedema coma). Myxedema coma, a rare cause of metabolic encephalopathy, is defined as a severe form of untreated hypothyroidism leading to decreased mental status, bradycardia, hypothermia, hypercapnia, hypotension, hypoglycemia, and hypoventilation.[
The following case describes an acute onset of altered mental status secondary to undiagnosed severe hypothyroidism that led to myxedema coma with a concomitant large frontal brain meningioma with significant vasogenic edema and a midline shift. This case highlights the medical and surgical obstacles and decision-making process involved in the successful perioperative treatment of severe undiagnosed metabolic encephalopathy.
CASE DESCRIPTION
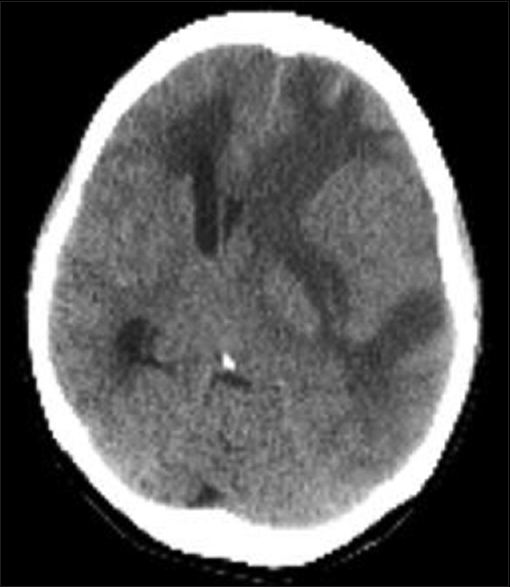
A 55-year old female presented with altered mental status, lethargy, incontinence, and an unsteady gait. Past medical history was significant for Hashimoto's thyroiditis, lung carcinoma treated with chemotherapy and radiation therapy followed by lobectomy, and rheumatoid arthritis. Vital signs revealed a blood pressure of 116/76 mmHg, heart rate 45 bpm, respiratory rate of 10/min, temperature of 35.3°C, and SaO2 98%. She was alert and oriented to person but slow to respond and would not follow commands. Neurologic examination demonstrated a right facial droop, aphasia, right-sided neglect, and a right-sided pronator drift. Laboratory findings were significant for an elevated TSH (151 mcunit/mL) and a decreased free T4 (0.6 ng/dL). Brain computed tomography (CT) revealed a 4.0 × 3.1 × 3.3 cm AP/TR/CC left frontal temporal mass, with significant surrounding vasogenic edema, associated with mass effect/near-complete effacement of the left lateral ventricle and rightward midline shift of approximately 1 cm [
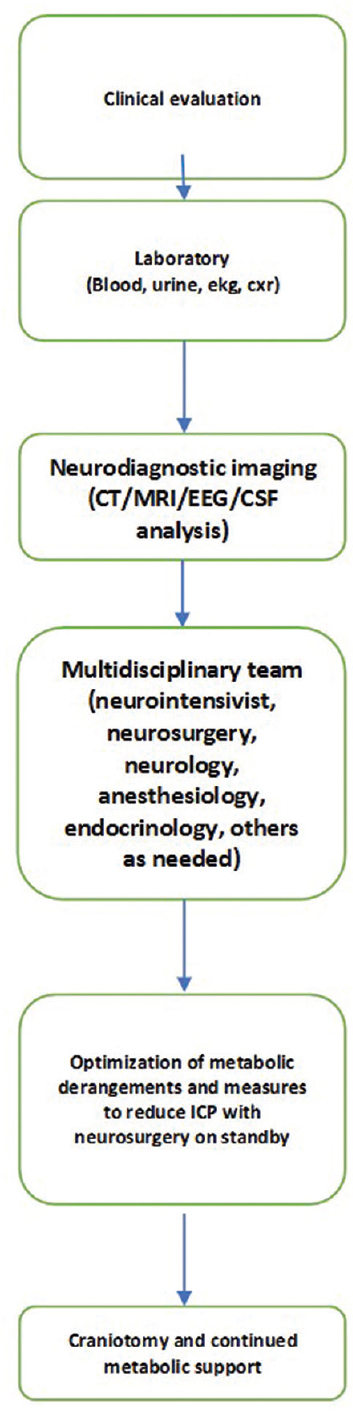
Shortly thereafter, the patient became obtunded with worsening bradycardia (HR 40), bradypnea, and became comatose. A multidisciplinary team involving anesthesia, intensive care, endocrinology, and neurosurgery was called to evaluate the patient. The decision was made for aggressive treatment of the severe hypothyroidism with administration of intravenous T3 and T4 while using osmodiuretics and steroids as temporizing agents. Shortly thereafter, the patient returned to her baseline mental status. Neurosurgery was on standby with close neurological observation and preparedness for surgical intervention should deterioration have occurred while conservative medical management was continued. After medical optimization and resolution of altered mental status, the patient underwent frontotemporal craniotomy and tumor resection. Endotracheal intubation was uneventful, and general anesthesia was maintained with a balanced concentration of intravenous remifentanil and propofol with sevoflourane titrated to <0.5 MAC. The tumor was isolated in the Sylvian fissure, and given the location along the dominant frontal lobe and temporal lobe, decision was made to perform a subcapsular resection. Using a microsurgical technique, the tumor was aggressively resected and the integrity of all the pial surfaces and the arachnoid/capsule was maintained. The surgical procedure and general anesthesia were well tolerated and no complications were noted. The patient was awakened uneventfully after extubation in the surgical intensive care unit 4 hours postoperatively.
DISCUSSION
The case presents two major clinical causes of altered mental status in an otherwise healthy adult patient. Neurosurgeons are familiar with primary conditions in which the brain tumor causes severe hypothyroidism secondary to disruption of the hypothalamic-pituitary-adrenal (HPA) axis (secondary or tertiary hypothyroidism). Our patient did not have a pituitary neoplasm but rather had two separate conditions unrelated to one another, metabolic encephalopathy, and an intracranial neoplasm, which posed an immediate threat to the patient.
Metabolic causes of altered mental status
Metabolic causes of altered mental status include drugs and toxins, infections, hypo/hyperglycemia, electrolyte abnormalities, uremia, hepatic encephalopathy, hypertensive encephalopathy, metabolic encephalopathy, hypoxia, and hypo/hyperthyroidism. Myxedema coma is a rare cause of metabolic encephalopathy and is a life-threatening form of untreated hypothyroidism with metabolic decompensation and mortality that reaches near 100%, if left untreated. Even with optimal therapy, the mortality rate can reach up to 30–60%.[
Structural brain lesions of altered mental status
Structural changes of the brain should also be considered in patients with acute mental status changes. Some examples include brain hemorrhage, brain tumors, traumatic brain injury, hydrocephalus, meningitis, and encephalitis. Meningioma is the most common adult primary brain neoplasm, accounting for 40% of all adult brain tumors. It causes chronic changes, and although symptoms are based on the location, size, and growth rate of the tumor, meningiomas are typically very slow growing and asymptomatic. The most common manifestations are focal findings such as headache, seizure, visual field deficits, loss of hearing or smell, extremity weakness, and mental status changes, all of which can result from large subfrontal or sphenoid ridge meningioma. Management of smaller, benign, and asymptomatic meningiomas typically includes close monitoring of symptoms and serial MRI studies. Treatment of atypical and malignant meningiomas can be treated with surgical resection or radiosurgery. If discovered earlier in a young patient, surgical resection is less complicated and usually provides cure if radical resection is performed. Radiosurgery may follow if the residual tumor was left behind and may be performed for isolated tumors in the deeper regions of the brain or those that are closer to delicate structures. However, if the tumor continues to grow to cause significant mass effect and vasogenic edema, it can produce not only altered mental status but also significant neurologic deterioration with higher morbidity and mortality. Certain preoperative measures should be taken, which include treating the cerebral edema and elevated intracranial pressure with corticosteroids, mannitol, and furosemide. Surgical morbidity ranges between 2% and 30%, and is dependent on a variety of factors such as size and location of tumor, patient age, and other metabolic comorbidities.
The current case illustrates severe metabolic encephalopathy with concomitant intracranial neoplasm with a significant midline shift, both of which are rare causes of acute decompensation. Differentiating between the causes of altered mental status was a challenging task, and despite the possibility of the meningioma-induced mass effect and herniation as a possible cause of altered mental status, the thyroid stimulating hormone and free thyroxine levels in combination with the signs and symptoms of the patient's presentation (hypothermia, bradycardia, bradypnea, altered mental status) were sufficient to make the diagnosis of myxedema coma.
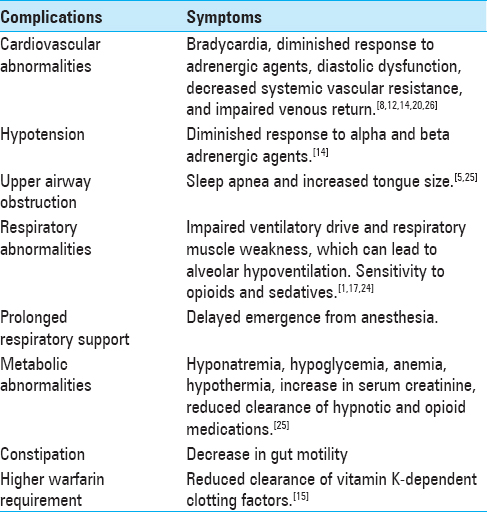
The multidisciplinary approach in diagnosing and treating this patient's altered mental status proved critical in avoiding significant perioperative morbidity and mortality associated with myxedema encephalopathy. Under the stress of surgery and general anesthesia, patients with untreated myxedema coma can exhibit significant myocardial depression and diastolic dysfunction, depressed respiratory drive and diaphragmatic weakness resulting in difficulty weaning from ventilator, decreased venous return and systemic vascular resistance, diminished response to alpha- and beta-adrenergic agents, and extreme sensitivity to opioids and sedatives [
Table 1
Risks and complications of general anesthesia for patients with severe hypothyroidism[
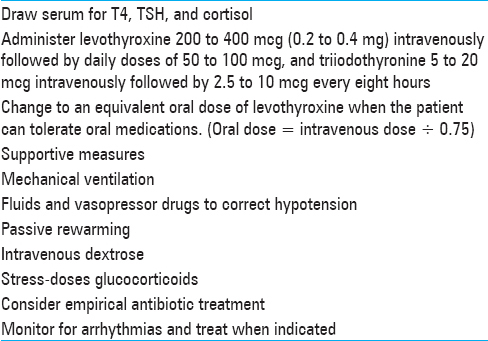
Table 2
Treatment guidelines for severe hypothyroidism[
If emergency surgery must be performed without the luxury of preoperatively treating myxedema coma, certain measures should be taken to decrease the risk of complications. Avoidance of benzodiazepines and opioids should be considered due to increased sensitivity and risk of respiratory failure. Induction can be achieved with ketamine, offering sympathetic stimulation in a state of hypotension, low cardiac output, intravascular volume depletion, and blunted baroreceptor reflexes. Ketamine use in traumatic brain injury was once considered contraindicated when associated with an elevation of ICP, with recent studies now demonstrating level 2 B grade C evidence showing that ketamine does not appreciably increase ICP.[
Medical management in this case included intravenous thyroid hormone therapy, osmodiuretics, and steroids. Steroids are recommended for reduction of intracranial pressure for all patients with peritumoral edema as improvement in neurological function can be seen within hours.[
When assessing a patient for altered mental status, metabolic causes of delirium must always be ruled out. If surgery must be performed in a patient with hypothyroidism and there is concern about existing or precipitating myxedema coma, treatment with osmodiuretics and steroids have proven to be useful adjuvants to control critical elevations of intracranial pressure while waiting for therapeutic levels of both T3 and T4 to maximize perioperative tolerance under anesthesia and surgery.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abbott TR. Anaesthesia in untreated myxoedema. Report of two cases. Br J Anaesth. 1967. 39: 510-
2. Akhtar S, Beynon J, Kearney T. Predictors of outcome in myxoedema coma. Crit Care. 2008. 12: 111-
3. Furman WRRobertson ACRetrieved on 2017 Sep 20. Available from https://www.uptodate.com/contents/anesthesia-for-patients-with-thyroid-diseasesource=search_result&search=nesthesia%20for%20patients%20with%20thyroid&selectedTitle=1~150.
4. Arlot S, Debussche X, Lalau JD, Mesmacque A, Tolani M, Quichard J. Myxodema coma: Response of thyroid hormones with oral and intravenous high-dose L-thyroxine treatment. Intensive Care Med. 1991. 17: 16-8
5. Bahammam SA, Jammah AA, Sharif MM. Prevalence of thyroid disease in patients with obstructive sleep apnea. Respir Med. 2011. 105: 1755-
6. Bailes BK. Hypothyroidism in elderly patients. AORN J. 1999. 69: 1026-30
7. Bennett-Guerrero E, Kramer DC, Schwinn DA. Effect of chronic and acute thyroid hormone reduction on perioperative outcome. Anesth Analg. 1997. 85: 30-
8. Biondi B. Cardiovascular effects of mild hypothyroidism. Thyroid. 2007. 17: 625-
9. Braverman LE, Ingbar SH, Utiger RD, Werner SC.editors. The thyroid: A fundamental and clinical text. Philadelphia: Lipincott Williams and Wilkins; 2000. p.
10. Weinberg AD, Brennan MD, Gorman CA, Marsh HM, O'Fallon WM. Outcome of anesthesia and surgery in hypothyroid patients. Arch Intern Med. 1983. 143: 893-
11. Bryan young, Francis , Joseph “Diagnosis of delirium and confusional states” UpToDate. p.
12. Taddei S, Caraccio N, Virdis A, Dardano A, Versari D, Ghoadoni L. Impaired endothelium-dependent vasodilatation in subclinical hypothyroidism: Beneficial effect of levothyroxine therapy. J Clin Endocrinol Metab. 2003. 88: 3731-
13. David PJ, Davis FB. Hypothyroidism in the elderly. Compr Ther. 1984. 10: 17-23
14. Deegan RJ, Furman WR. Cardiovascular manifestations of endocrine dysfunction. J Cardiothorac Vasc Anesth. 2011. 25: 705-
15. Douglas , Ross , Manzullo , Ellen “Nonthyroid surgery in the patient with thyroid disease” UpToDate. p.
16. Dutta P, Bhansali A, Masoodi SR, Bhadada S, Sharma N, Rajput R. Predictors of outcome in myxoedema coma: A study from a tertiary care centre. Crit Care. 2008. 12: R1-
17. Hackman L, Kim JM. Anesthesia for untreated hypothyroidism: Report of three cases. Anesth Analg. 1977. 56: 299-
18. Hylander B, Rosenqvist U. Treatment of myxoedema coma--factors associated with fatal outcome. Acta Endocrinol (Copenh). 1985. 108: 65-
19. Jordan RM. Myxedema coma: Pathophysiology, therapy, and factors affecting prognosis. Med Clin North Am. 1995. 79: 185-94
20. Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001. 344: 501-
21. LoPresti JS, Nicoloff JT. Myxedema coma. A form of decompensated hypothyroidism. Endocrinol Metab Clin North Am. 1993. 22: 279-90
22. Olsen C. Myxedema Coma In The Elderly. J Am Fam Med. 1995. 8: 376-83
23. Ross DRetrieved on 2017 Sep 20. Available from: https://www.uptodate.com/contents/myxedema-coma?source=search_result&search=Myxedema%20coma&selectedTitle=1~25.
24. Smallridge RC. Metabolic and anatomic thyroid emergencies: A review. Crit Care Med. 1992. 20: 276-
25. Stathatos N, Wartofsky L. Perioperative management of patients with hypothyroidism. Endocrinol Metab Clin North Am. 2003. 32: 503-
26. Virtanen VK, Saha HH, Groundstroem KW, Salmi J, Pasternack AI. Thyroid hormone substitution therapy rapidly enhances left-ventricular diastolic function in hypothyroid patients. Cardiology. 2001. 96: 59-
27. Michaud DSchiff DBatchelor TRetrieved on 2017 Sep 20. Available from. https://www.uptodate.com/contents/incidence-of-primary-brain-tumors?source=search_result&search=Incidence%20of%20primary%20brain%20tumors&selectedTitle=1~150.
28. Last accessed on 2017 Sep 20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2945461.
29. Last accessed on 2017 Sep 20. https://www.uptodate.com/contents/diagnosis-of-and-screening-for-hypothyroidism-in-nonpregnant-adults?source=search_result&search=hypothyroidism&selectedTitle=1~150#H2.
30. Last accessed on 2017 Sep 20. https://www.ncbi.nlm.nih.gov/pubmed/24515638.
31. Last accessed on 2017 Sep 20. https://www.uptodate.com/contents/management-of-vasogenic-edema-inpatients-with-primary-and-metastatic-brain-tumors.