- Department of Trauma and Orthopaedics, NHS Tayside, Ninewells Hospital, Dundee, United Kingdom.
- Department of Neurosurgery, NHS Lothian, Royal Infirmary of Edinburgh, Edinburgh, Scotland, United Kingdom.
- Department of Paediatric Neurosurgery, Birmingham Children’s Hospital, Birmingham Women’s and Children’s NHS Foundation Trust, Birmingham, United Kingdom.
- Department of Paediatric Neurosurgery, NHS Lothian, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom.
Correspondence Address:
Himanshu Shekhar, Department of Trauma and Orthopaedics, NHS Tayside, Ninewells Hospital, Dundee, United Kingdom.
DOI:10.25259/SNI_17_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Himanshu Shekhar1, Marco Mancuso-Marcello2, John Emelifeonwu2, Pasquale Gallo3, Drahoslav Sokol4, Jothy Kandasamy4, Chandrasekaran Kaliaperumal4. Management of traumatic atlanto-occipital dislocation in a 10-year-old with noninvasive halo immobilization: A case report. 27-May-2022;13:222
How to cite this URL: Himanshu Shekhar1, Marco Mancuso-Marcello2, John Emelifeonwu2, Pasquale Gallo3, Drahoslav Sokol4, Jothy Kandasamy4, Chandrasekaran Kaliaperumal4. Management of traumatic atlanto-occipital dislocation in a 10-year-old with noninvasive halo immobilization: A case report. 27-May-2022;13:222. Available from: https://surgicalneurologyint.com/surgicalint-articles/11621/
Abstract
Background: Traumatic atlanto-occipital dislocation is an unstable injury of the craniocervical junction. For pediatric patients, surgical arthrodesis of the occipitocervical junction is the recommended management. While having a high success rate for stabilization, the fusion comes with obvious morbidity of limitation in cervical spine flexion, extension, and rotation. An alternative is external immobilization with a conventional halo.
Case Description: We describe the case of a 10-year-old boy who was treated successfully for traumatic AOD with a noninvasive pinless halo. Following initial brain trauma management, we immobilized the craniocervical junction with a pinless halo after reducing the atlanto-occipital dislocation. The pinless halo was kept on at all times for the next 3 months. The craniocervical junction alignment was monitored with weekly cervical spine X-rays and CT craniocervical junction on day 15th, day 30th, and day 70th. A follow-up MRI C-spine 3 months from presentation confirmed resolution of the soft-tissue injury and the pinless halo was removed. Dynamic cervical spine X-rays revealed satisfactory alignment in both flexion and extension views. The patient has been followed up for 2 years postinjury and no issues were identified.
Conclusion: Noninvasive pinless halo is a potential treatment option for traumatic pediatric atlanto-occipital dislocation. This should be considered bearing in mind multiple factors including age and weight of the patient, severity of the atlanto-occipital dislocation (Grade I vs. Grade II and incomplete vs. complete), concomitant skull and scalp injury, and patient’s ability to tolerate the halo. It is vital to emphasize that this necessitates close clinicoradiological monitoring.
Keywords: Atlanto-occipital dislocation, Children, Halo, Trauma
BACKGROUND
Traumatic atlanto-occipital dislocation is an unstable injury of the craniocervical junction. Up to a third of patients with mortality related to cervical spine trauma have atlanto-occipital dislocation. Perhaps, due to the improved survival of trauma victims with modern trauma management, this injury is occasionally seen in survivors with craniocervical spine trauma.
Atlanto-occipital dislocation is commoner in children[
For pediatric patients, surgical arthrodesis of the occipitocervical junction is the recommended management.[
An alternative is external immobilization with a conventional halo. This has been described for patients with a “mild AOD”[
CASE DESCRIPTION
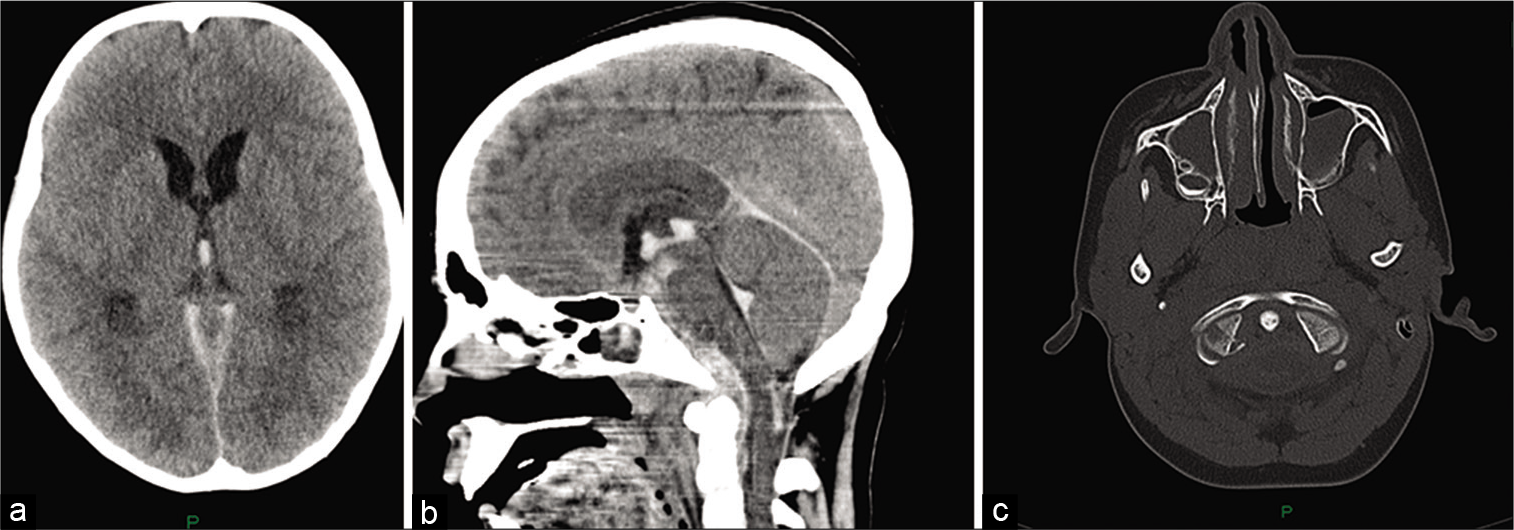
A 10-year-old boy was admitted to our hospital following a collision of his head to the underside of a metal barrier whilst riding at 30 mph on a motorized scooter. He sustained a hyperextension injury of the cervical spine. The patient also had considerable intracranial injuries. He was reported to be orientated and obeying commands at the scene of the accident but by his admission to the emergency department, he was GCS 9 (E2V4M3). He was intubated and ventilated. His injuries were assessed as per the ATLS protocol and his cervical spine was immobilized. IV mannitol was administered for suspected raised intracranial pressure. The initial trauma CT [
Figure 1:
(a) CT brain shows intraventricular hemorrhage and hydrocephalus, (b) sagittal MPR shows the intraventricular hemorrhage and extensive extra-axial hematoma anterior to the brainstem and extending to cervical spine, and (c) CT brain (bone window) shows fracture of the right occipital condyle with medial displacement of fractured fragment.
The patient underwent insertion of a left frontal intracranial pressure monitoring probe and a right frontal ventricular access device. Following his transfer to pediatric ICU, he had external CSF diversion through the ventricular access device and his intracranial pressure remained well controlled. On the 5th day, the sedation was weaned and the patient was extubated.
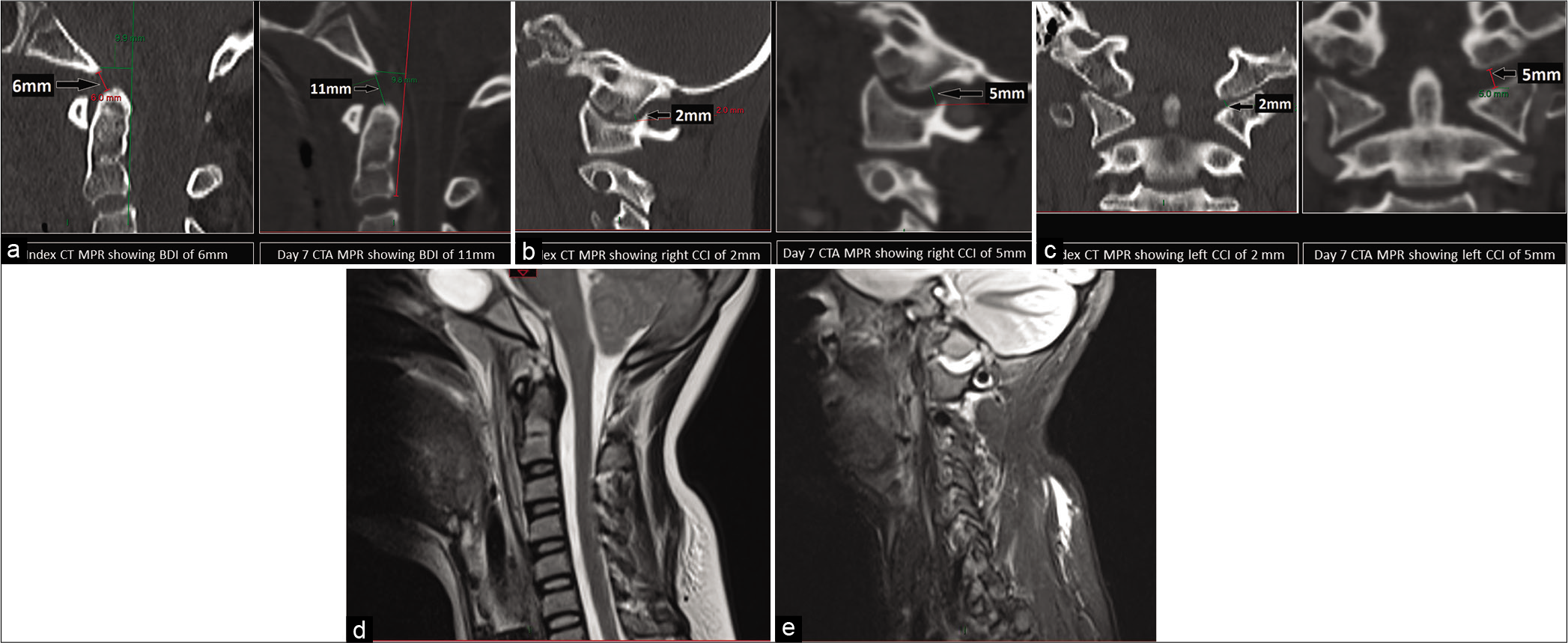
He had CT and MR cerebral angiograms 7 days after presentation to investigate suspected vascular injury and this revealed ligamentous injury at the craniocervical junction [
Figure 2:
CT MPR showing increase in the basion-dens interval from 6 mm to 11 mm between the index CT and the D7 CTA, (b) CT MPR showing increase in the right C0C1 interval from 2 mm to 5 mm between the index CT and the D7 CTA, (c) CT MPR showing increase in the left C0C1 interval from 2 mm to 5 mm between the index CT and the D7 CTA, (d) MR cervical spine (midsagittal T2) shows apical ligament injury and intact tectorial membrane elevated by retroclival hematoma, and (e) MR cervical spine (parasagittal T2) shows C0C1 joint injury with hemorrhage.
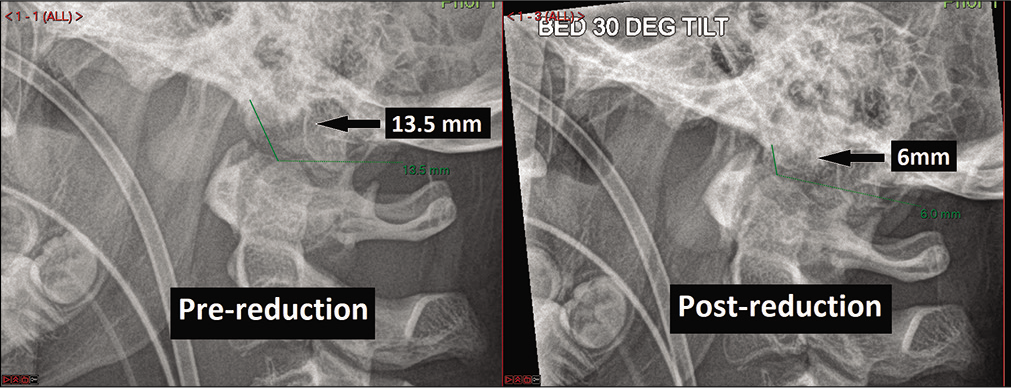
Under general anesthesia, the dislocation was reduced with gravity (30° head end elevation) and gentle compression with the pinless halo, under fluoroscopic guidance. We used the “Lerman” noninvasive halo for this patient.
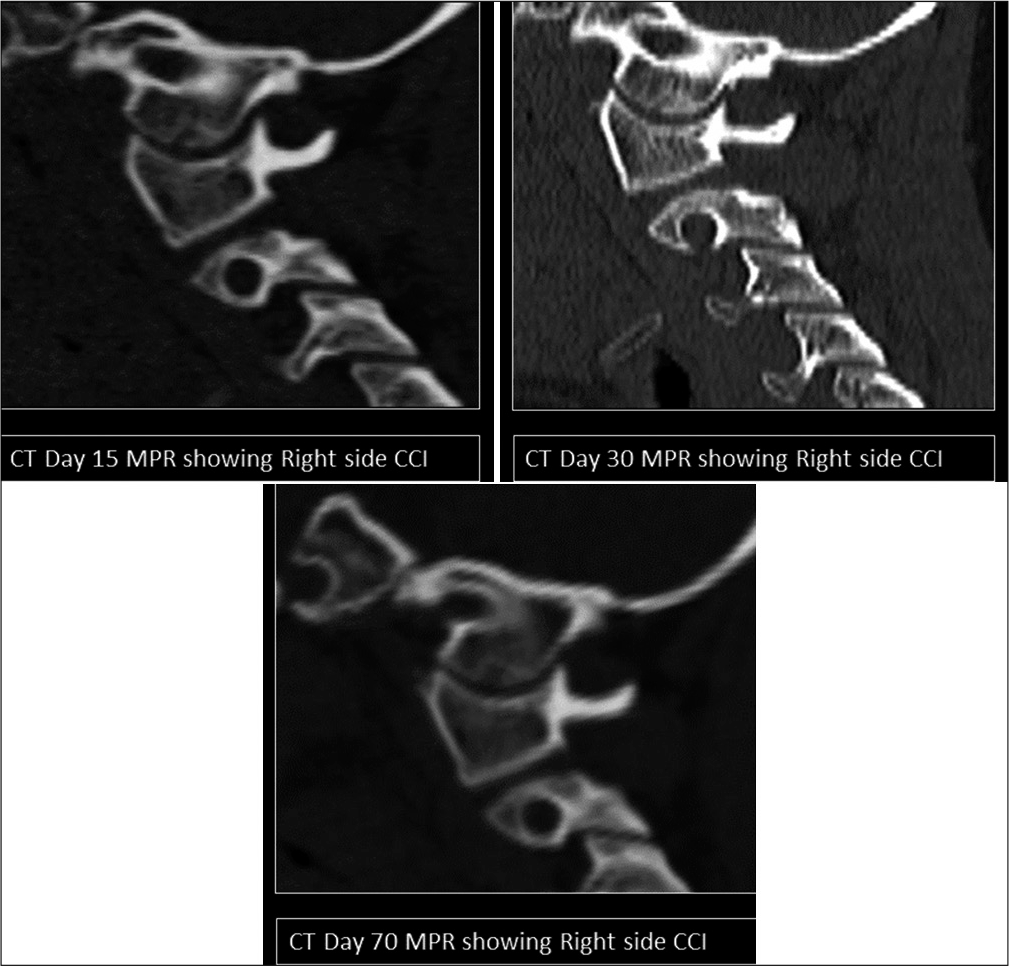
The pinless halo was kept on at all times for the next 3 months. The craniocervical junction alignment was monitored with weekly cervical spine X-rays and the noninvasive halo brace was reviewed weekly by orthotics. We also performed CT craniocervical junction to monitor the alignment and healing on day 15th day 30th, and day 70th [
During this 3-month period, the patient received regular physiotherapy, orthotics, and pain medicine input. He had an occipital laceration from the original trauma and this progressed to a pressure sore. This pressure sore was debrided and treated with IV antibiotics at 3 weeks postadmission. He developed worsening hydrocephalus on withdrawal of CSF drainage [
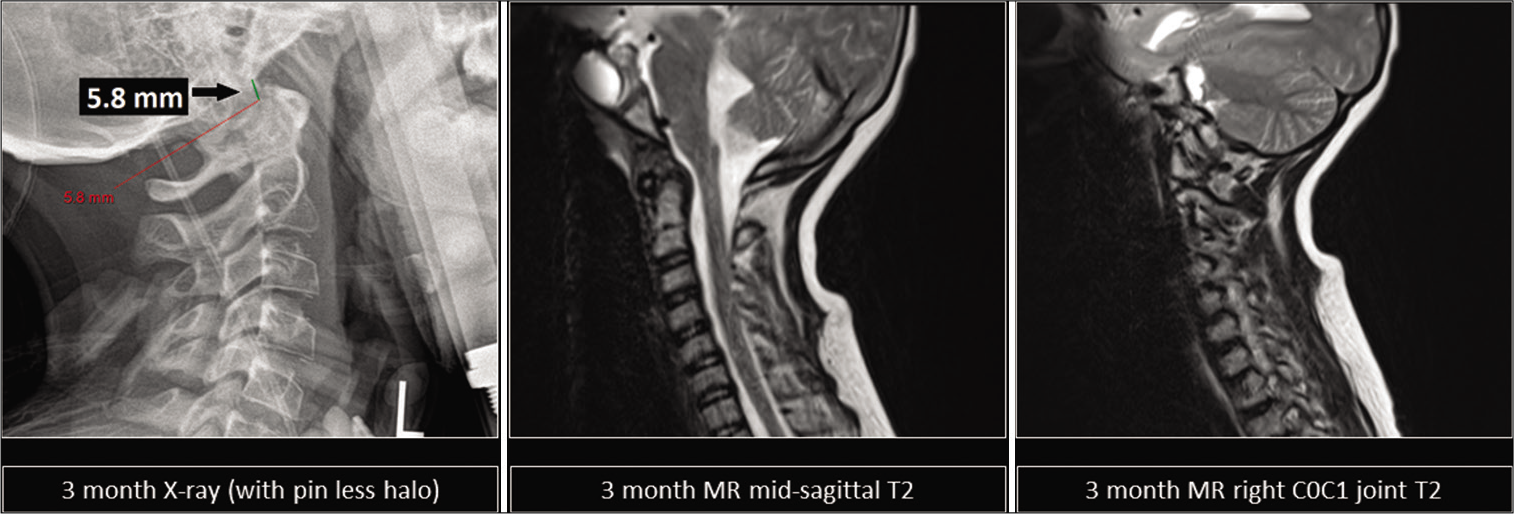
A follow-up MRI C-spine at 3 months from presentation confirmed resolution of the soft-tissue injury [
At the 2-year follow-up, he was noted to have made excellent recovery without any symptoms and signs of any spinal instability.
CONCLUSION
This report describes the successful management of traumatic AOD with a noninvasive halo. The case serves to illustrate that it is possible to gain sufficient stability with noninvasive halos in selected cases. The previous literature on pediatric traumatic craniocervical junction injury strongly advocates occipitocervical instrumented stabilization.[
The question of how to select patients for whom conservative strategy is appropriate is both difficult and as-of-yet unanswered.[
Horn et al. classified[
Steinmetz et al.[
Abel et al.[
For the patient described in our report, the decision to try a noninvasive halo was based on the consensus opinion of the pediatric neurosurgical team and their discussions with the parents. The tectorial membrane was intact on MR, suggesting an “incomplete” type AOD.[
There exist no cases to our knowledge which have made use of a noninvasive pinless halo in the context of traumatic AOD. AOD is a highly unstable craniocervical junction injury which can present with severe neck pain, lower cranial nerve palsies, spinal cord injury, and vascular injury (vertebral artery and carotid artery). Atlanto-occipital dislocation is commonly associated with traumatic brain injury,[
Several methods have been proposed for the radiological diagnosis of atlanto-occipital dislocation such as the Harris method using plain X-rays or the Condyle-C1 interval (CCI) on CT imaging. The Congress of Neurological Surgeons published a guideline in March 2013 which recommends using CT to determine the CCI method in pediatric patients with suspected AOD. This is also supported by other studies.[
However, in our patient, the index CT did not reveal any evidence of AOD. AOD was diagnosed on delayed CT and MR angiograms performed to investigate intracranial hemorrhage [
During the first 3 months, we monitored our patient’s craniocervical junction alignment with X-rays (on a weekly basis) and CT (at less frequent intervals). A further cervical spine X-ray with flexion-extension views was performed in the 4th month. Frequent clinicoradiological follow-up is very important factor in conservative management of AOD, as a patient may lose the reduction of the AOD despite halo immobilization.[
The conventional halo can be associated with significant adverse events: infection, pin loosening, dysphagia, dural/ skull penetration, and pressure ulcers.[
A multidisciplinary team input from a team of pediatric neurosurgeons, physiotherapists and occupational therapists, neuropsychologist, play therapist, speech therapist, and rehabilitation team leads to excellent clinical recovery in our case. Patient continues to remain asymptomatic on a 2-year follow-up. He mobilizes independently and attends mainstream school.
Pediatric patients with AOD and traumatic brain injury may require intense rehabilitation with input from physiotherapy, occupational therapy, and other therapists to address the child’s physical and psychological needs. We recommend that these patients are managed in a tertiary care center adapting a multidisciplinary approach lead by the pediatric neurosurgical team.
Noninvasive pinless halo is a potential treatment option for traumatic pediatric atlanto-occipital dislocation. This should be considered bearing in mind multiple factors including age and weight of the patient, severity of the atlanto-occipital dislocation (Grade I vs. Grade II and incomplete vs. complete), concomitant skull and scalp injury, and patient’s ability to tolerate the halo. It is vital to emphasize that this necessitates close clinicoradiological monitoring.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are very grateful to the patient and his parents, the orthotics team, occupational and physiotherapy departments, pediatric intensive care team, ward nursing staff, and the pediatric neurology team.
References
1. Abel TJ, Yan H, Canty M, Remick M, Dewan M, Witiw C. Traumatic atlanto-occipital dislocation in children: Is external immobilization an option?. Childs Nerv Syst. 2021. 37: 177-83
2. Abouelleil M, Siddique D, Dahdaleh N. Failure of the condyle-C1 interval method to diagnose atlanto-occipital dislocation in the presence of an associated atlanto-axial dislocation: A case report. Cureus. 2018. 10: 1-7
3. Astur N, Sawyer JR, Kelly DM, Warner WC, Klimo P, Muhlbauer MS. Traumatic atlanto-occipital dislocation in children. J Bone Jt Surg Am. 2013. 95: e194
4. Atlanto-Occipital T.editors. Textbook of Pediatric Neurosurgery. Switzerland: Springer; 2020. p. 2883-905
5. Bakhshi H, Kushare I, Banskota B, Nelson C, Dormans JP. Pinless halo in the pediatric population: Indications and complications. J Pediatr Orthop. 2015. 35: 374-8
6. Beez T, Brown J. Traumatic atlanto-occipital dislocation in children a case-based update on clinical characteristics, management and outcome. Childs Nerv Syst. 2017. 33: 27-33
7. Clifton W, Feindt A, Skarupa D, McLauchlin L, Tavanaiepour D, Rahmathulla G. Paradoxical distraction with upright position after halo fixation in 2 patients with atlanto-occipital dislocation. World Neurosurg. 2018. 110: 303-8
8. Hale AT, Say I, Shah S, Dewan MC, Anderson RC, Tomycz LD. Traumatic occipitocervical distraction injuries in children: A systematic review. Pediatr Neurosurg. 2019. 54: 75-84
9. Horn EM, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK, Theodore N. Survivors of occipitoatlantal dislocation injuries: Imaging and clinical correlates. J Neurosurg Spine. 2007. 6: 113-20
10. Hwang SW, Gressot LV, Chern JJ, Relyea K, Jea A. Complications of occipital screw placement for occipitocervical fusion in children. J Neurosurg Pediatr. 2012. 9: 586-93
11. Kimchi G, Greenberg G, Traynelis VC, Witiw CD, Knoller N, Harel R. Integrity of the tectorial membrane is a favorable prognostic factor in atlanto-occipital dislocation. Br J Neurosurg. 2020. 34: 470-4
12. McAllister A, Nagaraj U, Radhakrishnan R. Emergent imaging of pediatric cervical spine trauma. Emerg Radiol. 2020. 39: 1126-42
13. 14. Shekhar H, Yoong M, Mcphillips M, Kaliaperumal C. Stock car racing related cranio-cervical junction injury presenting with bilateral hypoglossal and abducens nerve palsy. Dev Med Child Neurol. 2015. 57: 19 15. Souslian FG, Patel PD, Elsherif MA. Atlanto-occipital dissociation in the setting of relatively normal radiologic findings. World Neurosurg. 2020. 143: 405-11 16. Steinmetz MP, Lechner RM, Anderson JS. Atlantooccipital dislocation in children: Presentation, diagnosis, and management. Neurosurg Focus. 2003. 14: ecp1