- Department of Anesthesiology, University of Chicago at Illinois, Advocate Illinois Masonic Medical Center, Chicago,
- Department of Neurosurgery, Ghaly Neurosurgical Associates, Aurora, Illinois, United States.
Correspondence Address:
Ramsis Ghaly
Department of Anesthesiology, University of Chicago at Illinois, Advocate Illinois Masonic Medical Center, Chicago,
DOI:10.25259/SNI_318_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ramsis Ghaly1,2, Armen Haroutunian1, Gevorg Grigoryan1, Jessica A. Patricoski2, Kenneth D. Candido1, Nebojsa Nick Knezevic1. Management of CRPS secondary to preganglionic C8 nerve root avulsion: A case report and literature review. 29-Aug-2020;11:262
How to cite this URL: Ramsis Ghaly1,2, Armen Haroutunian1, Gevorg Grigoryan1, Jessica A. Patricoski2, Kenneth D. Candido1, Nebojsa Nick Knezevic1. Management of CRPS secondary to preganglionic C8 nerve root avulsion: A case report and literature review. 29-Aug-2020;11:262. Available from: https://surgicalneurologyint.com/surgicalint-articles/10232/
Abstract
Background: Cervical nerve root avulsion is a well-documented result of high-velocity motor vehicle accidents (MVAs). In up to 21% of cases, preganglionic cervical root avulsion can result in a complex regional pain syndrome (CRPS) impacting the quality of life for patients already impaired by motor, sensory, and autonomic dysfunction. The optimal treatment strategies include repeated stellate ganglion blocks (SBGs).
Case Description: A 43-year-old male sustained a high-velocity MVA resulting in the left C8 nerve root avulsion. This resulted in weakness in the C8 distribution, tactile allodynia, and dysesthesias. The magnetic resonance imaging demonstrated an abnormal signal ventral to the C8–T1 level. As the patient was not considered a candidate for surgical intervention secondary to the attendant brachial plexus injury, a C7–C8 epidural steroid injection was performed; this did not provide improvement. Before placing a spinal cord stimulator, the patient underwent a series of six ultrasound-guided SBGs performed 2 weeks apart; there was 75% improvement in pain and strength. Six years later, the patient continues to do well while receiving SBGs 4 times a year.
Conclusion: A preganglionic cervical nerve root avulsion should not be a contraindication for a stellate ganglion block in a patient with established CRPS.
Keywords: Avulsion, Cervical, Complex regional pain syndrome, Nerve root, Preganglionic, Stellate ganglion block
INTRODUCTION
Neuropathic pain from preganglionic avulsion injuries (i.e., located proximal to the dorsal root ganglion [DRG]) is difficult to treat as nearly 50% develop chronic pain.[
CASE PRESENTATION
A 43-year-old male presented for more than 2 years of left-sided C8 root symptoms/ signs following an avulsion injury sustained due to a motor vehicle accident (MVA). He developed a CRPS type II lesion, treated with venlafaxine, lisdexamfetamine, quetiapine, cyclobenzaprine, and lidocaine patches, multiple cervical interlaminar epidural injections, and physical therapy; none of which resulted in significant improvement. On physical examination, he had left upper extremity 3/5–4/5 motor deficits in the C6–C8 distributions, intolerable C8 dysesthesias, and tactile allodynia. He also had a 2.3° reduced temperature regionally in the left arm compared to the right arm.
Magnetic resonance imaging (MRI) and EMG findings
The MRI demonstrated abnormal signals ventral to the C8–T1 level consistent with an avulsed C8 nerve root. Electrodiagnostic tests including electromyography revealed sensory and motor conduction abnormalities for pre- and postganglionic involvement of the C8 distribution.
Treatment with SBGs
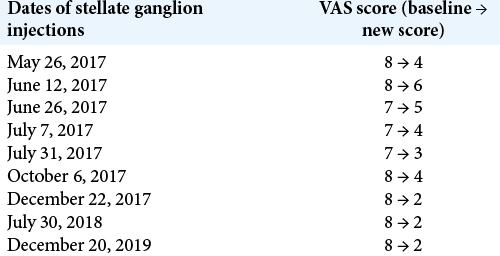
The patient met the Budapest Clinical Diagnostic Criteria for CRPS type II. The patient received an initial left-sided, ultrasound-guided stellate ganglion block 30 months after the avulsion injury; it resulted in 50% pain relief. He underwent a series of five additional SGBs performed 2–3 weeks apart, ultimately experiencing 75% improvement in pain and strength [
DISCUSSION
A high force traction brachial plexus injury can result in avulsion, leading to torn nerve roots and axons. These most commonly occur at the C8 and T1 levels. At present, there is no universally accepted standard of care for avulsion injuries.[
Diagnostic studies confirming nerve root avulsion injuries
Although MRI is the gold standard for the evaluation of nerve root avulsion injuries, CT myelography may also be very helpful.[
Treatment options
Treatment of preganglionic cervical nerve root avulsion includes conservative versus surgical approaches. Preganglionic avulsion injuries can be surgically treated by neurotization, nerve transfers, traditional spinal (dorsal) column stimulation (SCS: 50% success), peripheral nerve stimulation, DREZ lesions, and in primary motor cortex stimulation (55% success rate) (MCS).[
Interventional strategies
In patients with coexisting CRPS, interscalene brachial plexus and/or SBGs can be therapeutic.[
Pharmacologic therapy
Preganglionic avulsion injury is difficult to treat with strictly pharmacological therapy. First tier medications include tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs).[
CONCLUSION
Conventionally, SBGs have been utilized to treat CRPS type I (formerly called reflex sympathetic dystrophy) and CRPS type II syndromes following nerve root avulsion injuries. As a rescue technique, these have proven safe and effective, in some cases avoiding the need for surgery (e.g., nerve transfer and/or cervical spinal cord stimulation).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ackerman WE, Zhang JM. Efficacy of stellate ganglion blockade for the management of Type 1 complex regional pain syndrome. South Med J. 2006. 99: 1084-8
2. Chien GC, Candido KD, Saeed K, Knezevic NN. Cervical spinal cord stimulation treatment of deafferentation pain from brachial plexus avulsion injury complicated by complex regional pain syndrome. A A Case Rep 2014. ;. 3: 29-34
3. Datta R, Agrawal J, Sharma A, Rathore VS, Datta S. A study of the efficacy of stellate ganglion blocks in complex regional pain syndromes of the upper body. J Anaesthesiol Clin Pharmacol. 2017. 33: 534-40
4. Lovaglio AC, Socolovsky M, Di Masi G, Bonilla G. Treatment of neuropathic pain after peripheral nerve and brachial plexus traumatic injury. Neurol India. 2019. 67: S32-7
5. Subedi A, Chaudakshetrin P, Chotisukarat H, Mandee S. Effect of co-morbid conditions on persistent neuropathic pain after brachial plexus injury in adult patients. J Clin Neurol. 2016. 12: 489-94
6. Toshniwal G, Sunder R, Thomas R, Dureja GP. Management of complex regional pain syndrome Type I in upper extremity-evaluation of continuous stellate ganglion block and continuous infraclavicular brachial plexus block: A pilot study. Pain Med. 2012. 13: 96-106
7. Tu YK, Tsai YJ, Chang CH, Su FC, Hsiao CK, Tan JS. Surgical treatment for total root avulsion type brachial plexus injuries by neurotization: A prospective comparison study between total and hemicontralateral C7 nerve root transfer. Microsurgery. 2014. 34: 91-101