- Department of Neurosurgery, Riverside University Health System, Riverside, California, United States.
- Department of Clinical Imaging Research, Carle Illinois College of Medicine Beckman Institute of Advanced Science and Technology, Urbana, Illinois, United States.
- Department of Mechanical Engineering, University of Kansas, Lawrence, Kansas,
- Department of Neurosurgery, Carle Neuroscience Institute, Urbana, Illinois, United States.
Correspondence Address:
Samir Kashyap, Department of Neurosurgery, Riverside University Health System, Riverside, California, United States.
DOI:10.25259/SNI_94_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Samir Kashyap1, Andrew G. Webb2, Elizabeth A. Friis3, Paul M. Arnold4. Management of single-level thoracic disc herniation through a modified transfacet approach: A review of 86 patients. 06-Jul-2021;12:338
How to cite this URL: Samir Kashyap1, Andrew G. Webb2, Elizabeth A. Friis3, Paul M. Arnold4. Management of single-level thoracic disc herniation through a modified transfacet approach: A review of 86 patients. 06-Jul-2021;12:338. Available from: https://surgicalneurologyint.com/surgicalint-articles/10940/
Abstract
Background: Symptomatic thoracic disc herniation (TDH) is rare and does not typically resolve with conservative management. Traditional surgical management is the transthoracic approach; however, this approach can carry significant risk. Posterolateral approaches are less invasive, but no single approach has proven to be more effective than the other results are often dependent on surgeon experience with a particular approach, as well as the location and characteristics of the disc herniation.
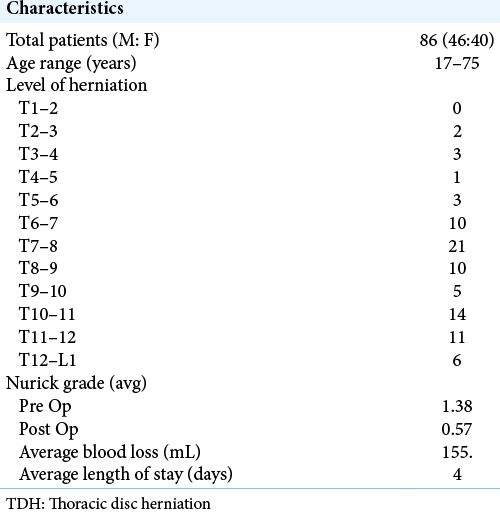
Methods: This was retrospective review of a prospectively collected database. Eighty-six patients with TDH treated surgically through the modified transfacet approach were reviewed and evaluated for pain improvement, Nurick grade, and neurological symptoms. Patients were followed for 12 months postoperatively; estimated blood loss, length of hospital stay, hospital course, and postoperative complications were also assessed.
Results: All attempts at disc resection were successful. Most patients reported improvement in pain, sensory involvement, and strength. Seventy-nine patients had complete resolution of their symptoms while four patients had unchanged symptoms. Three patients experienced mild neurologic worsening postoperatively, but this resolved back to baseline. One patient experienced myelopathy during the postoperative period that resolved with steroid administration. The procedure was well tolerated with minimal complications.
Conclusion: TDH can be managed surgically through a variety of approaches. The selection of approach is dependent on surgeon experience with an approach, the patient’s health, and the location and type of disc. The transfacet approach is safe and efficacious.
Keywords: Pedicle sparing, Thoracic disc herniation, Transfacet
INTRODUCTION
Thoracic disc herniation (TDH), while relatively rare in comparison to cervical and lumbar disc herniation, is not as uncommon as once thought. Advanced imaging techniques have revealed a prevalence of 11–37% in TDH patients who are asymptomatic and an incidence of 15.2% in postmortem patients.[
While the transthoracic approach is traditionally viewed, as the gold standard for surgical treatment of TDH, transpedicular, transdural, transfacet pedicle-sparing, and minimally invasive posterolateral approaches are gaining popularity, due to increased evidence of reductions in length of stay and shorter recovery time for patients without sacrificing neurological outcome.[
MATERIALS AND METHODS
Patient population
A retrospective review was conducted for patients with symptomatic single level TDHs who underwent surgical treatment at single institution between August 1993 and January 2019. All patients presented with symptoms of either radiculopathy or myelopathy. The patients’ preoperative clinic notes, operative reports, and postoperative follow-up clinic notes up to 12 months postoperation were also reviewed. Diagnosis was confirmed by MRI, CT myelogram, or both. Patients with centrally located or calcified disks were not treated via this approach.
Surgical technique
The surgical procedure was previously described.[
RESULTS
All attempts at resection of 86 single-level herniated discs were successful in (46 males and 40 females), ranging from 17 to 75 years of age. Pain relief was the preoperative symptom most consistently improved, with 82% of patients achieving good results (P < 0.005). About 57% of patients demonstrated improvement in their ability to ambulate, and 51% had postoperative sensory improvement. The most common level of herniation was T7-8[
DISCUSSION
Symptomatic TDHs are as rare as they are controversial in their management, ranging from conservative medical management (e.g., epidural steroid injections, physical therapy, and oral medications) to surgical management.[
In asymptomatic patients, the herniation will not spontaneously regress, but it will typically remain stable.[
Surgical management of TDH has remained controversial. The only approach that has effectively been abandoned is laminectomy due to its increased morbidity and mortality and lack of efficacy.[
Recent studies indicate that posterolateral approaches such as the transfacet pedicle-sparing approach result in shorter length of stay and decreased complications while still achieving similar outcomes.[
Minimally-invasive approaches are rapidly gaining popularity due to their ability to minimize blood loss, bone, and soft-tissue resection, and eliminate the need for fusion.[
CONCLUSION
Eighty-six patients with single-level TDHs were surgically managed through a modified transfacet approach. All patients presented with complaints of myelopathy, radiculopathy, or intractable back pain. About 82% of patients demonstrated postoperative pain reduction, and 57% of patients showed improved ability to ambulate. Sensory loss was less consistently improved with 51% of patients showing improvement. Complications occurred at a rate of <4.5%. Surgical management of herniated thoracic discs can be achieved through a modified transfacet approach in a safe and efficacious manner.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arnold PM, Bryniarski M. Emergency thoracic diskectomy for the acute onset of paraplegia: Report of two cases. J Spinal Cord Med. 2004. 27: 481-3
2. Arnold PM, Johnson PL, Anderson KK. Surgical management of multiple thoracic disc herniations via a transfacet approach: A report of 15 cases. J Neurosurg Spine. 2011. 15: 76-81
3. Baranto A, Börjesson M, Danielsson B, Hellström M, Swärd L. Acute chest pain in a top soccer player due to thoracic disc herniation. Spine (Phila Pa 1976). 2009. 34: E359-62
4. Börm W, Bäzner U, König RW, Kretschmer T, Antoniadis G, Kandenwein J. Surgical treatment of thoracic disc herniations via tailored posterior approaches. Eur Spine J. 2011. 20: 1684-90
5. Bransford R, Zhang F, Bellabarba C, Konodi M, Chapman JR. Early experience treating thoracic disc herniations using a modified transfacet pedicle-sparing decompression and fusion. J Neurosurg Spine. 2010. 12: 221-31
6. Bransford RJ, Zhang F, Bellabarba C, Lee MJ. Treating thoracic-disc herniations: Do we always have to go anteriorly?. Evid Based Spine Care J. 2010. 1: 21-8
7. Brotis AG, Tasiou A, Paterakis K, Tzerefos C, Fountas KN. Complications associated with surgery for thoracic disc herniation: A systematic review and network meta-analysis. World Neurosurg. 2019. 132: 334-42
8. Carr DA, Volkov AA, Rhoiney DL, Setty P, Barrett RJ, Claybrooks R. Management of thoracic disc herniations via posterior unilateral modified transfacet pedicle-sparing decompression with segmental instrumentation and interbody fusion. Global Spine J. 2017. 7: 506-13
9. Coppes MH, Bakker NA, Metzemaekers JD, Groen RJ. Posterior transdural discectomy: A new approach for the removal of a central thoracic disc herniation. Eur Spine J. 2012. 21: 623-8
10. Cornips EM, Janssen ML, Beuls EA. Thoracic disc herniation and acute myelopathy: Clinical presentation, neuroimaging findings, surgical considerations, and outcome. J Neurosurg Spine. 2011. 14: 520-8
11. Court C, Mansour E, Bouthors C. Thoracic disc herniation: Surgical treatment. Orthop Traumatol Surg Res. 2018. 104: S31-40
12. Lara FJ, Berges AF, Quesada JQ, Ramiro JA, Toledo RB, Muñoz HO. Thoracic disk herniation, a not infrequent cause of chronic abdominal pain. Int Surg. 2012. 97: 27-33
13. Mannen EM, Friis EA, Sis HL, Wong BM, Cadel ES, Anderson DE. The rib cage stiffens the thoracic spine in a cadaveric model with body weight load under dynamic moments. J Mech Behav Biomed Mater. 2018. 84: 258-64
14. Moon SJ, Lee JK, Jang JW, Hur H, Lee JH, Kim SH. The transdural approach for thoracic disc herniations: A technical note. Eur Spine J. 2010. 19: 1206-11
15. Nacar OA, Ulu MO, Pekmezci M, Deviren V. Surgical treatment of thoracic disc disease via minimally invasive lateral transthoracic trans/retropleural approach: Analysis of 33 patients. Neurosurg Rev. 2013. 36: 455-65
16. Nakhla J, Bhashyam N, De la Garza Ramos R, Nasser R, Kinon MD, Yassari R. Minimally invasive transpedicular approach for the treatment of central calcified thoracic disc disease: A technical note. Eur Spine J. 2018. 27: 1575-85
17. Nannapaneni R, Marks SM. Posterolateral thoracic disc disease: Clinical presentation and surgical experience with a modified approach. Br J Neurosurg. 2004. 18: 467-70
18. Ohnishi K, Miyamoto K, Kanamori Y, Kodama H, Hosoe H, Shimizu K. Anterior decompression and fusion for multiple thoracic disc herniation. J Bone Joint Surg Br. 2005. 87: 356-60
19. Paolini S, Tola S, Missori P, Esposito V, Cantore G. Endoscope-assisted resection of calcified thoracic disc herniations. Eur Spine J. 2016. 25: 200-6
20. Piccirilli M, Lapadula G, Caporlingua F, Martini S, Santoro A. Spontaneous regression of a thoracic calcified disc herniation in a young female: A case report and literature review. Clin Neurol Neurosurg. 2012. 114: 779-81
21. Rohde RS, Kang JD. Thoracic disc herniation presenting with chronic nausea and abdominal pain. A case report. J Bone Joint Surg Am. 2004. 86: 379-81
22. Sheikh H, Samartzis D, Perez-Cruet MJ. Techniques for the operative management of thoracic disc herniation: Minimally invasive thoracic microdiscectomy. Orthop Clin North Am. 2007. 38: 351-61
23. Shirzadi A, Drazin D, Jeswani S, Lovely L, Liu J. Atypical presentation of thoracic disc herniation: Case series and review of the literature. Case Rep Orthop. 2013. 2013: 621476
24. Sivakumaran R, Uschold TD, Brown MT, Patel NR. Transfacet and transpedicular posterior approaches to thoracic disc herniations: Consecutive case series of 24 patients. World Neurosurg. 2018. 120: e921-31
25. Stillerman CB, Chen TC, Couldwell WT, Zhang W, Weiss MH. Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. J Neurosurg. 1998. 88: 623-33
26. Uribe JS, Smith WD, Pimenta L, Härtl R, Dakwar E, Modhia UM. Minimally invasive lateral approach for symptomatic thoracic disc herniation: Initial multicenter clinical experience. J Neurosurg Spine. 2012. 16: 264-79
27. Wagner R, Telfeian AE, Iprenburg M, Krzok G, Gokaslan Z, Choi DB. Transforaminal endoscopic foraminoplasty and discectomy for the treatment of a thoracic disc herniation. World Neurosurg. 2016. 90: 194-8
28. Wessell A, Mushlin H, Fleming C, Lewis E, Sansur C. Thoracic discectomy through a unilateral transpedicular or costotransversectomy approach with intraoperative ultrasound guidance. Oper Neurosurg (Hagerstown). 2019. 17: 332-7
29. Wood KB, Blair JM, Aepple DM, Schendel MJ, Garvey TA, Gundry CR. The natural history of asymptomatic thoracic disc herniations. Spine (Phila Pa 1976). 1997. 22: 525-9
30. Xiong Y, Lachmann E, Marini S, Nagler W. Thoracic disk herniation presenting as abdominal and pelvic pain: A case report. Arch Phys Med Rehabil. 2001. 82: 1142-4
31. Yang X, Liu X, Zheng Y. Surgical treatment of thoracic disc herniations using a modified transfacet approach. Indian J Orthop. 2014. 48: 158-62